Serum Lipoprotein (a) as a Diagnostic Marker of Coronary Artery Disease: A Case-Control Study
M.M. Kavitha1, Jeevan G. Ambekar2, Sangappa V. Kashinakunti3, Nilima Dongre4
1 PhD Scholar, Department of Biochemistry, Shri B.M. Patil Medical college, Hospital Research Centre, BLDE Deemed to be University, Vijayapura, Karnataka, India.
2 Professor, Department of Biochemistry, Shri B.M. Patil Medical College, Hospital Research Centre, BLDE Deemed to be University, Vijayapura, Karnataka, India.
3 Professor, Department of Biochemistry, S. Nijalingappa Medical College and Hanagal Sri Kumareshwara Hospital and Research Centre, Bagalkot, Karnataka, India.
4 Associate Professor, Department of Biochemistry, Shri B.M. Patil Medical College, Hospital Research Centre, BLDE Deemed to be University, Vijayapura, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. M.M. Kavitha, Department of Biochemistry, B.M. Patil Medical College, BLDE Deemed to be University, Vijayapura-586103, Karnataka, India.
E-mail: mekch@rediffmail.com
Introduction
Coronary Artery Disease (CAD) is a major cause of mortality in India. Conventional risk factors fail to explain the increasing burden of CAD, thus necessitating to search for newer risk factors like Lipoprotein (a) {Lp(a)}. Lp(a) is considered as one of the risk marker of CAD. Lp(a) levels have shown wide ethnic variation among human population.
Aim
The study was aimed to estimate Lp(a) levels in CAD patients and to compare it with healthy controls. To see the correlation between Lp (a) with other lipid parameters and also to find the best cut-off value for Lp(a) in CAD patients in North Karnataka population.
Materials and Methods
This was hospital based, observational, case-control study done on 120 participants, with 60 CAD patients and 60 healthy controls. Lipid profile, Lp(a) and FBS (Fasting Blood Sugar) was analysed along with anthropometric measurements. Quantitative data expressed as mean±SD. Student’s t-test for comparison, Pearson correlation for correlation and Receiver Operating Curve (ROC) to get the best cut-off value for Lp(a) was used.
Results
Lp(a) levels were significantly increased (p<0.001) in CAD patients compared to controls with mean values 52.34±24.87 and 16.81±3.91 respectively. Triglyceride (TG) was significantly increased (p<0.001) and High Density Lipoprotein (HDL) was significantly decreased in CAD patients. Area under the curve is >0.8 with 78% sensitivity and 86% specificity. The best cut-off value is 23.7 mg/dL. Lp(a) positively correlated with Total Cholesterol (TC), Low Density Lipoprotein cholesterol (LDL) and negatively correlated with HDL.
Conclusion
Raised Lp(a) levels is associated with an increased risk and may serve as marker of CAD. When Lp(a) is above 23.7 mg/dL. it acts as a predictor for CAD even when lipid levels are in normal range. It is better to assess the Lp(a) along with routine lipid profile in all patients with CAD in north Karnataka.
Dyslipidemia, Low density lipoprotein variant, Risk factor
Introduction
Cardiovascular Disease (CVD) is the leading cause of death and accounts for 30% of all deaths and 10.3% of disability adjusted life year loss. By the year 2020, it is estimated that CVD will surpass infectious diseases as the world’s leading cause of death and disability. India is predicted to bear the greatest CAD burden according to the estimates from Global Burden of Disease Study [1]. CAD strikes Indian population at younger age and many will be killed in their potential productive years [2].
Risk factors play an important role in initiating and accelerating the complex process of CAD. The modifiable risk factors are dyslipidemia, diabetes mellitus, hypertension, and smoking. Unmodifiable risk factors include age, gender and family history. These conventional risk factors have failed to explain the increasing burden of CAD. Inspite the usage of newer drugs to lower the lipid concentration, CVD continue to be the main cause of death [3]. Thus, necessitating the need to search for newer risk factors like lipoprotein (a) {Lp(a)}, homocysteine, inflammatory markers, endothelin and thrombogenic factors.
