Uterine Rupture in an Unscarred Uterus in Second Trimester: A Case Report
Dhwany M. Munshi1, Manisha M. Laddad2, Gauri R. Shinde3
1 Senior Resident, Department of Obstetrics and Gynaecology, Krishna Institute of Medical Sciences Deemed University, Karad, Maharashtra, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, Krishna Institute of Medical Sciences Deemed University, Karad, Maharashtra, India.
3 Assistant Professor, Department of Obstetrics and Gynaecology, Krishna Institute of Medical Sciences Deemed University, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dhwany Maharshi Munshi, 602, Madhuban Apts., T.P.S.-III, Road No. 51, Borivali (West), Mumbai-400092, Maharashtra, India.
E-mail: dhwany.j23@gmail.com
Uterine rupture in an unscarred uterus is rare and diagnosis is not always obvious; leading to increased morbidity and mortality of the mother and the foetus. Here we report a case of complete spontaneous uterine rupture in a multigravida with 23 week’s pregnancy.
Abruptio placenta, Hysteroscopic resection, Vaginal examination
Case Report
A 22-year-old pregnant lady reported with complaint of pain in abdomen and two to three episodes of vomiting; with tachycardia and mild uterine contractions since one hour. No history of bleeding per vaginum or abdominal trauma was noted. She was gravida three with previous two abortions, with history of suction and evacuation with first abortion, and history of Hysteroscopic resection of the uterine septum, eight months ago. On examination: pulse rate was 120 bpm, blood pressure was 100/60 mmHg, respiratory rate was 18/min, Cardiovascular System examination: S1 S2 heard, no murmur, Respiratory System: air entry equal on both sides. Per Abdomen examination showed uterus was 22 to 24 weeks in size. Mild contractions were present. Vaginal examination revealed cervical os closed, uneffaced. FHS was not detected on portable doppler machine. The differential diagnoses of the present case were- threatened preterm labour, abruptio placenta, uterine rupture, red degeneration of fibroid or acute abdominal surgical causes like appendicitis.
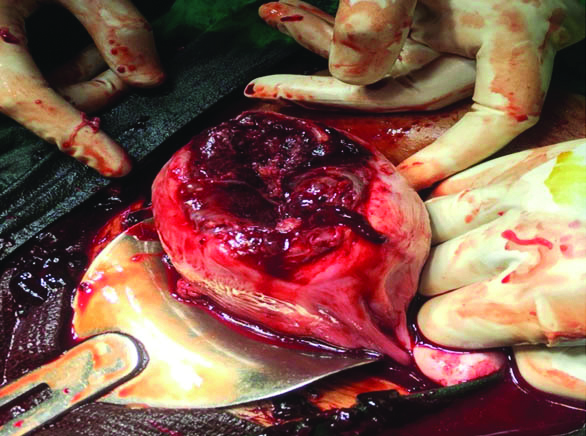
Sonography findings were suggestive of intrauterine foetal demise and haemoperitoneum. Patient was rushed to operation room for an emergency laparotomy. On opening of the abdominal wall, clots of approximately 500 gm and around 1000 mL of blood present in the peritoneal cavity [Table/Fig-1]. An abortus of approximately 950 gm was present in the peritoneal cavity. Intraoperatively Three units of Packed Cell Volume (PCV) and four units of fresh frozen plasma were transfused. A 10x5 cm rent was present at the uterine fundus [Table/Fig-2]. Haemostatic sutures were taken with vicryl no.1 suture material. No intraoperative complications noted. Patient was kept for observation in surgical intensive care unit for 24 hours. No postoperative complications noted. At the time of discharge, patient was counselled against conception for next pregnancy and contraceptive measures were advised.

Rupture at the uterine fundus.
Discussion
Uterine rupture is one of the most serious complications of pregnancy leading to maternal and fetal mortality. Major predisposing factors for uterine rupture include uterine instrumentation, unsupervised labour, previous caesarean sections (C-section), grand multiparity, foetal malpresentation and uterine anomalies. The incidence of uterine rupture is more in a scarred uterus as compared to unscarred uterus; most common cause being previous cesarean section. Thus, in cases where trial of labor for patients with prior C-section is offered, perinatal risks and complications are to be discussed in detail with the patient and well documentation including the consent of the patient are required prenatally. Induction and augmentation with oxytocin, prostaglandin E1 and E2 are not contraindicated but increase the risk of uterine ruptures. Well monitored and supervised labor is the key to avoid complications such as uterine rupture [1].
