A Treatment Dilemma: Inadvertently Placed Temporary Dialysis Catheter in the Subclavian Artery of a Critically Ill Patient
Mustafa Salam Mawih1, Isai Gopalakrish Bowline2
1 Fellow, Department of Nephrology, Wake Forest Baptist Medical Center, Wake Forest University, Winston-Salem, NC, USA.
2 Assistant Professor, Department of Nephrology, Wake Forest Baptist Medical Center, Wake Forest University, Winston-Salem, NC, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mustafa Salam Mawih, Medical Centre Blvd, Winston-Salem, NC 27157, USA.
E-mail: Mustafa_mawih@yahoo.com
Each year, more than 5 million Central Venous Catheters (CVCs) are placed in the United States and mechanical complications occur in 19% of them. Despite the advances in the procedure technique and the use of bedside ultrasound, mechanical complications can still occur. Arterial puncture and catheterisation is one of the well-recognised mechanical complications. We report a case of arterial catheterisation of a temporary non-tunneled dialysis catheter in a critically ill patient. The treatment of this complication can be challenging, and, in present case, all treatment options were infeasible. Removal of the CVC from the artery carries a risk of haemorrhage, stroke and pseudoaneurysm, which necessitates a careful consideration of the risks and benefits of each treatment option. Treatment options include manual compression after catheter removal, endovascular and open surgical repair. The present case highlights some of the risk factors associated with arterial catheterisation of CVCs and the limitations of the treatment options.
Central venous catheter, Endovascular procedure, Vascular closure device
Case Report
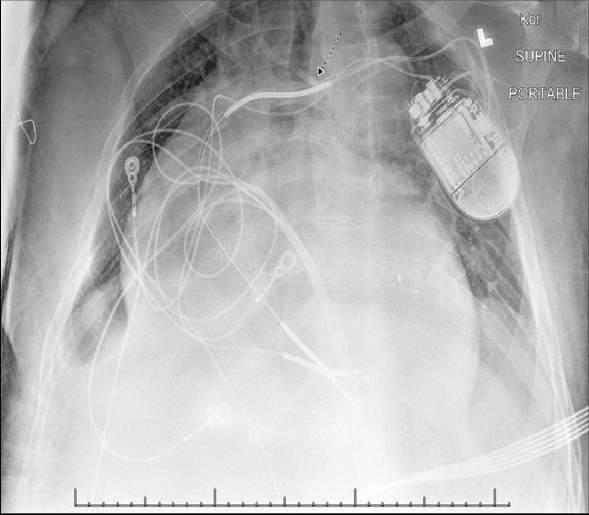
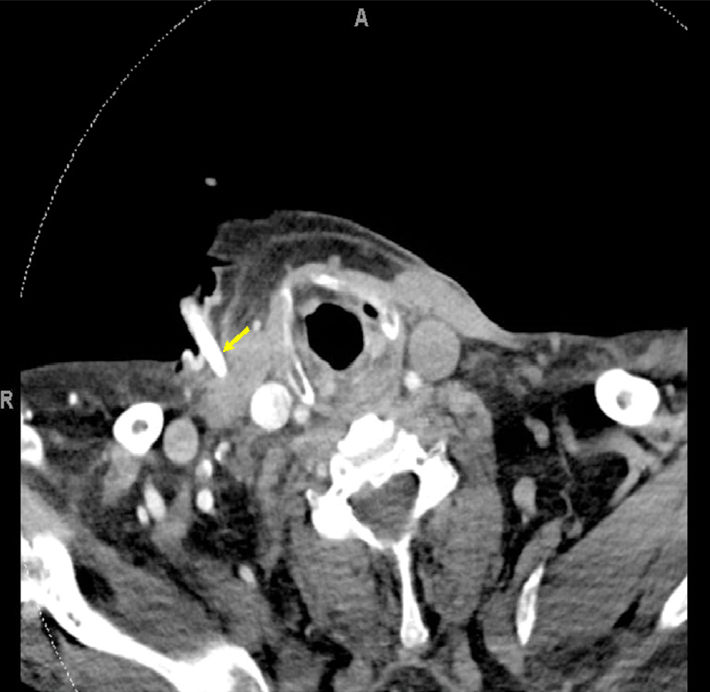
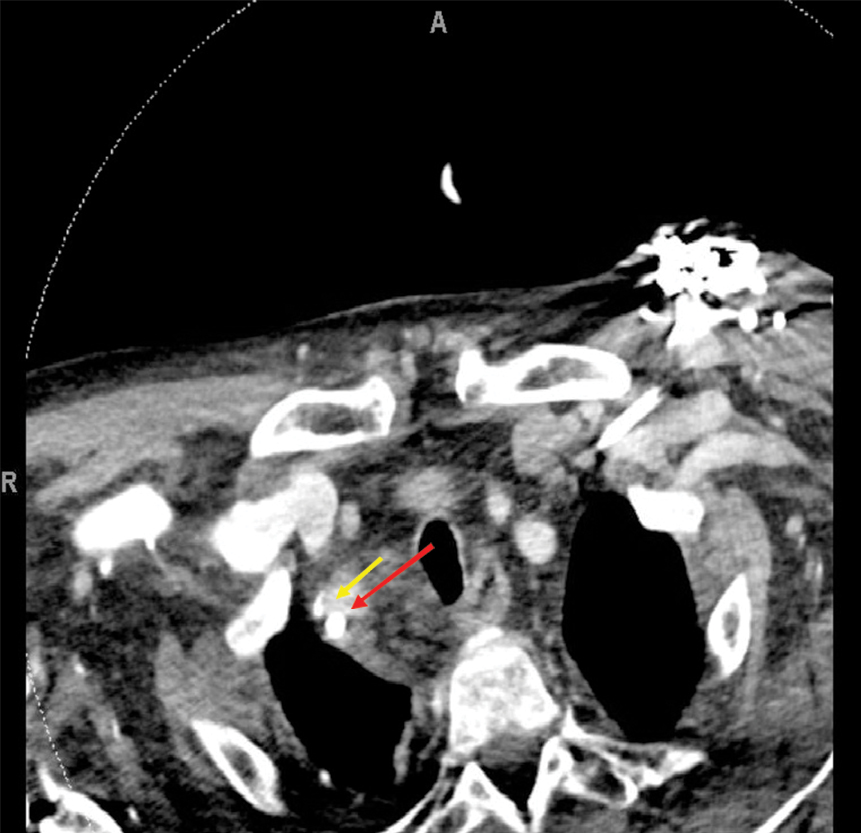
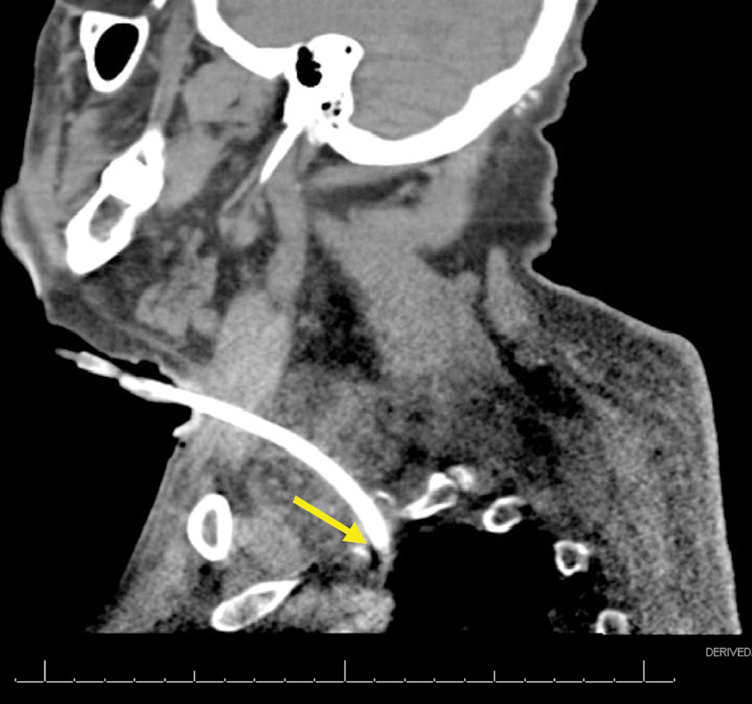
