Materials and Methods
This cross sectional study, which took place in the Department of General Surgery for a period of one year (Feb 2015- Feb 2016) was approved by the Institute Ethics Committee (IEC).
A total of 100 patients (sample of convenience was taken) of American Society of Anaesthesiologists (ASA) I and II status with cholelithiasis for elective laparoscopic cholecystectomy from Feb 2015 to Feb 2016 were included in the study. Patients with hypersensitivity to bupivacaine or tramadol, LC converted to open cholecystectomy and those in which intraperitoneal wash was given were excluded from the study. Informed consent was obtained from all the patients included in the study.
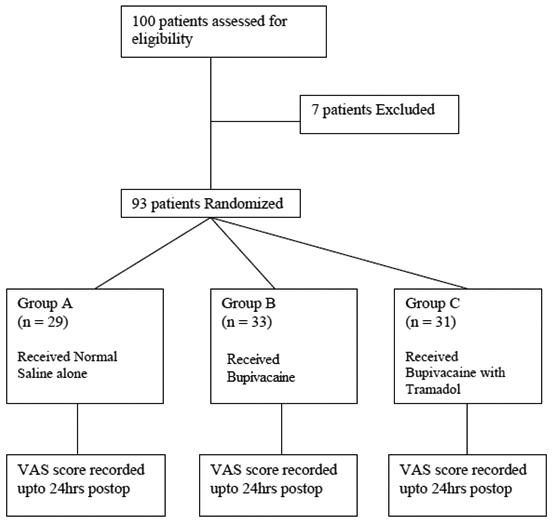
Patients were randomly assigned by a computer generated table into one of three groups. Patient allocated to Group A received 30 mL of inj. normal saline IP, Group B received 30 ml of 0.25% inj. bupivacaine and Group C received 30 ml of 0.25% inj. bupivacaine along with 100 mg inj. tramadol [Table/Fig-1]. The local anaesthetic/analgesic or placebo solution was sprayed on the upper surface of the liver and on right subdiaphragmatic space and over gall bladder bed. This was done using a size 14 infant feeding tube inserted through the subcostal trocar guided by instrument through epigastric port under direct laparoscopic control in supine position.
Flow Diagram: Study design- patients are randomly divided into three groups.
All patients received standard premedication as advised in pre-anaesthetic checkup. General anaesthesia was induced by intravenous administration of fentanyl (2 mcg/kg) and propofol titrated to effect. Orotracheal intubation was done using Inj.vecuronium or rocuronium as per standard dose for the patient. Anaesthesia was maintained using isoflurane, oxygen and air to a desired depth of anaesthesia specific for that patient guided by Monitored Anaesthesia Care (MAC). Minute ventilation was adjusted to keep end-tidal CO2 at 30 to 35 mmHg. Intraperitoneal pressure was maintained at 10-12 mmHg. 10 ml of 0.25% Inj. bupivacaine was given to all patients at the port sites for parietal (somatic) pain to assess the visceral pain better. Study drugs/placebo was instilled fifteen minutes before the end of the surgery according to their allocation to the group by the surgeons (among the researchers).
All patients stayed in post anaesthesia care unit after surgery for two hours. Visual Analogue Scale (VAS) score was recorded by surgeons, not part of the operating team of that particular patient, and hence were blinded as to which drug was being assessed. The intensity of the pain was recorded for all patients using VAS at 0, 1, 2, 6, 12 and 24 hours after surgery.
Rescue analgesia with inj. diclofenac sodium 75 mg IM stat was given in patients with VAS score > 3 and uncomfortable with pain even with VAS </= 3.
Statistical Analysis
Data were analysed by using INSTAT software (Graphpad prism software, Inc,. La Zolla, CA. USA). All results were reported as mean±SD. Demographic data were studied using unpaired Student’s t-test. Differences in the rescue analgesia required, incidence of PONV and comparison of proportional difference between groups for gender were studied using Fishers exact-test. The student t-test of significance was used to compare mean pain score between groups. The p-value ≤0.05 was taken as significant.
