This case report aims to share the successful management of Epithelial Downgrowth (ED) which occurred following persistent wound leak, after Removal of Silicone Oil (ROSO) via the anterior chamber. A teenage male with history of high myopia underwent bilateral phacoemulsification and implantation of Multifocal Intraocular Lens (MFIOLs). Four months later, he complained of left eye floaters and blurring of vision. Fundus showed left vitreous haemorrhage with lens subluxation. Left 23 gauge pars plana vitrectomy revealed multiple retinal tears. Endolaser and gas injection with MFIOL repositioning was done. Retinal redetachment and MFIOL subluxation occurred six weeks postoperatively. Revision vitrectomy with silicone oil and explantation of MFIOL was performed rendering left eye aphakic. Four months later, he underwent ROSO via a superior corneal incision. Positive Seidels was seen two weeks post-ROSO and resuturing was performed. Unfortunately, advancing ED was noted at the superior cornea. One month after ROSO, scleral fixated IOL implantation with manual removal of ED and intracameral injection of 5-fluorouracil (5-FU) were performed. Twelve months postoperatively, cornea remained clear with a pinhole vision of 6/7.5 and retina was flat. In conclusion, wound leak after ROSO via the anterior chamber in aphakic individuals may predispose to ED. Key to treatment of this sight threatening condition is thoughtful anterior segment examination. Manual removal of the membrane combined with 5-FU injection during secondary lens implantation surgery is an effective treatment.
Case Report
A 16-year-old male with history of high myopia underwent bilateral phacoemulsification and implantation of MFIOL. Four months later he complained of left eye floaters and reduced vision. Fundus showed left eye vitreous haemorrhage with lens subluxation. Left 23 Gauge pars plana vitrectomy revealed multiple retinal tears. Endolaser and gas injection with MFIOL repositioning into the sulcus was done. Retinal redetachment and MFIOL subluxation was noted six weeks postoperatively. Revision vitrectomy with silicone oil injection and explantation of MFIOL was performed rendering the left eye aphakic. This was performed to remove the subluxated lens and allow trimming of the anterior vitreous to reduce risk of anterior proliferative vitreoretinopathy.
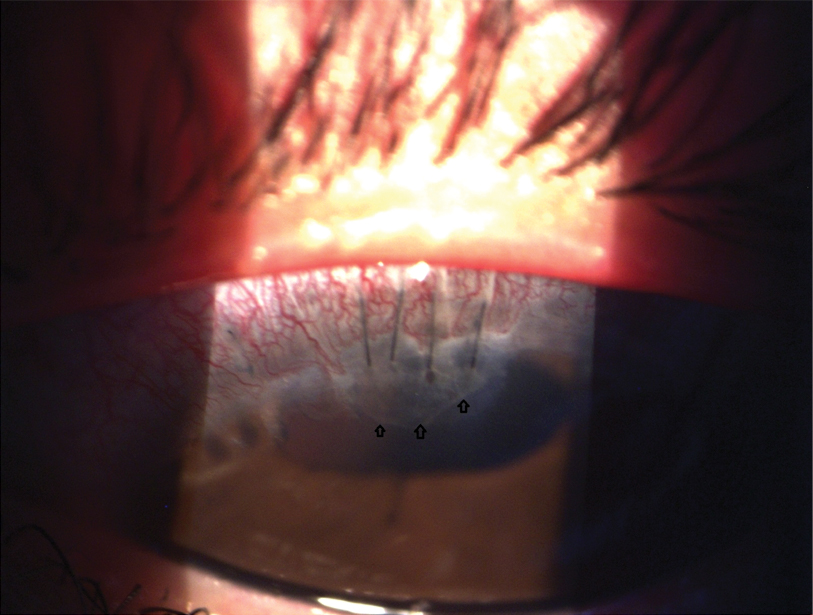
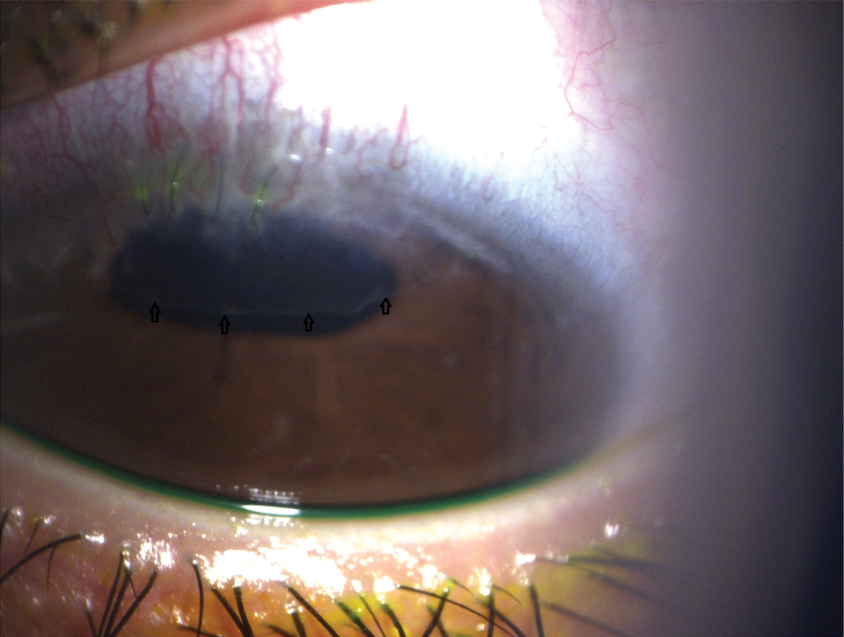