We report the case of a 74-year-old African American male patient, with a past medical history of end-stage renal disease, on haemodialysis for seven years via a left brachiocephalic Arteriovenous Fistula (AVF), admitted to the medical ICU for septic shock in November of 2017. The patient was haemodynamically unstable requiring vasopressors and; therefore, unable to undergo his regular haemodialysis treatment. On the second day of admission, the patient developed fluid overload needing Continuous Veno-Venous Haemofiltration (CVVH) for fluid removal. As a standard practice in our hospital, we do not routinely use AVFs for CVVH, and we placed a temporary dialysis catheter instead. After obtaining an informed consent from the family, we placed a triple lumen (12.5 French) temporary non-tunneled dialysis catheter via right anterior Internal Jugular Vein (IJV) approach using Seldinger technique (after the needle was introduced into the vessel, with ultrasound guidance, a guidewire was advanced through the lumen of the needle and the needle was withdrawn. The dialysis catheter was then passed over the guidewire into the vessel and the guidewire was withdrawn). In the post-procedural Chest X-ray (CXR), the catheter crossed the midline in the superior mediastinum, which was concerning for an arterial placement [Table/Fig-1]. An urgent blood gas from the catheter confirmed arterial placement [Table/Fig-2]. We started heparin drip and obtained an urgent CT angiogram of the head and neck. The CT angiogram showed that the catheter entered the subclavian artery near the origin of the right vertebral artery and within 1 cm of the right common carotid artery [Table/Fig-3,4 and 5], and the tip of the catheter ended at the brachiocephalic artery near the aortic arch [Table/Fig-6]. It also showed that the left vertebral artery was chronically occluded, and the right IJV was narrow distally. Vascular surgery, interventional radiology and