Lipoprotein (a) {Lp(a)} is a LDL like particle formed by the association of the highly polymorphic glycosylated apolipoprotein (a) with apolipoprotein B100 attached through a single disulphide bond. It is located on chromosome 6 (6q26-27) on the telomeric region [4]. Lp(a) has emerged as a powerful genetic risk factor for CAD [5]. Many studies documented that Lp(a) in excess increases the risk of premature CAD even in the presence or absence of concomitant risk factors [6,7]. Lp(a) is structural analogue and competitive inhibitor of plasminogen leading to impaired fibrinolysis. Lp(a) accumulates in the vessel wall and inhibits binding of plasminogen to cell surface and promotes proliferation of smooth muscle cells. Hence Lp(a) has atherogenic and thrombotic properties [8]. Different population across the globe have shown Lp(a) worldwide ethnic variation with different levels associated with CAD [9,10].
Hence, this study was aimed to estimate Lp(a) levels in CAD patients and to compare with healthy controls. To see the correlation between Lp(a) with other lipid parameters and also, to find the best cut-off value for Lp(a) in CAD patients in North Karnataka population.
Materials and Methods
This was hospital based observational case control study conducted in the Department of Biochemistry, tertiary care teaching hospital in Karnataka. The study protocol was approved by Institutional Ethics Committee (IEC) with reference number SNMC/IECHSR/2014-15/A-18-1.1. Study was conducted over a period of one year from January to December 2016.
The study comprises of 120 subjects. Sample size was calculated using open-epi version 2.3.1 software. Taking Mohan V et al., reference, at 95% confidence interval and 80% power, sample size was 57 in each group [11]. Sixty patients who were clinically diagnosed of CAD coming to Medicine, Cardiology OPD and admitted patients were chosen for the study. The CAD patients were selected on the basis of coronary angiography i.e., presence of atleast 50% stenosis in major coronary arteries, ECG, Echocardiograph and previous medical records. Age and sex matched 60 healthy controls in the age group of 40-80 years, who were non-diabetic, non-hypertensive and nonsmokers were enrolled in the study. Presence of CAD in controls was ruled out by detailed clinical history, ECG pattern, echocardiography and family history. Patients with thyroid disorders, nephrotic syndrome, stroke, chronic liver and renal diseases, cancer, pregnant women and women on oral contraceptives, hormone replacement therapy were excluded from the study group.
Informed consent was taken from all participants before the study. Care was taken to maintain the confidentiality of the patients as per Helsinki declaration. For each patient detailed history was taken on smoking, family history, medication and medical records. General physical examination and anthropometric measurements like height and weight were recorded. Body Mass Index (BMI) was calculated using the formula Wt (Kg)/Ht (m2).
Under aseptic precaution 6 mL of fasting venous blood was drawn and serum was separated by centrifugation. The serum was used for estimation of biochemical parameters like blood glucose (FBS), lipoprotein (a) and lipid profile fasting. Two mL blood was collected in sodium floride bulbs for glucose estimation. Glucose was determined by glucose oxidase and peroxidase (GOD –POD) method. Total cholesterol by cholesterol oxidase and peroxidase method, TG’s by glycerol phosphate method. HDL-C estimated by direct method and LDL-C was calculated by Friedewald’s formula i.e., LDL=TC-TG/5-HDL. Lp(a) was estimated by immunoturbidemetric method [12]. All parameters were measured in fully automated analyser, Biosystem A25 using Biosystem kits on the same day. Lipid ratios were calculated by using formulae TC/HDL, LDL/HDL, and TG/HDL.
Statistical Analysis
All statistical analysis was done using software Statistical Package for the Social Sciences (SPSS) version 13. Quantitative data has been expressed in terms of mean±SD. Student’s t-test was used for comparison of groups and Pearson’s correlation test was applied for correlation of Lp(a) with other parameters. Receiver Operating Curve (ROC) was put to find the best cut off value for Lp(a) in CAD patients. A p<0.05 was considered as statistically significant.
