Atheromatous plaque in artery i.e., hardening of artery takes place in CAD which is a chronic condition where diameter of arterial lumen decreases due to which death can occur [1]. CVD is the leading cause of death in US and worldwide where atherosclerosis was considered as bland lipid storage [2]. The classical risk factors are raised LDL cholesterol levels, smoking, obesity, diabetes and sedentary life styles [1,3]. Now-a-days, it is known that a better mechanism is responsible for the initiation and development of atherosclerosis i.e., inflammation which plays an important role [4] having an autoimmune component [1]. In 1999 Russell Ross first published that atherosclerosis is an inflammatory disease [5]. Cytokines are important mediators of CVD [6] wherein plaque macrophages are the most important source of cytokine production r [7]. IL-1 is a pro-inflammatory glycoprotein and was the first cytokine discovered by Grey and Waksman in 1972 which is a lymphocyte activating factor having a molecular weight of 17 kDa with α and β isoforms [1,8,9]. It is involved in complex reactions of atherosclerosis with initiation of immune cells for plaque formation in arterial walls [4,10]. Increased levels of serum IL-1β have been reported in some studies of CVD [3,8].
Very few studies have been done so far regarding role of the serum concentration of IL-1β in CVD [3,8,11,12]. To our current knowledge this is the first study in Western Maharashtra population particularly in Mumbai city. This study was aimed to measure serum IL-1β level in different cardiac diseases. In addition we would like to ascertain a cut-off level of IL-1β to differentiate CVD patients from the normal population.
Materials and Methods
This was a case control study conducted at Cardiology and Medicine Department from Lokamanya Tilak Municipal General Hospital, Sion, Mumbai, India, from August 2015 to June 2016. In this study 229 cases of CVD’s (16 cases of complete heart block, one case of congenital heart disease, 22 cases of heart failure, 169 cases of myocardial infarction, one case of myocarditis and 20 cases of rheumatic heart disease) who were enrolled at Cardiology and Medicine Department along with 229 age and sex matched healthy controls. Sample size of 229 cases and 229 controls were obtained by consecutive sampling strategy undertaken for a period of 10 months. Based on the previous study of [8] interleukin values, sample size was estimated to be a minimum of 96 participants in each group for a type I error of 0.01 and type II error of 0.01. The following formula for sample size calculation was used.
n= (1+1/K) σ
where K= nA/nB is the matching ratio for cases and controls.
μA= mean of IL-1 among cases =4.4 pg/mL
μB= mean of IL-1 among controls =0.3 pg/mL
σ = standard deviation= 5.8 pg/mL
α = Type I error =0.01
β = Type II error =0.01.
The final sample size of 229 cases and controls each was thus included which satisfied the criteria laid for sample size calculation with the given Type I and Type II error values.
All the cases were diagnosed by cardiologists and final patient selection was done. Diagnostic test included 2D Echo along with electrocardiogram. The inclusion criteria were CVD patients undergoing hospitalization in Cardiology Intensive Care Unit and Medicine ward, who were willing to participate in the study and signed the informed consent. Patients with chronic illnesses such as malignancies, infections, rheumatoid arthritis (where the inflammatory markers are presumed to be raised) were excluded, The study protocol was approved by the institutional ethics committee. Informed consent was taken from all study subjects, both cases and controls after explaining the purpose of the study.
Venous blood was drawn in a plain tube without anticoagulant and centrifuged for 10 minutes at 2000 rpm at room temperature. Serum was separated in the screw type vials and stored at -40°C (BD Instruments). The serum IL-1β was measured by human IL-1β Enzyme-Linked Immunosorbent. Assay (ELISA) kits (Affymetrix, eBiosciences, San Diego, CA, USA) at Hinduridaysamrat Balasaheb Thackeray Municipal Medical College and Dr. RN Cooper General Hospital. This ELISA set is specifically engineered for accurate and precise measurement of protein levels from serum samples which recognises the cleaved mature form and uncleaved pro-form of Human IL-1β.