cardiothoracic surgery consultant were involved due to the complexity of the case and we considered different treatment strategies. Due to the atriotomy size, deep location, proximity of nearby branch vessels and chronic occlusion of the left vertebral artery, endovascular interventions were too risky and infeasible. We further considered an open surgical repair. However, due to the atriotomy location, we needed to perform at least a partial sternotomy, and the patient was too critical to undergo such a surgery. The patient’s condition continued to deteriorate, and we had a prolonged multi-disciplinary conversation with the family considering all available options. After the family meeting and respecting the patient’s wishes, his code status was changed to comfort measures only and the plan was to avoid any further intervention. We left the catheter in place and discharged the patient to a nearby facility. The patient passed away after one day of discharge.
AP portal CXR showing the catheter course and tip (arrow) crossing the midline in the superior mediastinum which is concerning for arterial placement.
Post-procedural blood gas drawn from the catheter confirming arterial placement.
| Blood gas component | Value | Ref. range for venous blood |
|---|
| pH | 7.39 | 7.320-7.420 |
| pCO2 | 40.8 mmHg | 38.0-48.0 mmHg |
| pO2 | 138.4 mmHg | 35.0-45.0 mmHg |
| HCO3 | 24.4 mEq/L | 22.0-26.0 mmoL/L |
| Base deficit | 0.4 mEq/L | 0.0-2.0 mmoL/L |
| O2 saturation | 98.7% | <70.0% |
CT angiogram of the neck axial view showing the site of catheter entry into the skin (arrow).
CT angiogram of the neck axial view showing the site of catheter entry into the right subclavian artery (long arrow) at the level of the right vertebral artery origin (short arrow).
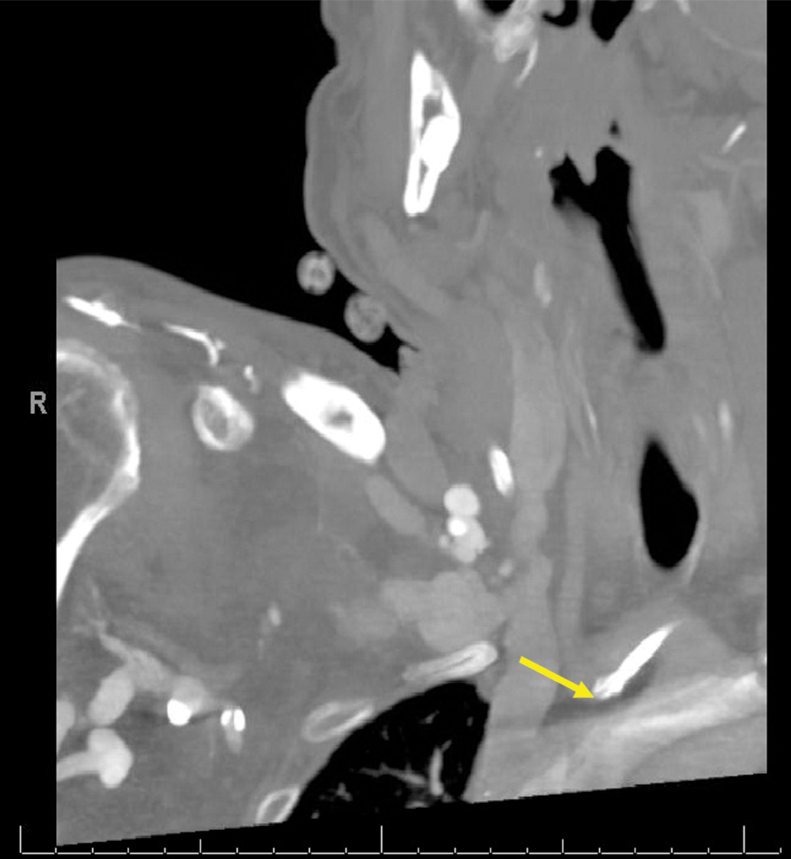
CT angiogram of the neck sagittal view showing the catheter entry into the right subclavian artery.