Results
The 60 CAD patients were in the age group of 40 to 80 years. Among them 38 were male and 22 were female patients and there was no significant difference in age and sex ratio between cases and controls. Males are affected more in our study, this may be due to (29) 48% of CAD patients were smokers. The BMI, systolic and diastolic blood pressure and fasting blood glucose were significantly (p<0.05) higher in CAD patients as compared to controls as depicted in [Table/Fig-1].
Baseline characters in cases and controls.
| Parameters | Casesn = 60 | Controlsn =60 | t | p-value |
|---|
| Male: Female | 38:22 | 35:25 | - | - |
| Age in year | 58.85±12.82 | 55.72±16.24 | 1.17 | 0.243 |
| BMI Kg/m2 | 26.37±3.54 | 24.87±1.32 | 3.06 | 0.003 |
| SBP mm of Hg | 134±10 | 112±9 | 12.52 | <0.001 |
| DBP mm of Hg | 94±6 | 78±6 | 13.57 | <0.001 |
| FBS mg/dL | 135.84±42.92 | 85.45±16.04 | 10.38 | <0.001 |
BMI= Body mass index, SBP=Systolic blood pressure DBP= Diastolic blood pressure, FBS= Fasting blood sugar.
p<0.05 statistical significant
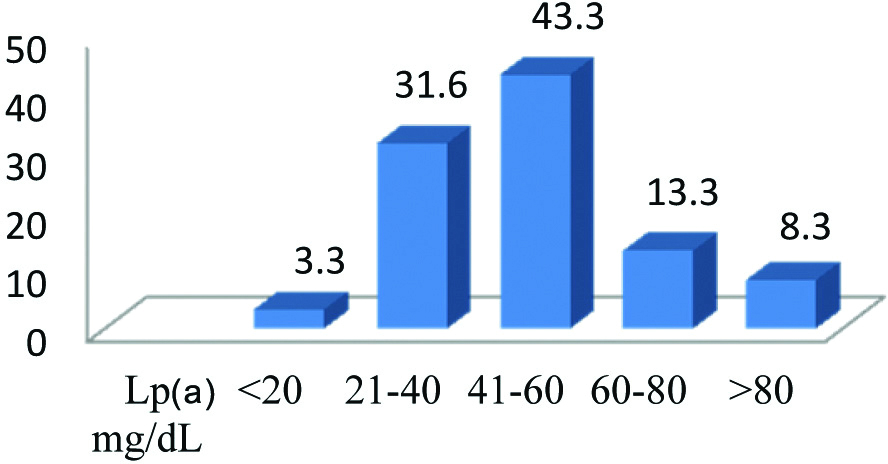
There was statistically significant increase (p<0.001) in TGs and VLDL and significant decrease (p<0.001) in HDL in CAD patients compared to control group. Even though, there was difference in TC and LDL but it was not statistical significant. There was significant increase (p<0.001) in Lp(a) in CAD patients compared to controls. Mean Lp(a) levels in CAD patients were 52.34±24.87 which was highly significant (p<0.001) compared to controls 16.81±3.91. There was significant increase in lipid ratios TC/HDL, TG/HDL and LDL/HDL in cases compared to controls as shown in [Table/Fig-2]. Distribution of Lp(a) among the CAD patients was shown in [Table/Fig-3]. Majority of the CAD patients i.e., 43.3% had Lp(a) levels in the range of 41-60 mg/dL followed by 31.6 % in the range of 21-40 mg/dL. The cut-off value for Lp(a) was 23.7 mg/dL in CAD patients in our study. Most of CAD patients had Lp(a) levels were above this value.