However, major factors contributing to uterine rupture in unscarred uterus would be uterine trauma due to curettage, uterine abnormalities, obstetric maneuvers, malpresentations, cephalopelvic disproportion, abnormal placentation (most common in placenta percreta), excessive uterine contractions [2]. It is a rare and a late complication in a patient with history of Hysteroscopic surgery. There are predisposing factors like use of electro surgery which increases the risk of uterine rupture by weakening the myometrial tissue and vascular damage; use of monopolar electric current can cause extensive deep tissue necrosis thus causing rupture [3]. In our case, uterine rupture occurred eight months after the Hysteroscopic procedure while Abbas AM et al., reported first uterine rupture after one year [3]; whereas Ergenoglu M et al., reported recurrent uterine ruptures three times in five years, with the first one occurring after two years of procedure [4].
When the risk of uterine rupture for women with different types of risk factors is assessed, these baseline rates of pregnancy-related uterine rupture in women with native, unscarred uteri, specifically, the rates of 0.012% (1 in 8,434) for women living in industrialized countries and 0.11% (1 in 920) for women living in developing countries, represent observational benchmarks that should be referenced for all comparisons [5].
The diagnosis of uterine rupture is difficult as the signs and symptoms are nonspecific and inconsistent to the cause and delay in definitive treatment risks grave complications. Early surgical intervention is most important as it reduces morbidity and mortality. Maternal and foetal outcome and prognosis of uterine rupture depend on the time between diagnoses of uterine rupture and prompt intervention. Foetal complications include neonatal intensive care unit admission, foetal hypoxia or anoxia, and neonatal death. Maternal complications include haemorrhage, hypovolemic shock, bladder injury, obstetric hysterectomy, and death [6].
Some differential diagnoses of a pregnant patient with complaints of pain in abdomen should be ruled out. For example, after foetal well-being is assessed, in cases of early pregnancy, as in the case discussed above, with no other obvious cause in the presence of uterine contractions with no cervical changes, treatment for threatened preterm labour should be given; typically it being use of tocolytic agents. If the ultrasound is suggestive of causes like abruptio placenta, patient has to be posted for emergency caesarean section. Red degeneration of fibroid is a cause to be ruled out in pregnant patients with complaints of pain in abdomen; mostly managed medically with analgesics, rarely surgical management. Acute abdominal causes to be ruled out on ultrasound and depending on the cause medical or surgical management to be decided [7].
Conclusion
The most important symptom in cases of uterine rupture is pain with specific history of predisposing factors is the key to prompt diagnosis and fast intervention. In order to reduce the high mortality and morbidity associated with uterine rupture, measures are to be taken such as regular antenatal care, supervised hospital delivery, health education of the masses, restricted pregnancies.
[1]. Martel MJ, MacKinnon CJ, Guidelines for vaginal birth after previous Caesarean birthJ Obstet Gynaecol Can 2005 27(2):164-88.10.1016/S1701-2163(16)30188-8 [Google Scholar] [CrossRef]
[2]. Guèye M, Baye M, Guèye MDN, Guèye SMK, Diouf AA, Niang MM, Spontaneous uterine rupture of an unscarred uterus before labourCase Reports in Obstetrics and Gynecology 2012 2012:59835610.1155/2012/59835623243529 [Google Scholar] [CrossRef] [PubMed]
[3]. Abbas AM, Abdallah M, Michael A, Recurrent rupture uterus after hysteroscopic resection of uterine septum: A case reportMiddle East Fertility Society Journal 2017 22(4):340-42.10.1016/j.mefs.2017.02.002 [Google Scholar] [CrossRef]
[4]. Ergenoglu M, Yeniel AO, Yıldırım N, Akdemir A, Yucebilgin S, Recurrent uterine rupture after hysterescopic resection of the uterine septumInt J Surg Case Rep 2013 4(2):182-84.10.1016/j.ijscr.2012.10.02223276762 [Google Scholar] [CrossRef] [PubMed]
[5]. Nahum GG, Isaacs C, Uterine rupture in pregnancyhttps://reference.medscape.com/article/275854-overview. Last Updated: Mar 252016,medscape.com/article/275854 [Google Scholar]
[6]. Revicky V, Muralidhar A, Mukhopadhyay S, Mahmood T, A case series of uterine rupture: lessons to be learned for future clinical practiceJournal of Obstetrics and Gynaecology of India 2012 62(6):665-73.10.1007/s13224-012-0328-424293845 [Google Scholar] [CrossRef] [PubMed]
[7]. Hiralal Konar, DC Dutta’s Textbook of Obstetrics_ Including Perinatology and Contraception-JP Medical Pub (2016), Chapter 20, Medical and surgical illness complicating pregnancy, page 35510.5005/jp/books/12540_21 [Google Scholar] [CrossRef]