Four months later, he underwent ROSO via a superior corneal incision created with 2.4 mm Clearcut slit knife (Alcon Ophthalmics). Infusion was achieved using a 20G Lewicky anterior chamber maintainer (Storz Ophthalmics) placed at the inferior temporal limbus. Positive Seidels was seen two weeks post-ROSO and resuturing was performed. Unfortunately, an advancing epithelial membrane was noted at the superior cornea [Table/Fig-1]. This progressed rapidly over the course of two months which suggested this was ED [Table/Fig-2]. The intraocular pressure was normal and he was otherwise asymptomatic.
Anterior segment photograph taken with the patient looking down showing a well demarcated edge of epithelial downgrowth with scalloped edges (arrows) one month post resuturing for wound leak after silicone oil removal (ROSO) measuring about 1.2 mm from the limbus. There is injection of the adjacent conjunctiva and nylon sutures placed at the superior limbus.
Anterior segment photograph taken with patient on downgaze at 2 months post resuturing showed a rapidly advancing edge measuring 2.1 mm from the limbus (arrows). The nylon sutures have become loose and collected mucus. These were removed in the subsequent surgery.
The anterior segment surgeon performed standard scleral fixated intraocular lens (Model CZ70BD, Alcon Laboratories, Inc., USA) implantation first followed by removal of the ED and injection of 5-FU into the anterior chamber under general anaesthesia. Removal of the ED was performed using Rosenwasser Irrigating Endothelial Stripper (Katena catalogue no. K7-5897, USA) [Table/Fig-3] and reversed sinskey hook (Katena catalogue no. K3-5002), USA) [Table/Fig-4] with viscoelastic filling the anterior chamber until all visible membrane was removed from the superior cornea. The superior incision was then sutured with nylon 10/0. The 5-FU was given at concentration of 1 mg/0.1 mL of ViscoatTM (Alcon laboratories, USA) as per the study done by Ni N et al., [1].
Rosenwasser Irrigating Endothelial Stripper (Katena, USA).

Reversed sinskey hook (Katena, USA)

The mixture of 5-FU in viscoelastic was carefully injected at the area where the epithelial membrane was removed in order to avoid dissemination of the antimetabolite.
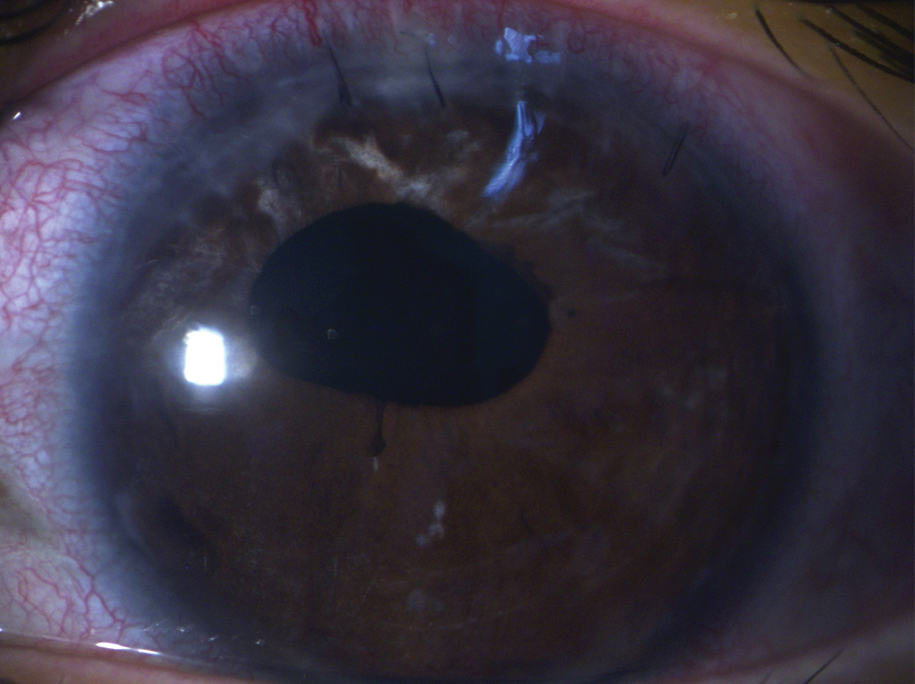
The patient had an uneventful recovery with no obvious increased signs of toxicity or inflammation to adjacent structures. At four months there was no membrane recurrence [Table/Fig-5]. The intraocular pressure remained normal. Twelve months postoperatively the cornea was clear even in the area of removal and best corrected visual acuity was 6/7.5, N10. The retina remained flat.
