Childhood Bezoars: A Case Series
Kamal Nain Rattan1, Rashmi Hooda2, Shalu Ogha3, Ahmad Khursheed4, Aashima5
1 Professor and Head, Department of Pediatric Surgery, Pt. BDS Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
2 Senior Resident, Department of Pediatrics, Pt. BDS Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
3 Junior Resident, Department of Pediatrics, Pt. BDS Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
4 Junior Resident, Department of Pediatrics, Pt. BDS Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
5 Junior Resident, Department of Pediatrics, Pt. BDS Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rashmi Hooda, 7/11 J, PGIMS Campus, Rohtak, Haryana, India.
E-mail: rashmihooda112@gmail.com
Bezoars are the rarest causes of upper abdominal masses and upper gastric outlet obstruction in children and are most commonly seen in females of adolescent age. They can present with the common symptoms of abdominal mass or abdominal pain but may lead to serious complications as well. They must be diagnosed and managed early despite their rarity so as to prevent complications like obstruction, perforation and bleeding. This article is reporting our 25 years experience with abdominal bezoars with variable presentation in our tertiary care centre.
Phytobezoar, Rapunzel syndrome, Trichobezoar
Bezoars can be classified according to their components into phytobezoars (vegetable matter), trichobezoars (hair), and pharmacobezoar (medications), lactobezoars (milk). Trichobezoars are usually associated with trichotillomania, characterised by compulsive pulling of hair followed by eating of the same (trichophagia). This condition was first described by Baudamant in 1779 [1]. They are mostly found in stomach, but can also extend into the duodenum and jejunum, a condition known as Rapunzel syndrome, the rarest type of bezoar. This was first described in the literature by Vaughan ED et al., [2].
Case Series
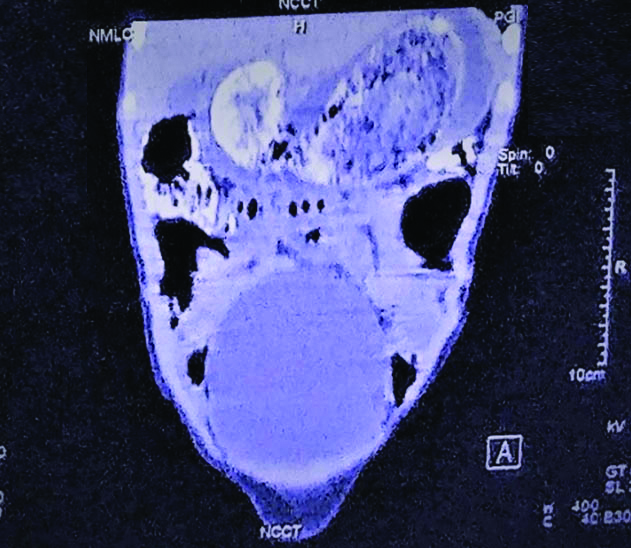
During the study period of 25 years from 1991 to 2016, we had 5 gastric bezoars, 3 intestinal bezoars and 3 rapunzels [Table/Fig-1]. These are described in [Table/Fig-2]. All intestinal bezoars were present in males. Two of them were trichobezoars and one was a phytobezoar. One child with intestinal trichobezoar presented with intestinal perforation and peritonitis, expired in the post-operative period due to sepsis and disseminated intravascular coagulopathy. The most common mode of presentation of gastric bezoars was abdominal lump with upper gastric outlet obstruction, while the intestinal bezoars presented with acute intestinal obstruction. All of them presented with the common symptoms of weight loss, loss of appetite and history of trichotillomania and trichophagia, loss of scalp hair since last 3-4 years. The symptoms were associated with psychiatric illness characterised by depression and anxiety only in 2 out of 11 cases. The diagnosis was made with the help of X-ray abdomen, abdominal ultrasound and Computerized Tomography (CT) scan of abdomen to confirm the diagnosis [Table/Fig-3]. Barium meal follow through was done in cases of lower gastrointestinal obstruction.