Statistical Analysis
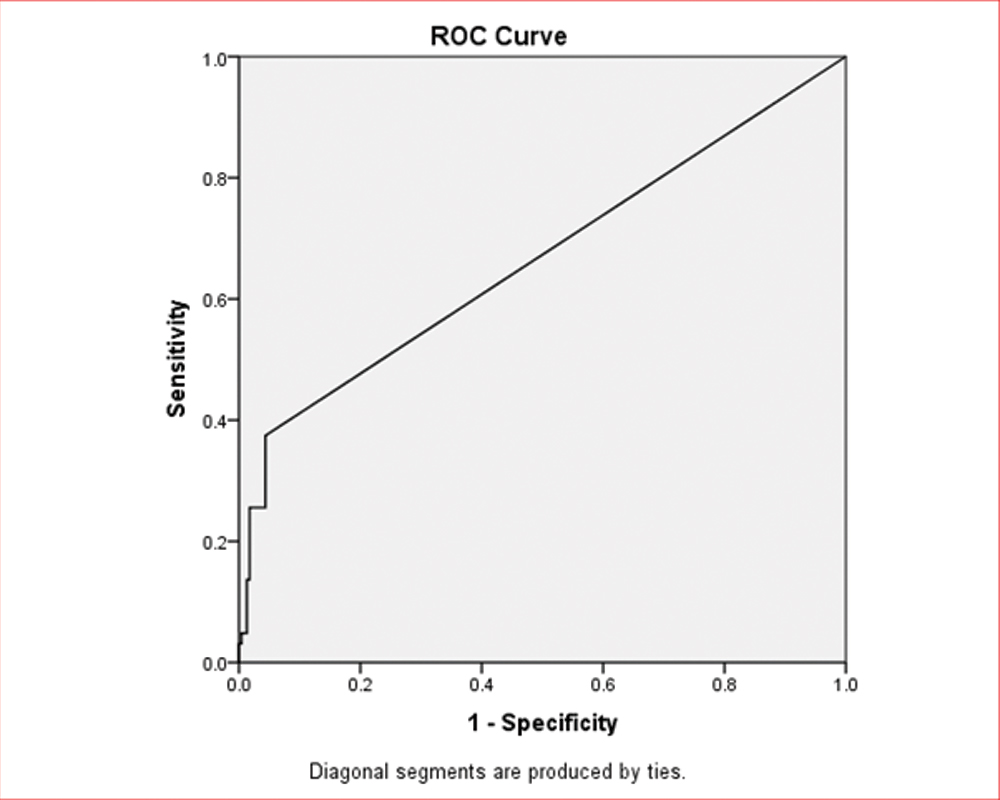
Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS) version 16.0 and Microsoft Excel 2007. Continuous data has been expressed as mean (Standard deviation) and median (Interquartile range) and categorical data is summarised as frequencies and percentages. The normality of the data was tested by Shapiro-Wilk test. As the data did not meet the assumption of normality, non-parametric tests were used. For IL-1β Mann-Whitney U test was applied. ROC Curve and Area Under the Curve (AUC) with 95% Confidence limits were generated for estimating the optimum cut-off of the diagnostic markers in terms of sensitivity and specificity to identify the best cut-off point for IL-1β. A p-value < 0.05 (2-tailed) was used to identify statistical significance. The optimum threshold of a diagnostic test in terms of sensitivity and specificity for determining the presence or absence of a condition of interest (in the present study, cardiac disease) has been mentioned as the cut-off value for the given diagnostic parameter.
Results
Significantly raised concentrations of serum IL-1β were seen in the CVD group compared to controls (p<0.0005). The calculated cut-off point for IL-1β in CVD samples to discriminate between the CVD patients and normal healthy condition in the study, was 2 pg/mL with a sensitivity of 37.4% and specificity 95.6%. The lower detection limit for serum IL-1β with the ELISA was 2 pg/mL.
Comparison of baseline characteristics and serum level of IL-1β between two groups is depicted in [Table/Fig-1].
Comparison of baseline characteristics and serum level of IL-1β between two groups.
| Parameters | Case (n=229) | Control (n=229) | p-value |
|---|
| Age (years) | 54.49±11.71 | 54.03±12.35 | 0.636 |
| Male | 161 (70.3) | 171 (74.7) | - |
| Female | 68 (29.7) | 58 (25.3) | - |
| Body Mass Index (kg/m2) | 24.43 (3.61) | 25.74 (3.19) | <0.0005 |
| Blood pressure Systolic (mmHg) | 122.97 (18.98) | _ | _ |
| Diastolic (mmHg) | 77.32 (11.32) | - | - |
| Diabetes mellitus | 30.1% | - | - |
| Hypertension | 42.8% | - | - |
| Previous myocardial infarction | 20.5% | - | - |
| Smoking | 24% | - | - |
| Tobacco | 37.1% | - | - |
| Alcohol | 17.5% | - | - |
| IL-1β pg/mL | Median (IQR) 0 (2.9) | Median (IQR) 0 (0) | <0.0005* |
| Minimum | Maximum | Minimum | Maximum |
| 0 | 111.4 | 0 | 9.7 |
*p-values < 0.05 (2-tailed) were used to identify statistical significance.
The analysis for IL-1β for ROC Curve was done with 458 observations [Table/Fig-2].
Receiver Operator Curve (ROC) for IL-1β.