Four months after the final surgery, the superior cornea clarity allows superior iris atrophy to be visible with clear central cornea. The pupil irregularity was a result of the lens explantation in patient’s earlier surgery.
Discussion
This retrospective case report is interesting because it illustrates an anterior complication of an initially posterior surgical problem. It also reiterates an effective method for early surgical and medical eradication of ED.
The rate of ED is very low at 0.08% following surgeries for cataract. A higher rate is observed at 0.25% following corneal transplants [2]. ED occurs when there is advancing growth of epithelial cells presumably from the ocular surface, usually the cornea, into intraocular structures through a breach in the ocular surface. It forms a cyst or sheet of cells akin to surface epithelial cells. There is a tendency for these cells to multiply and migrate uncontrollably. They also seem to cause underlying structures to become disorganised [3].
ED has been reported to occur following various types of ocular surgery including phacoemulsification [4], descemet stripping automated endothelial keratoplasty [1], penetrating keratoplasty [2] and clear corneal cataract surgery [5]. It has also been seen following glaucoma surgery and penetrating trauma [6].
Risk factors include multiple procedures, invasive surgery including keratoprosthesis [7], impaired wound healing especially if there is a leakage or wound fistula, iris or vitreous prolapse to the wound [4] and ocular inflammation.
Diagnosis of ED is made clinically by the observation of a translucent layer or membrane with a clearly defined border that covers the cornea internally or coats the iris, adjacent to the surgical wound [3], in the early stages. Over time, this edge can be seen to advance rapidly over a period of weeks, in contrast to fibrous ingrowth which tends to be slower.
The outcomes of treatment are variable and generally unsatisfactory with no clear treatment guidelines [1-5]. The available treatments include surgical excision of the invading epithelium using a large en bloc excision together with penetrating corneoscleral graft [4], cryotherapy to the affected surface including the posterior cornea, trabecular meshwork or iris [6]. Cryotherapy to the cornea has been typically unsatisfactory with many patients requiring corneal graft later due to decompensation of the cornea [6].
The high failure rate and devastating outcome of unsuccessfully treated ED by surgical excision alone has prompted surgeons to seek a better treatment and adjunct. The usage of antimetabolites such as 5-FU was proposed first by Weiner MJ in 1989 as a non surgical method and as an adjunct treatment [3]. The 5-FU is selected due to its effect mainly on dividing cells while sparing adjacent structures. Studies have shown its safety for intraocular use at selected concentrations [3].
Nonetheless, usage of 5-FU also had mixed success in patients with corneal graft and clear cornea cataract surgery [1,5,8].
The sequelae of ED are notably serious with majority of treated patients having permanent loss of vision [6]. This is largely due to corneal oedema or intractable glaucoma when the ED grows over the trabecular meshwork.
The cause of ED in this case was most likely to have been multifactorial. Risk factors included multiple surgeries through the same corneal wound and wound leaking that the patient experienced after the removal of oil [3]. The persistent wound leak would have allowed surface corneal epithelial cells to migrate through the open wound. There would also have been increased inflammation in a young patient such as this as shown by the injected wound in [Table/Fig-2]. This is an example of misguided healing process.
ROSO via the anterior chamber is a commonly performed procedure by posterior segment surgeons in aphakic individuals. Removal is straight forward and does not require the placement of pars plana infusions but rather an anterior chamber maintainer. This is limited to removal of light silicone oil of 1000 and 5000 centistokes and is not suitable for heavy oil or heavy liquid removal procedures. Till date, ED has not been described following ROSO via an anterior approach.
The good outcome in this case was due to early detection before the advancement towards the central cornea. In the early stages, an advancing edge of ED could have been mistaken for corneal wound scarring. The hallmark of ED diagnosis was rapid advancement of the edge. This was captured by anterior segment photography, allowing clear comparison [Table/Fig-1,2].