Rapunzel causing ileal obstruction in a four-year-old male child.

Summary of 11 cases of bezoars.
| Patient | Age (years) | Gender | Presenting complaints | Type of bezoar | Extent | Surgical procedure | Postoperative complications | Psychiatric manifestations |
|---|
| 1 | 4 | M | Intestinal perforation, peritonitis, severe wasting | Trichobezoar | Intestinal | Enterotomy, gut resection, end to end anastomosis | Expired | -- |
| 2 | 6 | M | Lower GI obstruction, mass, weight loss | Trichobezoar | Intestinal | Enterotomy, resection and end to end anastomosis | none | Absent |
| 3 | 7 | M | Lower GI obstruction, mass, weight loss | Phytobezoar | Intestinal | Enterotomy, resection and end to end anastomosis | none | Absent |
| 4 | 10 | F | Abdominal lump, weight loss, trichotillomania, trichophagia | Trichobezoar | gastric | Gastrotomy | none | Absent |
| 5 | 14 | F | Abdominal lump, Upper GI obstruction, weight loss, trichotillomania, trichophagia | Trichobezoar | Gastric | Gastrotomy | None | Absent |
| 6 | 13 | F | Abdominal lump, Upper GI obstruction, weight loss, trichophagia | Trichobezoar | gastric | gastrotomy | none | Anxiety, depression |
| 7 | 14 | F | Abdominal lump, weight loss, loss of scalp hair | Trichobezoar | Gastric | Gastrotomy | none | Absent |
| 8 | 16 | F | Abdominal lump, vomiting, upper GI obstruction, loss of scalp hair | Trichobezoar | Gastric | gastrotomy | none | Anxiety, depression |
| 9 | 15 | F | Abdominal lump, weight loss, trichotillomania, trichophagia | Trichobezoar | rapunzel | Enterotomy | None | Absent |
| 10 | 14 | F | Abdominal lump, weight loss, Upper GI obstruction | Trichobezoar | rapunzel | Enterotomy | None | Absent |
| 11 | 15 | F | Pain abdomen, abdominal lump weight loss, upper GI obstruction | Trichobezoar | rapunzel | Enterotomy | None | Absent |
CECT abdomen: non-adherent spindle shaped mass in the stomach, with the contrast surrounding, coating and infiltrating trichobezoar with extension into duodenum.
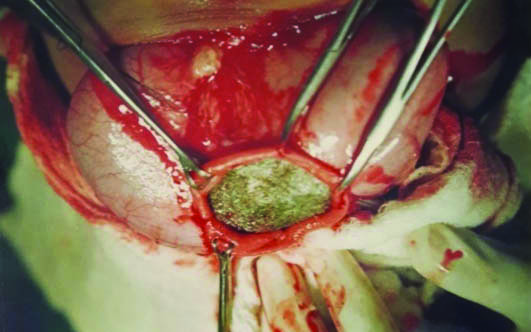
All the cases were managed with exploratory laparotomy. The gastric bezoars were removed through gastrotomy [Table/Fig-4]. The intestinal bezoars were removed by enterotomy and resection and end to end anastomosis, as there was associated perforation in one case and unhealthy looking gut in others. Feeds were started on post-operative day 3 in most of the cases after the return of bowel sounds and passage of stools. All the cases were referred for psychiatry follow-up to avoid further recurrence.
Pre-operative photograph of large gastric bezoar.