Comparison of lipid profile and Lp(a) in cases and controls.
| Parameters | Cases | Controls | t | p-value |
|---|
| T cholesterol mg/dL | 153.69±39.63 | 145.78±23.41 | 1.333 | 0.185 |
| Triglyceride mg/dL | 139.06±80.41 | 92.01±22.46 | 4.366 | <0.001 |
| HDL mg/dL | 30.86±5.62 | 38.76±7.36 | 6.604 | <0.001 |
| LDL mg/dL | 94.59±32.07 | 88.62±23.51 | 1.18 | 0.24 |
| VLDL mg/dL | 28.24±18.7 | 18.4±4.49 | 3.95 | <0.001 |
| Lp(a) mg/dL | 52.34±24.87 | 16.81±3.91 | 10.93 | <0.001 |
| TC/HDL | 5.21±1.96 | 3.8±0.93 | 4.73 | <0.001 |
| TG/HDL | 4.78±3.46 | 2.46±0.77 | 5.053 | <0.001 |
| LDL/HDL | 3.23±1.45 | 2.38±0.83 | 3.91 | <0.001 |
HDL=High density lipoprotein, LDL=Low density lipoprotein, VLDL= Very low density lipoprotein, TG=Triglyceride
p<0.05 considered as statistical significant
Percentage of CAD patients depending on Lp(a) levels.
[Table/Fig-4] shows the correlation of Lp(a) with other lipid parameters. Lp(a) shows significant positive correlation with TC and LDL where as negative correlation with HDL. There was also positive correlation with TC/HDL and LDL/HDL. ROC for Lp(a) in CAD patients is shown [Table/Fig-5]. Area under the curve is >0.8 which is highly significant (p<0.001). In our study we found cut-off value was 23.7 mg/dL with 78% sensitivity and 86% specificity shown in [Table/Fig-6]. This suggests that Lp(a) above this cut off value can be used to evaluate risk of CAD in our region.
Correlation of Lp(a) with other lipid parameters in CAD patients.
| Parameters | r-value | p-value |
|---|
| Lp(a) | TC | 0.385 | 0.002 |
| TG | 0.101 | 0.442 |
| HDL | - 0.455 | <0.001 |
| LDL | 0.494 | <0.001 |
| VLDL | 0.104 | 0.428 |
| TC/HDL | 0.549 | <0.001 |
| TG/HDL | 0.227 | 0.08 |
| LDL/HDL | 0.623 | <0.001 |
p<0.05 statistical significance
ROC curve of Lp(a) to detect the best cut-off value in CAD patients.
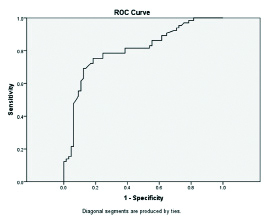
Sensitivity, specificity and AUC of Lp(a) in CAD patients.
| Sensitivity | Specificity | AUROC | Cut-off value | p-value |
|---|
| Lp(a) mg/dL | 78.3 % | 86.4% | 0.8 | 23.7 mg/dL | < 0.001 |
Discussion
In the present study we evaluated the significance of novel biomarker i.e., Lp(a) in CAD patients. Recently Lp(a) is emerging as a strong biomarker of CAD. Our result shows high levels of TG and low levels of HDL and is strongly associated with CAD. A large cross-sectional study conducted in North India by Ashfaq F et al., found increased TG and very low HDL levels in diseased vessel patients as compared to those with normal coronary status [13]. They also indicated that usefulness of estimation of TG to identify the presence of CAD even when the patients are receiving treatment i.e., hypolipidemic drugs like statins. Austin MA et al., reported TG levels more than 130 mg/dL are strongly associated with the extent of patient’s coronary atherosclerosis and states that hypertriglyceridemia is commonly associated with CAD patients [14]. Low levels of HDL are reported to increase the risk of cardiovascular disease even when cholesterol is not elevated [15,16]. Low HDL level is an independent risk factor for CAD [17]. In our study, we did not find any statistical difference in TC and LDL levels in CAD patients compared to controls. Atherogenicity of Lp(a) is more marked with concomitant decrease in HDL levels which was also seen in our study [18].