Alternatively, careful clinical measurements and recording in the notes would also have aided the diagnosis as well as close follow-up. Another feature to support a diagnosis of ED is the whitish burns seen with use of Argon laser on the membrane [1]. However, this was not needed due to the rapid clinical progression and history of surgery in this patient. Other diagnostic measures include aqueous aspiration for cytology which will show cells of epidermal origin [1].
Diagnosis of ED is often made late when patients present with worsening vision, redness and pain usually within one year of surgery [3]. Mean onset is five months. However, it can occur as early as two weeks like in present case or many years later [3]. This is because patients are asymptomatic at onset of ED. The signs can be subtle if the ophthalmologist is not aware of the condition. Trainees in particular may misinterpret the sign as scarring due to the similarity in appearance. In advanced cases, despite radical surgery, the prognosis remains poor. Thus, the decision to treat is influenced by the visual potential, status of fellow eye among others.
Management in early cases can be less invasive and have a better outcome as shown in this case. The main complication of advanced ED is intractable glaucoma that could lead to enucleation. The usage of 5-FU offers a non surgical approach to ED however in practice, given the aggressive nature of the condition, surgeons will more likely prefer an excisional approach if there is a visible membrane or cyst. This case illustrates, the good cornea clarity that combination of excision with 5-FU, was able to achieve. This case also illustrates successful use of single dose of 5-FU in combination with viscoelastic in treating early ED as an adjunct to surgical removal, unlike the two or more doses used in other case reports [1,5,8]. This case also highlights the use of 1 mg/0.1 mL of intracameral 5-FU mixed with viscoelastic to deliver the drug directly to affected tissues.
The treatment is surgical and more extensive the ED is, the more radical the excision needs to be. The key therefore is early intervention before the condition becomes advanced.
Conclusion
Wound leak after ROSO via the anterior chamber in aphakic individuals may predispose to ED. The key to treatment of this sight threatening condition after ROSO is thoughtful anterior segment examination. Manual removal of the membrane combined with 5-FU injection during secondary lens implantation surgery is an effective treatment.
[1]. Ni N, Goldberg MA, Eagle Jr. RC, Rapuano CJ, Haller JA, Epithelial downgrowth after intraocular surgery treated with intracameral 5-fluorouracilCase Rep Ophthalmol Med 2015 2015:32548510.1155/2015/32548526106497 [Google Scholar] [CrossRef] [PubMed]
[2]. Sugar A, Meyer RF, Hood CI, Epithelial downgrowth following penetrating keratoplasty in the aphakeArch Ophthalmol 1977 95(3):464-67.10.1001/archopht.1977.04450030106015320971 [Google Scholar] [CrossRef] [PubMed]
[3]. Weiner MJ, Trentacoste J, Pon DM, Albert DM, Epithelial downgrowth: a 30-year clinicopathological reviewBr J Ophthalmol 1989 73:06-11.10.1136/bjo.73.1.62920156 [Google Scholar] [CrossRef] [PubMed]
[4]. Vargas LG, Vroman DT, Solomon KD, Holzer MP, Escobar-Gomez M, Schmidbauer JM, Epithelial downgrowth after clear cornea phacoemulsification: report of two cases and review of the literatureOphthalmology 2002 109(12):2331-35.10.1016/S0161-6420(02)01274-5 [Google Scholar] [CrossRef]
[5]. Tomlins PJ, Savant V, Quinlan M, Failure of intracameral fluorouracil to resolve an epithelial ingrowth following clear corneal cataract surgeryJ Cataract Refract Surg 2007 33(5):923-924.10.1016/j.jcrs.2007.01.02617466875 [Google Scholar] [CrossRef] [PubMed]
[6]. Rachitskaya AV, Dubovy SR, Hussain RM, Perez VL, Alfonso EC, Berrocal AM, Epithelial downgrowth in the vitreous cavity and on the retina in enucleated specimens and in eyes with visual potentialRetina 2015 35(8):1688-95.10.1097/IAE.000000000000049525768250 [Google Scholar] [CrossRef] [PubMed]
[7]. Chen HS, Pineda R, Epithelial and fibrous downgrowth: mechanisms of diseaseOphthalmol Clin North Am 2002 15(1):41-48.10.1016/S0896-1549(01)00013-X [Google Scholar] [CrossRef]
[8]. Lattanzio FA Jr, Sheppard JD Jr, Allen RC, Baynham S, Samuel P, Samudre S, Do injections of 5-fluorouracil after trabeculectomy have toxic effects on the anterior segment?J Ocul Pharmacol Ther 2005 21(3):223-35.10.1089/jop.2005.21.22315969640 [Google Scholar] [CrossRef] [PubMed]