Discussion
The origin of the word ‘Bezoar’ stems from a Persian word ‘Badzehr’ with literal meaning of ‘antidote’. It was regarded as a stone capable of curing any kind of poison, which was later found to be a misconception. It was called a stony concretion in late 15th century, found in the gastrointestinal tracts of certain animals. The hair in the stomach escapes digestion and gets entrapped in the gastric mucosal folds, escaping peristalsis as well. They get coated by gastric mucus and get denatured by gastric acid resulting in their black and shiny appearance. The continued ingestion of hair leads to their accumulation in the stomach, with the bezoar assuming the oblong shape of the stomach [3]. Due to large capacity of the stomach, it takes long time of about 3-4 years for the bezoar to assume sufficiently large size to present as abdominal lump or obstruction. The complications include gastric outlet obstruction [4], gastric ulcer and gastric perforation [5], intestinal obstruction, peritonitis [6,7], intussusception, pancreatitis, obstructive jaundice/cholangitis and death [8].
They may extend further to a variable extent into the jejunum, resulting in Rapunzel syndrome. There, the tip may get adhered to the jejunal wall at solitary or multiple sites, or it may lie free. They may primarily form in the intestine or get detached from the gastric bezoar to lodge into the intestine and cause obstructive symptoms [2]. The clinical manifestations depend on the site and size of the bezoar.
Contrary to the available literature, with females below 20 years of age forming 90% of the cases with trichobezoars [9], the occurrence of bezoars in males was around 27% in our institute. But all of them were intestinal bezoars. The psychiatric abnormality was present in only two out of the 11 cases. Trichobezoars are commonly associated with history of trichotillomania and trichophagia, but few cases have been described without the association with trichotillomania [10]. Fatality has been reported in 3 out of 49 cases of Rapunzel in a review by Kim SC et al., [11]. The diagnosis can be made with the help of ultrasonography or CT scan of abdomen. Findings on ultrasound include hyperechoic band-like lesions and CT scan shows intraluminal mass with bubbly gaseous lucencies. Abdominal radiographs after barium contrast may be required in some cases. They demonstrate a filling defect outlining the bezoar with air entrapped in it. The diagnosis can also be confirmed by endoscopy which can also be used for removal of the mass if it is small.
The management of bezoars depends on the site and the size of the bezoar. For large gastric bezoars and Rapunzel syndrome, treatment of choice is surgical removal through gastrotomy. In Rapunzel syndrome, if the tail is free, only gastrotomy is indicated. But, if the tail is adherent to jejunum at solitary or multiple sites, then solitary or multiple jejunotomies are required. The tail should be pulled gently; otherwise forceful extraction may result in jejunal perforation [7]. For small bezoars, endoscopic or laparoscopic removal may be tried. Coca cola has also been used to fragment the phytobezoars, which can then be removed endoscopically [12]. The mechanisms proposed are mucolytic effects of sodium bicarbonate, and the acidifying effects of carbonic and phosphoric acid present in diet coke. Dissolution of trichobezoars with papain, cellulose or acetylcysteine has largely been unsuccessful [13]. A literature review by Al-Janabi IS et al., found laparotomy as the best and most effective methods for management of the bezoars [14]. The laparoscopy and endoscopy being reported as unsuccessful in most of the case reports, while laparotomy followed by gastrotomy was associated with a success rate of around 99% [8,10,15]. But, the advantage of endoscopy and laparoscopic removal is that it is non-invasive, while laparotomy with surgical removal is associated with various complications, like wound infection.
The further management is necessary in order to avoid further recurrences. Upto 20% of the patients can have recurrent bezoars [16]. This can be minimized by prompt psychiatric referral and follow-up. We referred all our patients for psychiatry follow-up.
Conclusion
A high index of suspicion is necessary for diagnosis. Trichobezoars should be suspected in the cases presenting with weight loss, abdominal pain or abdominal lump. The best method of management is laparotomy or gastrotomy. Recurrences can be minimized by appropriate psychiatry follow-up.