The area under the curve for the ROC curve is 0.665 (95% CI 0.615-0.715)
Discussion
Cardiac biomarkers are substances released into the blood from a damaged or stressed heart and it is an important to measure for diagnosis and prognosis of cardiac disorders [13]. This study demonstrates the important role of IL-1β as a biomarker in the prediction of CVD. Serum levels of IL-1β were raised significantly in CVD cases {median (IQR) 0 (2.9) pg/mL} than the healthy age and sex matched controls {median (IQR) 0(0) pg/mL} (p<0.0005). This investigation also showed a high diagnostic value of IL-1β with an optimal cutoff point 2 pg/mL yielding a sensitivity of 37.4% and specificity of 95.6%. Cut-off point was determined by using ROC curve in order to minimise the false-negative and false-positive cases. On the other hand, measuring this inflammatory biomarker can be considered as a sensitive and highly specific test for predicting CVD. Generally IL-1β is not present in cells of healthy individuals which are a product of limited number of cells like blood monocytes, tissue macrophages and dendritic cells. Many cytokines like tumour necrosusis factor, IL-1α or IL-1β itself induces IL-1β transcription in autoinflammation [14]. Increased levels of serum IL-1β was reported in ischaemic heart disease by Hasdai D et al., [8]. Ikonomidis I et al., found raised serum IL-1β in patients with 3-vessel disease as compared to the patients with single- and two-vessel disease in the stable angina patients. They also found in a randomized, double-blind, placebo-controlled, crossover trial that the level of serum cytokines reduced after aspirin therapy [15]. Ozeren A et al., studied 37 patients with Unstable Angina Pectoris (UAP) (12 males and 25 females; mean age 57.5±9.7 years) within six hours of admission with 20 healthy age and sex matched controls. Serum IL-1β was measured in early phase, which was significantly increased in UAP patients [11]. Jing X et al., studied 163 CAD patients at different stages with 68 controls for IL-1β [3]. These authors found significantly higher levels of IL-1β in CAD patients than the controls, with no considerable difference among acute myocardial infarction, UAP and stable angina pectoris subgroups of CAD [3]. Study done by Patti G et al., showed that level of IL-1 receptor antagonists (a naturally occurring antagonist of the pro-inflammatory cytokine IL-1) significantly increased levels in unstable angina than stable angina patients {158 (110-224) pg/mL vs 108 (95-154) pg/mL, p= 0.002}, where IL-1Ra competitively blocks the binding of IL-1βb to IL-1 membrane receptors and counterbalances an augmented synthesis of IL-1 [16]. Amin studied serum IL-1β in 28 dyslipidaemic patients along with 16 healthy age and sex matched controls [17]. They found raised serum concentration of IL-1β compared to controls. The sensitivity, specificity and Area Under Curve (AUC) of IL-1β were 0.89, 0.75, and 0.84 respectively [17]. This study correlates with the above studies. Thus, the increased level is indicative of development of atherosclerosis. As IL-1β takes part in the regulation of vascular dysfunction, as its level increases in CVD’s, this contributes to the development of atherosclerosis. The reason may be due to impaired production of vasodilators like nitric oxide, which is known to be involved in atherosclerotic dysfunction [8]. IL-1β controls the nitric oxide production by inducing nitric oxide synthase which is involved in formation of nitric oxide. It also induces guanylate cyclase and increases concentration of c-GMP which is a relaxing factor and also helps in production of C-type natriuretic peptide which works as a vasodilator [8]. Another reason is that IL-1β induces IL-6 production which ultimately increases gene expression for clotting factors and inhibitors of fibrinolysis and which also contribute to transendothelial passage of neutrophils by increasing surface expression of endothelial adhesion molecules and which leads to IL-8 production [18]. Atherogenic risk factors such as oxidised low density lipoprotein, viral infection and several cytokines may induce endothelial for macrophage colony stimulating factor production which further stimulates IL-1β production. This IL-1β enhances cholesterol uptake from human macrophages by up regulating of their oxidized LDL receptors resulting in foam cell formation. IL-1β is released by injured endothelium which promotes interaction of endothelial cells with circulating leukocytes. This further contributes to development and progression of atherosclerosis [15]. It is likely that cytokines do not cause heart failure, but it’s over expression leads to progression and severity of heart failure. These cytokines not only have effect on myocardial infarction but it is also responsible for myocardial remodeling [19]. Thus, IL-1β is responsible for plaque rupture which leads to acute coronary syndrome which may be due to ischemia and reperfusion. Considering the above mechanism it was necessary to evaluate serum IL-1β for detecting CVD patients. However, in another study Shubair MK et al., found decreased serum IL-1β concentrations in CHD patients compared to controls in Sudanese population [20]. Further research with therapeutic approach is recommended.
Limitation
Even though present study is with 458 samples, quite a few limitations of these data should be taken into account. The present study lacks the follow-up. Long term follow-up are necessary which would have provided additional important information of IL-1β for risk stratification and prognosis.
Conclusion
The inflammatory marker, serum IL-1β (measured by ELISA which is relatively cost-effective assay) is a potentially useful marker for evaluation of CVD and can be included as a diagnostic marker along with other proven markers. It plays an important role in atherogenesis which further leads to CVDs. Thus, the serum IL-1β is detected as an important biomarker for better diagnosis of CVDs.
*p-values < 0.05 (2-tailed) were used to identify statistical significance.