In this study we estimated Lp(a) levels in CAD patients and controls. We also made an attempt to find out cut-off value for Lp(a) levels using ROC. We found higher levels of Lp(a) in CAD patients, our results are in agreement with other studies [19-21]. Ashfaq F et al., reported that Lp(a) levels correlated positively with severity of atherosclerosis [19]. Lp(a) levels of 21mg/dL are associated with presence of CAD even when cardiovascular risk factors and specific treatments were taken. In north Indian studies by Yusuf J et al., and Gupta R et al., showed highest Lp(a) levels were observed in triple vessel disease, followed by double and single vessel disease [20,21]. CAD patients showed almost five fold higher Lp(a) levels as compared to controls [22]. Zampoulkis JD et al., studied the relationship of excess Lp(a) with extent and severity of atherosclerosis in CAD patients. They revealed that Lp(a) is related to diffuse lesions covering large part of coronary vasculature [23]. Lp(a) competitively inhibit plasminogen activity, leading to impaired fibrinolysis. The smaller the apo (a), the higher are the Lp(a) levels and the risk for CAD. It enhances the oxidation and foam cell formation.
In our study, cut-off value was 23.7 mg/dL with 78% sensitivity and 86% specificity. A study on 151 south Indian patients, by Rajashekhar D et al., shown Lp(a) >25 mg/dL is associated independently with around two fold risk of CAD [10]. A north Indian study by Hoogeveen RC et al., had proposed a cut off value was >19 mg/dL in 103 subjects [24]. Another largest north Indian study by Yusuf J et al., showed Lp(a) above 40 mg/dL assessed by an isoform insensitive assay is an independent risk factor for CAD [20]. According to Saini V et al., Lp(a) showed independent predictor of CAD irrespective of traditional risk factor with good sensitivity and specificity. The best cut-off value of Lp(a) came out to be 45 mg/dL [9]. Lp(a) levels above 20mg/dL are reported to be associated with a high risk of CAD [25]. Studies found that patients with Lp(a) levels more than 30 mg/dL had risk of CAD increased by about three fold [26,27].
We noted there was significant positive correlation of Lp(a) with TC, LDL, TC/HDL and LDL/HDL and negative correlation with HDL which are in agreement with other studies [28,29]. A large cohort study from five European countries comprising of 56,804 individuals reported that elevated Lp(a) was robustly associated with an increased risk of major coronary events. Total cholesterol correlated positively with Lp(a) levels [28]. A study by Pedreno J et al., reported Lp(a) levels associated with LDL cholesterol [29].
Limitation
Small sample size, genetic data is not provided. It is recommended to conduct study in larger sample size.
Conclusion
In this study we were able to show Lp(a) as one of the reliable marker, as Lp(a) was found to be raised significantly in CAD patients compared to controls. Since Lp(a) levels show wide ethnic variation, an attempt has been made to derive the best cut-off value for Lp(a) levels in CAD patients in North Karnataka population.
BMI= Body mass index, SBP=Systolic blood pressure DBP= Diastolic blood pressure, FBS= Fasting blood sugar.