[1]. Baudamant M, Description de deux masses de cheveux trouvee dans l’estomac et les intestines d’un jeune garcon age de seize ansHist Soc Roy Med, Paris 1777-1779 2:262-63. [Google Scholar]
[2]. Vaughan ED Jr, Sawyers JL, Scott HW Jr, The Rapunzel syndrome. An unusual complication of intestinal bezoarSurgery 1968 63:339-43. [Google Scholar]
[3]. Williams RS, The fascinating history of bezoarsMed J Aust 1986 145:613-614.10.5694/j.1326-5377.1986.tb139511.x3540541 [Google Scholar] [CrossRef] [PubMed]
[4]. Couceiro A, Viveiro C, Capelão G, Nobre J, Laureano M, Gonçalves I, A Rare Cause of Abdominal Mass and Gastric Outlet ObstructionGE Port J Gastroenterol 2016 23:50-53.10.1016/j.jpge.2015.08.00328868431 [Google Scholar] [CrossRef] [PubMed]
[5]. Mohite PN, Gohil AB, Wala HB, Vaza MA, Rapunzel syndrome complicated with gastric perforation diagnosed on operation tableJ Gastrointest Surg 2008 12:2240-42.10.1007/s11605-007-0460-018172606 [Google Scholar] [CrossRef] [PubMed]
[6]. Singla SL, Rattan KN, Kaushik N, Pandit SK, Rapunzel syndrome- a case reportAm J Gastroenterol 1999 94:1970-71.10.1111/j.1572-0241.1999.01243.x10406272 [Google Scholar] [CrossRef] [PubMed]
[7]. Rattan KN, Yadav V, Yadav V, Singh J, Ileal trichobezoar presenting as intestinal obstruction and peritonitisAPSP J Case Rep 2017 8:1110.21699/ajcr.v8i2.54928401038 [Google Scholar] [CrossRef] [PubMed]
[8]. Gorter RR, Kneepkens CM, Mattens EC, Aronson DC, Heij HA, Management of trichobezoar: case report and literature reviewPediatr Surg Int 2010 26:457-63.10.1007/s00383-010-2570-020213124 [Google Scholar] [CrossRef] [PubMed]
[9]. Andrus CH, Ponsky JL, Bezoars: classification, pathophysiology, and treatmentAm J Gastroenterol 1988 83:476-78. [Google Scholar]
[10]. Tiago S, Nuno M, João A, Carla V, Gonçalo M, Joana N, Trichophagia and trichobezoar: case reportClin Pract Epidemiol Ment Health 2012 8:43-45.10.2174/174501790120801004322675398 [Google Scholar] [CrossRef] [PubMed]
[11]. Kim SC, Kim SH, Kim SJ, A case report: large trichobezoar causing rapunzel syndromeMedicine 2016 95:e374510.1097/MD.000000000000374527258502 [Google Scholar] [CrossRef] [PubMed]
[12]. Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatmentAliment Pharmacol Ther 2013 37:169-73.10.1111/apt.1214123252775 [Google Scholar] [CrossRef] [PubMed]
[13]. Coulter R, Anthony MT, Bhuta P, Memon MA, Large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literatureSouth Med J 2005 98:1042-44.10.1097/01.smj.0000182175.55032.4a16295823 [Google Scholar] [CrossRef] [PubMed]
[14]. Al-Janabi IS, Al-Sharbaty MA, Al-Sharbati MM, Al-Sharifi LA, Ouhtit A, Unusual trichobezoar of the stomach and the intestine: a case reportJ Med Case Rep 2014 8:7910.1186/1752-1947-8-7924580892 [Google Scholar] [CrossRef] [PubMed]
[15]. Pogorelic Z, Juric I, Zitko V, Britvić-Pavlov S, Biocić M, Unusual cause of palpable mass in upper abdomen-giant gastric trichobezoar: report of a caseActa Chir Belg 2012 112:160-63.10.1080/00015458.2012.1168081622571081 [Google Scholar] [CrossRef] [PubMed]
[16]. Robles R, Parrilla P, Escamilla C, Lujan JA, Torralba JA, Liron R, Gastrointestinal bezoarsBr J Surg 1994 81:1000-01.10.1002/bjs.18008107237922045 [Google Scholar] [CrossRef] [PubMed]