Results
A total of 93 patients completed this study. There were no differences (p=0.1469) among the three groups with respect to age, sex, body weight, ASA class, duration of surgery and duration of anaesthesia [Table/Fig-2]. The operative technique (standard four port technique) was similar with regard to factors that can increase postoperative pain, for e.g., adhesions requiring extensive dissection, additional port placements, bile spillage, injury to surrounding viscera, bleeding etc. Seven patients not complying to the eligibility criteria were excluded (In three patients, bile spillage occured and peritoneal wash given; three patients converted to open cholecystectomy; and one wanted discharge on the same day of surgery). No adverse haemodynamic event occurred during surgery. Total of 22 patients suffered from PONV who were managed successfully with intravenous (IV) fluids and IV antiemetics.
Demographic Profile of the 3 groups.
| Variable | Group A(n=29) | Group B(n=33) | Group C(n=31) |
|---|
| Age (years) | 40.44 +/- 7.59 | 36.21 +/- 9.00 | 37.61 +/- 8.75 |
| Male | 9(31%) | 10(30.3%) | 10(32.3) |
| Female | 20(69%) | 23(69.7%) | 21(67.7%) |
| Weight (Kg) | 60.44 +/- 8.29 | 58.90 +/- 10.08 | 61.00 +/- 13.16 |
| ASA I | 21(72.4%) | 25(75.8%) | 24(77.4%) |
| ASA II | 8(27.6%) | 8(24.2%) | 7(22.6%) |
| Duration of General Anaesthesia (min) | 78.79 +/- 12.71 | 80.42 +/_ 12.51 | 77.67 +/- 13.05 |
| Duration of Surgery(min) | 67.96 +/- 8.67 | 67.54 +/- 8.60 | 69.12 +/- 9.79 |
(The difference in age of the three groups was done by one-way Analysis of Variance (ANOVA) and p-value was 0.1469 which was considered not significant)
There was statistically significant difference in postoperative pain intensity between group A and group B during the first 6 hours postoperatively [Table/Fig-3].
Mean VAS score comparison between Placebo (group A) vs Bupivacaine group (group B).
| Duration (hrs) | Placebo Group (n=29)(Group A) | Bupivacaine Group(n=33)(Group B) | p-value |
|---|
| 0 | 5.75±1.10 | 2.96±0.93 | <0.0001 |
| 1 | 4.34±0.92 | 2.63±0.83 | <0.0001 |
| 2 | 4.62±1.06 | 2.39±0.90 | <0.0001 |
| 6 | 4.40±1.35 | 1.84±0.57 | <0.0001 |
| 12 | 2.90±0.36 | 2.8±0.23 | 0.11 |
| 24 | 2.68±0.98 | 2.49±0.17 | 0.27 |
(p-value calculated by unpaired student t-test of significance)
There was statistically significant difference in postoperative pain intensity between group A and group C during the first 6 hours postoperatively [Table/Fig-4]. But the difference in VAS scores between groups B and C were not statistically significant at all times of postoperative recordings.
VAS score comparison between Placebo (group A) vs Bupivacaine+Tramadol group (group C).
| Duration (hrs) | Placebo Group(n=29)(Group A) | Bupivacaine + Tramadol Group(n=31)(Group C) | p-value |
|---|
| 0 | 5.75±1.10 | 2.86±0.83 | <0.0001 |
| 1 | 4.34±0.92 | 2.60±0.74 | <0.0001 |
| 2 | 4.62±1.06 | 2.22±0.47 | <0.0001 |
| 6 | 4.40±1.35 | 1.84±0.24 | <0.0001 |
| 12 | 2.90±0.36 | 2.7±0.46 | 0.06 |
| 24 | 2.68±0.98 | 2.52±0.22 | 0.37 |
(p-value calculated by student t-test of significance)
Thus there was statistically significant reduction of postoperative visceral pain with IP inj. bupivacaine±inj. tramadol compared to placebo group.
With reference to the use of rescue analgesia (WHO step ladder) for all groups, it was observed that all 29 (100%) patients in group A (Placebo) required rescue analgesia compared to 13(39.4%) in group B and 11(35.5%) in group C [Table/Fig-5]. There was statistically significant difference noted in terms of rescue analgesia between group A vs group B (p<0.0001) and also group A vs group C (p<0.0001); however difference between group B vs group C was not statistically significant.