CT angiogram of the neck right oblique view showing the tip of the catheter at the brachiocephalic artery (arrow) near the aortic arch.
Discussion
Central venous catheter placement is a widely performed procedure in the United States with more than 5 million catheters placed per year [1], and mechanical complications occur in up to 19% of these common procedures [1,2]. One of the mechanical complications is arterial puncture which may lead to arterial catheterisation if not recognised early. Arterial puncture rate during IJV cannulation is between 6.3% and 9.4 % [1] with the rate of arterial catheterisation is less than 1% [3]. It is important to know the risk factors for arterial catheterisation and recognise this potentially fatal complication as early as possible. In a hypotensive patient, the arterial puncture might be harder to recognise due to the less pulsatile backflow of the arterial blood [4,5]. The patient was in septic shock and this put him at risk for arterial catheterisation. Low haemoglobin saturation is another risk factor given that visualisation of a well-oxygenated blood usually gives an immediate clue to its arterial source [4]. This could also happen in critically ill patients, however it was not the case in our patient as the arterial blood gas showed a good oxygen saturation [Table/Fig-2].
Although, ultrasound use has shown to decrease the risk of vascular complications of CVC placement [6], arterial puncture and catheterisation can still happen even with ultrasound guidance [7]. In a prospective study of 714 CVC placement attempts, misplacement rate seemed to correlate with the anatomy of the vein, the valves and angulations between the insertion site and the right side of the heart [2]. In present case, the right IJV was narrow distally which could have been another technical difficulty that led to arterial catheterisations. This highlights the importance of vein anatomy as a risk factor of arterial catheterisation. More focus on vascular imaging and vein anatomy before the procedure may decrease the misplacement risk.
Arterial injuries usually include the carotid artery, vertebral artery, subclavian artery, brachiocephalic artery and thoracic aorta [8]. Removal of the CVC from the artery has a risk of haemorrhage [9], stroke [10] or pseudoaneurysm [11]. Treatment strategies of arterial catheterisation include local compression after catheter removal, endovascular and open surgical repair. Local compression is often helpful if arterial puncture is diagnosed during the procedure before introducing the catheter [12]. In present case, local compression was not an option given the deep arteriotomy site. Open surgical repair adds significant morbidity given it often needs general anaesthesia and sternotomy in critically ill patients [4], and we deferred open surgery in our patient for the same reason. Endovascular repair options include a stent graft placement, an endovascular closure device or a balloon tamponade. Endovascular closure devices have been successful in treating inadvertently placed CVC into the subclavian artery [13]. However, their use for atriotomy size caused by CVC is off label and beyond the manufacturer recommendations [12]. They are approved for arteriotomy size range of (5-8 French) [14]. Covered stents can be effective in certain cases; however, their use is limited by the risk of closing nearby arteries, especially in the subclavian circulation [12]. In our patient, the arteriotomy site was at the level of the Right Vertebral Artery (RVA) origin. Also, further complication in present case was that the RVA was the main blood supply to the posterior cerebral circulation. This was because, after careful review of the CT angiogram, the Left Vertebral Artery (LVA) was chronically occluded and there was no significant posterior cerebral communicating artery. This meant the closure of the RVA had a substantial risk of a massive stroke. Temporary balloon tamponade was effective in treating subclavian arterial injury during inadvertent CVC placement but most of the reported cases were with smaller size catheters (7-7.5 French) [15].
Conclusion
Arterial catheterization is a serious and well-recognised complication of CVC placement. Hypotension in critically ill patients is a risk factor for this complication and one should always keep in mind that arterial puncture in such patients is harder to recognise. Available treatment options include endovascular and open surgical repair. Endovascular repair may be limited by the arteriotomy size and the anatomy of the nearby vasculature, and open surgical repair is often too risky in critical patients. More research in this area may pave the road for the development of new endovascular device or technique for the treatment of this complication.