p<0.05 statistical significant
HDL=High density lipoprotein, LDL=Low density lipoprotein, VLDL= Very low density lipoprotein, TG=Triglyceride
p<0.05 considered as statistical significant
p<0.05 statistical significance
[1]. Murry CJ, Lopez AD, Alternative projections of mortaliy and disability by cause 1990-2020: Global burden of disease studyLancet 1997 349(9064):1498-504.10.1016/S0140-6736(96)07492-2 [Google Scholar] [CrossRef]
[2]. Leeder S, Raymond S, Greenberg H, A race against time: The challenge of of cardiovascular disease in developing countries 2005 New York NYColumbia university [Google Scholar]
[3]. Braunwald E, Shattuck lecture cardiovascular medicine at the turn of he millennium: Triumphs, concerns and opportunitiesN Engl J Med 1997 337:1360-69.10.1056/NEJM1997110633719069358131 [Google Scholar] [CrossRef] [PubMed]
[4]. Berg K, A new serum type system, the Lp(a) systemActa Pathol Microbiol Scand 1963 59:369-82.10.1111/j.1699-0463.1963.tb01808.x14064818 [Google Scholar] [CrossRef] [PubMed]
[5]. Danish J, Collins R, Peto R, Lipoprotein (a) and coronary artery disease: A meta analysis of prospective studiesCirculation 2000 102:1082-85.10.1161/01.CIR.102.10.108210973834 [Google Scholar] [CrossRef] [PubMed]
[6]. Gambhir JK, Kaur H, Gambhir DS, Prabhu KM, Lipoprotein (a) as an independent risk factor for coronary artery disease in patients less than 40 years of ageInd Heart J 2000 52:411-15. [Google Scholar]
[7]. Enas EA, Chako V, Sethilkumar A, Elevated lipoprotein (a)- A genetic risk factor for premature vascular disease in people with or without standard risk factors: A reviewDis Mon 2006 52:5-50.10.1016/j.disamonth.2006.01.00216549089 [Google Scholar] [CrossRef] [PubMed]
[8]. Caplice NM, Panetta C, Peterson TE, Kleppe LS, Mueske CS, Kostner GM, Broze GJ, Simari RD, Lp(a) binds and inactivates tissue factor pathway inhibitor: a novel link between lipoproteins and thrombosisBlood 2001 98(10):2980-87.10.1182/blood.V98.10.298011698280 [Google Scholar] [CrossRef] [PubMed]
[9]. Saini V, Bhatnagar MK, Bhattacharjee J, Evaluation of homocysteine, lipoprotein (a) and endothelin as diagnostic marker of coronary artery disease in Indian populationInternet Journal of Medical Update 2013 8(1):17-23. [Google Scholar]
[10]. Rajashekhar D, Saibaba KSS, SrinivasaRao PVLN, Latheef SAA, Subramanyam G, Lipoprotein (a): better accessory of coronary heart disease risk in south Indian populationInd J Clin Biochem 2004 19:53-59.10.1007/BF0289425823105457 [Google Scholar] [CrossRef] [PubMed]
[11]. Mohan V, Raj Deep, Sai Prashanth H, Premalatha G, Rema M, Lipoprotein (a) is an independent risk factor for CAD in NIDDM patients of south IndiaDiabetes Care 1998 21:1819-23.10.2337/diacare.21.11.18199802727 [Google Scholar] [CrossRef] [PubMed]
[12]. Gaubatz JW, Heideman C, Gotto AM Jr, Morrisett JD, Dahlen GH, Human plasma lipoprotein (a). Structural propertiesJ Biol Chem 1983 258(7):4582-89. [Google Scholar]
[13]. Ashfaq F, Goel PK, Sethi R, Khan MI, Wahid Ali, Idris MZ, Lipoprotein (a) levels in relation to coronary artery disease in North Indian patientsHeart Views 2013 14(1):12-16.10.4103/1995-705X.10711423580919 [Google Scholar] [CrossRef] [PubMed]
[14]. Austin MA, Epidemiology of hypertriglyceridemia and cardiovascular diseaseAm J Cardiol 1999 83:13F-6F.10.1016/S0002-9149(99)00209-X [Google Scholar] [CrossRef]
[15]. Reaven GM, Insulin resistant compensatory hyperinsulinemia, essential hypertension, and cardiovascular diseaseJ Clin Endocrinol Metab 2003 88:239910.1210/jc.2003-03008712788834 [Google Scholar] [CrossRef] [PubMed]