Rescue Analgesia comparison in the 3 groups.
| Group A(Placebo)(n=29) | Group B (Bupivacaine)(n=33) | Group C (Bupivacaine + Tramadol)(n=31) |
|---|
| Rescue Analgesia required | 29(100%) | 13(39.4%) | 11(35.5%) |
The incidence of PONV was also compared between the 3 groups; however there was no statistically significant difference between the groups [Table/Fig-6].
| Post Surgical Symptoms | Group A (Placebo)n=29 | Group B(Bupivacaine)n=33 | Group C(Bupivacaine + Tramadol)n=31 |
|---|
| Nausea n (%) | 7 (24.1%) | 3 (9.1%) | 6 (19.4%) |
| Vomiting n (%) | 3 (10.3%) | 1 (3%) | 2 (6.5%) |
Recovery indices (time to start oral feeds, time to ambulation, length of hospital stay) were observed between the groups [Table/Fig-7]. Although recovery indices in group B and group C were better as compared to group A, it was not statistically significant.
Recovery Indices comparison between three groups.
| (in hours) |
|---|
| Variables | Placebo Group(Group A) | Bupivacaine Group(Group B) | Bupivacaine+Tramadol(Group C) |
|---|
| Time to start oral feeds (hours) | 10.3 | 8.1 | 8.5 |
| Time to Ambulation (hours) | 12.32 | 10.41 | 10.64 |
| Length of Hospital stay (hours) | 28.33 | 24.22 | 24.35 |
There was statistically significant decrease in the requirement of postoperative rescue analgesia when IP inj. bupivacaine and IP inj. bupivacaine + inj. tramadol were used as opposed to placebo group. However, even though there was decrease in incidence of PONV and the recovery indices were better with use of IP local anaesthetics compared to placebo group, the results were not statistically significant.
Discussion
Laparoscopic cholecystectomy is a part of day case surgery hence adequate analgesia and early recovery is of utmost importance. Postoperative pain and nausea are the most common complications of laparoscopic surgery. The pain reaches a maximum level within 6 hour of the procedure and then gradually decreases over a couple of days, but varies considerably between patients [10,11].
Pain after LC can be somatic pain at port site (port site pain) and visceral pain which is caused by residual carbon dioxide in the peritoneal cavity. Visceral pain is mainly due to stretching of the visceral peritoneum and peritoneal inflammation and phrenic nerve irritation [10,12]. Postoperative pain in these patients is observed in peaks immediately after surgery and decreases after 24 postoperative hours [13].
Pain by itself and also by contributing to PONV prolong recovery and hospital stay. Improved postoperative pain management using opioid-sparing regimens may facilitate a high success rate of outpatient laparoscopic cholecystectomy [14].
It is recognised that after laparoscopy shoulder-tip (visceral) pain is a common complaint and may delay discharge from hospital [3]. Instillation of local anaesthetics Intraperitoneally (IP) around the operative site is used as an analgesic technique on the assumption that conduction from visceral sites is obstructed and may lessen the intensity of referred pain to the shoulder (C3,C4) which results from irritation of diaphragm innervations, i.e., phrenic nerve (C3, C4, C5) and diaphragmatic stretching due to gaseous distension, in the postoperative period [4]. Thus, IP drug instillation blocks the visceral afferent signals and modifies visceral nociception.
Hence in this study, it was decided to use IP local anaesthetics after LC and found that IP administration of Inj. bupivacaine (± inj. tramadol) in LC is a safe method and offers significant pain relief in first 6 hours and significant decrease in requirement of analgesics similar to the results obtained by Garza G et al., and also to Rivard C et al., who showed similar results with Inj. bupivacaine in minimally invasive gynecologic and gynecologic cancer surgery [14,15].
Boddy AP et al., conducted a meta analysis on the efficacy of IP local anaesthetics in relieving post-laparoscopic cholecystectomy pain, and found IP local anaesthetics to be efficient in relieving postoperative pain without side effect of analgesic toxicity [16]. In our study as well there was significant pain relief in the first 6 hours postoperatively by IP bupivacaine after taking care of the port site pain by injection bupivacaine in all groups with no significant toxicity.