[1]. Mcgee DC, Gould MK, Preventing complications of central venous catheterizationNew England Journal of Medicine 2003 348(12):1123-33.10.1056/NEJMra01188312646670 [Google Scholar] [CrossRef] [PubMed]
[2]. Sznajder JI, Central vein catheterization. Failure and complication rates by three percutaneous approachesArchives of Internal Medicine 1986 146(2):259-61.10.1001/archinte.1986.00360140065007 [Google Scholar] [CrossRef]
[3]. Shah KB, Rao TLK, Laughlin S, El-Etr AA, A review of pulmonary artery catheterization in 6,245 patientsAnesthesiology 1984 61(3):271-75.10.1097/00000542-198409000-000076476435 [Google Scholar] [CrossRef] [PubMed]
[4]. Pikwer A, Acosta S, Kölbel T, Malina M, Sonesson B, Åkeson J, Management of inadvertent arterial catheterisation associated with central venous access proceduresEuropean Journal of Vascular and Endovascular Surgery 2009 38(6):707-14.10.1016/j.ejvs.2009.08.00919800822 [Google Scholar] [CrossRef] [PubMed]
[5]. Bowdle A, Vascular complications of central venous catheter placement: evidence-based methods for prevention and treatmentJournal of Cardiothoracic and Vascular Anesthesia 2014 28(2):358-68.10.1053/j.jvca.2013.02.02724008166 [Google Scholar] [CrossRef] [PubMed]
[6]. Hind D, Ultrasonic locating devices for central venous cannulation: Meta-AnalysisBMJ 2003 327(7411):36110.1136/bmj.327.7411.36112919984 [Google Scholar] [CrossRef] [PubMed]
[7]. Pillai L, Zimmerman PM, Audiffret ACD, PS170. Inadvertent great vessel arterial catheterization during ultrasound-guided central venous line placement: a potentially fatal eventJournal of Vascular Surgery 2011 53(6):74S10.1016/j.jvs.2011.03.142 [Google Scholar] [CrossRef]
[8]. Ruesch S, Walder B, Tramèr MR, Complications of central venous catheters: Internal jugular versus subclavian access-A systematic reviewCritical Care Medicine 2002 30(2):454-60.10.1097/00003246-200202000-0003111889329 [Google Scholar] [CrossRef] [PubMed]
[9]. Wolfe TJ, Smith TP, Alexander MJ, Zaidat OO, Endovascular treatment of inadvertent cannulation of the vertebro-subclavian arterial junctionNeurocritical Care 2007 6(2):113-16.10.1007/s12028-007-0016-x17522794 [Google Scholar] [CrossRef] [PubMed]
[10]. Guilbert MC, Elkouri S, Bracco D, Corriveau MM, Beaudoin N, Dubois MJ, Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithmJournal of Vascular Surgery 2008 48(4):918-25.10.1016/j.jvs.2008.04.04618703308 [Google Scholar] [CrossRef] [PubMed]
[11]. Bernik TR, Friedman SG, Scher LA, Safa T, Pseudoaneurysm of the subclavian-vertebral artery junctionVascular and Endovascular Surgery 2002 36(6):461-64.10.1177/15385744020360060712476236 [Google Scholar] [CrossRef] [PubMed]
[12]. Yoon DY, Annambhotla S, Resnick SA, Eskandari MK, Rodriguez HE, Inadvertent arterial placement of central venous catheters: diagnostic and therapeutic strategiesAnnals of Vascular Surgery 2015 29(8):1567-74.10.1016/j.avsg.2015.05.03026256713 [Google Scholar] [CrossRef] [PubMed]
[13]. Shetty SV, Kwolek CJ, Garasic JM, Percutaneous closure after inadvertent subclavian artery cannulationCatheterization and Cardiovascular Interventions 2007 69(7):1050-52.10.1002/ccd.2114317421015 [Google Scholar] [CrossRef] [PubMed]
[14]. Bechara CF, Annambhotla S, Lin PH, Access site management with vascular closure devices for percutaneous transarterial proceduresJournal of Vascular Surgery 2010 52(6):1682-96.10.1016/j.jvs.2010.04.07920619582 [Google Scholar] [CrossRef] [PubMed]
[15]. Yu H, Stavas JM, Dixon RG, Burke CT, Mauro MA, Temporary balloon tamponade for managing subclavian arterial injury by inadvertent central venous catheter placementJournal of Vascular and Interventional Radiology 2011 22(5):654-59.10.1016/j.jvir.2011.03.01021514519 [Google Scholar] [CrossRef] [PubMed]