[16]. Ramachandra A, Sathyamurthy I, Snehalatha C, Risk variables for coronary artery disease in Asian IndiansAm J Cardiol 2001 87(3):267-71.10.1016/S0002-9149(00)01356-4 [Google Scholar] [CrossRef]
[17]. VonEckardstein A, Schulte H, Cullen P, Assmann G, Lipoprotein (a) further increases the risk of coronary events in men with high global cardiovascular riskJ Am Coll Cardiol 2001 37(2):43410.1016/S0735-1097(00)01126-8 [Google Scholar] [CrossRef]
[18]. Cobbaert C, Jukema JW, Zwinderman AH, Withagen AJ, Lindemans J, Bruschke AV, Modulation of lipoprotein (a) atherogenicity by high density lipoprotein cholesterol levels in middle aged men with symptomatic coronary artery disease and normal to moderately elevated serum cholesterol. Regression growth evaluation statin studyJ Am Coll Cardiol 1997 30(6):1491-99.10.1016/S0735-1097(97)00353-7 [Google Scholar] [CrossRef]
[19]. Ashfaq F, Goel PK, Moorthy N, Sethi R, Khan MI, Idris MZ, Lipoprotein (a) and SYNTAX score association with severity of coronary artery atherosclerosis in North IndiaSultan Qaboos University Med J 2012 12(4):465-72.10.12816/000317223275843 [Google Scholar] [CrossRef] [PubMed]
[20]. Yusuf J, Yadav N, Mukhopadhyay S, Goyal A, Mehta V, Trehan V, Reelook at lipoprotein (a): Independent risk factor of coronary artery disease in North Indian populationIndian Heart Journal 2014 66:272-79.10.1016/j.ihj.2014.03.00224973831 [Google Scholar] [CrossRef] [PubMed]
[21]. Gupta R, Vashist S, Bahl VK, Correlation of lipoprotein (a) to angiographically defined coronary artery disease in IndiansIntern J Cardiol 1996 57:265-70.10.1016/S0167-5273(96)02800-8 [Google Scholar] [CrossRef]
[22]. Chopra V, Vasisht S, Gulati S, Manchanda SC, Serum levels of lipoprotein (a) and other lipids in angiographically defined coronary artery disease patients and healthy blood bank donorsIndian Journal of Medical Sciences 2000 54(7):284-89. [Google Scholar]
[23]. Zampoulkis JD, Kyriakousi AA, Poralis KS, Karaminas NT, Palermos ID, Chimonas ET, Lipoprotein (a) is related to the extent of lesions in the coronary vasculature and to unstable coronary syndromesClin Cardiol 2000 23:895-900.10.1002/clc.4960231208 [Google Scholar] [CrossRef]
[24]. Hoogeveen RC, Gambhir JK, Gambhir D S, Kimball KT, Ghazzaly K, Vaduganathan M, Evaluation of Lp(a) and other independent risk factors for CHD in Asian Indians and their USA counterpartsJ Lipid Res 2001 42:631-38. [Google Scholar]
[25]. Panwar RB, Gupta R, Gupta BK, Atherothrombotic risk factors and premature coronary heart disease in India: a case-control studyIndian J Med Res 2011 134:26-32. [Google Scholar]
[26]. Doetsch K, Roheim PS, Thompson JJ, Human lipoprotein(a) quantified by capture ELISAAnn Clin Lab Sci 1991 21(3):216-24. [Google Scholar]
[27]. Maranhao R, Arie S, Vinagre CG, Lipoprotein (a) plasma levels in normal subjects and patients with coronary disease confirmed by coronary angiographyArq Bias Cardiol 1991 56(2):121-25. [Google Scholar]
[28]. Waldeyer C, Nataliya M, Tanja Z, Renate BS, Fabian JB, Torben J, Lipoprotein (a) and risk of cardiovascular disease in the European population: results from the BiomarCaRE consortiumEuropean Heart Journal 2017 :1-9. [Google Scholar]
[29]. Pedreno J, Fernandez R, Ballester A, Petit M, Lack of association of serum lipoprotein (a) levels with type-2 diabetes mellitus in patients with angiographically defined coronary artery diseaseInternational Journal of Cardiology 2000 74(2-3):159-67.10.1016/S0167-5273(00)00304-1 [Google Scholar] [CrossRef]