Yari M et al., in their study demonstrated that IP administration of bupivacaine reduced both visceral and shoulder pains at 4th postoperative hour but had no effect on reduction of rescue analgesic (opioids) [17]. In contrast, our study showed a significant decrease in visceral pain relief after LC in the first 6 hours postoperatively and also there was a significant reduction in the requirement of rescue analgesia in the group B (inj. bupivacaine only) and group C (inj. bupivacaine + inj. tramadol).
There was a decrease in occurence of PONV in both group B (inj. bupivacaine) and group C (inj. bupivacaine + inj. tramadol) compared to group A (placebo) although the difference was not statistically significant. This result was similar to Yari M et al., where they found that IP inj. bupivacaine had no impact on reduction of PONV and the incidence of nausea and vomiting were similar in both groups (placebo and bupivacaine) [17].
However the addition of inj. tramadol to inj. bupivacaine (group C) IP did not cause a significant reduction in pain compared to inj. bupivacaine only group (group B) but there was increased incidence of PONV noted in group C (inj.bupivacaine + inj. tramadol) as compared to group B (inj. bupivacaine only). Memis D et al., found that intraperitoneal tramadol and bupivacaine are very effective for postoperative analgesia in patients undergoing laparoscopic tube ligation, on the contrary, in this study addition of Tramadol IP did not impart any additional benefit in terms of reduction of postoperative pain and PONV [18].
In the present study, the difference in recovery indices (time to start oral feeds, time to ambulation, length of hospital stay), though faster in patients with IP bupivacaine (+/- tramadol) compared to placebo group, was not statistically significant as also observed by Garza G et al., [14].
Our study yielded results comparable to a similar study done by Yadava A et al., where they had found significant decrease in mean pain VAS score by using IP bupivacaine and tramadol after LC [4]. In their study they had also added IP magnesium sulphate (MgSO4) to bupivacaine and had concluded that addition of MgSO4, by antagonising N-methyl-D-aspartate (NMDA) receptors and thereby reducing neuronal signalling as well as pain processing in the central nervous system, resulted in longer duration of pain-free period and less consumption of rescue analgesics in postoperative period compared to IP instillation of tramadol with bupivacaine.
On the contrary Shukla U et al., found that addition of IP instillation of dexmedetomidine 1 μg/kg; which blocks the release of substance P in the nociceptive pathway at dorsal root neuron level; to bupivacaine 0.25% in elective LC is superior to bupivacaine alone and maybe better than bupivacaine and tramadol for postoperative pain relief [19].
Govil N et al., conducted a study designed to study the effect of intraperitoneal instillation of levobupivacaine along with clonidine for pain relief after LC [20]. They concluded that IP levobupivacaine produces postoperative analgesia better than what was obtained with intraperitoneal placebo and the combination of intraperitoneal levobupivacaine and clonidine is superior to the plain levobupivacaine for the relief of postoperative pain in patients undergoing laparoscopic cholecystectomy. These findings corroborated with our study of IP bupivacaine after LC had shown to reduce postoperative pain significantly, however we did not add IP clonidine to bupivacaine.
However, to validate the use of such combinations to IP bupivacaine and also the different doses and concentration of IP bupivacaine and other analgesic drugs for postoperative pain relief following LC further studies are needed on larger populations.
Limitation
One disadvantage of the study is that pain varies from person to person, and depends largely on the pain threshold of each person and how each perceives pain. The tools to measure pain were subjective.
Conclusion
LC is being performed as a part of day-case surgery and postoperative pain is one of the hurdles to day surgery, IP bupivacaine may be used for postoperative pain relief, decreasing need for analgesia and opioids which may lead to early ambulation and initiation of oral feeds, leading to faster recovery and hence shorter hospital stay, thereby decreasing the burden both to the patient as well as to the hospital.
(The difference in age of the three groups was done by one-way Analysis of Variance (ANOVA) and p-value was 0.1469 which was considered not significant)
(p-value calculated by unpaired student t-test of significance)
(p-value calculated by student t-test of significance)