THA is an effective method for patients in the final stages of osteoarthritis. It can reduce the pain, increase the patients’ ability to walk and recover their functions [1]. THA is one of the most common orthopedic surgeries [2], and is widely performed in the world (more than 1 million cases each year) [3]. Pain and dysfunction result from degenerative changes in the hip joint are the most frequent causes of THA [4,5]. Other indications for the surgery can be trauma, hip dislocation, avascular necrosis of femoral neck, Rheumatoid Arthritis (RA), lupus, and so on [6,7]. According to previously published data, after three to six months of THA, pain decreases and range of motion improves [8,9].
THA procedure can be associated with a series of complications, such as infection, hip and knee pain, hematoma in the surgical site, ectopic ossification, thromboemboli, limb-length discrepancies, prosthetic dislocation, and osteolysis [10,11]. These complications are divided into three categories: 1) complications related to surgery in the operating room; 2) short-term complications after surgery; 3) delayed complications after surgery.
There are not enough studies which directly evaluate complications and outcomes of THA. The purpose of the present study was mainly to investigate the results of THA in patents referred to the hospitals in Babol, north of Iran. Our results would be helpful for the clinicians to better find out the positive and negative points of THA procedure and select a good choice for treatment of the patients.
Materials and Methods
Study population: This prospective study was performed on patients who referred to Shahid Beheshti and Ayatollah Rohani teaching hospitals to undergo THA during 2014-2015. Patients with severe knee osteoarthritis, a psychiatric disorder, history of previous arthroplasty, bilateral osteoarthritis, contraindications to a large surgery, and failure to follow-up, were excluded.
Data collection: The following information were collected from the patients: age, sex, height, weight, occupation, family history, smoking history, underlying disease (including arthritis of the hip, diabetes, osteoporosis, etc.,), history of hip fracture, type of fracture, surgical approach (posterior), complications after surgery (early loosening, dislocation, wear, infection, nerve damage).
Patients were evaluated in third and sixth weeks, and at third and sixth months after surgery. To measure physical hip performance, HHS was used. HHS is a scale to evaluate pain, patient’s function during various activities, the deformity level and hip range of motion. Scoring range of 90-100 is excellent, 80-89 is good, 70-79 is average, and below 70 is poor [12].
Preoperative protocol: The procedure of the surgery and follow-up was stated to the patients. They were reassured about the surgical care, pain control and postoperative analgesia, and home discharge as soon as possible after the surgery. Appropriate antibiotic prophylaxis (Keflin 500 mg intravenously every 6 hours) was administered to all patients preoperatively.
Procedure of surgery: All patients underwent THA by the same surgeon. The surgeries were performed through the posterolateral approach. The procedures last between 45 and 90 minutes. All implants had a standard cementless cup and a cementless stem.
Postoperative protocol: Prophylaxis for thromboembolism (enoxaparin 4000 IU) was administered to all patients until they were able to walk independently. Then, enoxaparin was replaced by aspirin (80 to 160 mg per day). Blood transfusion was provided when needed. Two days after the surgery, the patients were encouraged to begin walking (by walker or cane) and physiotherapy was initiated. They also received the activities of daily living retraining.
Statistical Analysis
Collected data were analysed by SPSS software version 17.0. They underwent descriptive analysis. Also, t-test analysis was used to compare the HHS between different categories. A p-value less than 0.05 were considered statistically significant.
Ethical issues: This study was approved by ethical committee of Babol University of Medical Sciences and Health Services with code of MUBABOL.REC.1393.13. The study procedure was explained to all patients before surgery and the informed consent was obtained from all of them.
Results
A total of 58 patients were enrolled in this study, of whom 24 patients (41.4%) were male and 34 patients (58.6%) were female. The average age was 56.8±16.56-year-old. Salient patients’ characteristics are shown in [Table/Fig-1].
Salient characteristics of the patients.
| Variable | N (%) |
|---|
| Gender |
| Male | 24 (41.4) |
| Female | 34 (58.6) |
| Age {Mean±SD (year)} | 56.8±16.56 |
| Smoking |
| Yes | 3 (5.2) |
| No | 55 (94.8) |
| Opium intake |
| Yes | 6 (10.3) |
| No | 52 (89.7) |
| Rheumatoid arthritis |
| Yes | 8 (13.8) |
| No | 50 (86.2) |
| Diabetes mellitus |
| Yes | 4 (6.9) |
| No | 54 (93.1) |
The indications for surgery were as follows: femoral head avascular necrosis, n=20 (34.5%); developmental dislocation of the hip, n=17 (29.3%); degenerative joint disease, n=16 (27.6%); femuro-acetabular impingement, n=5 (8.6%).
Regarding complications of THA, postoperative infection was seen only in one male patient which occurred ten days after the surgery. The complication was resolved by seven days antibiotic therapy. Two patients (one male and one female) over 70 years of age had postoperative posterior dislocation three months after the surgery which were reduced in the operating room. One diabetic male patient aged 78 years suffered from peroneal nerve paresis who was cured after three months. Thromboemboli was not observed in any case.
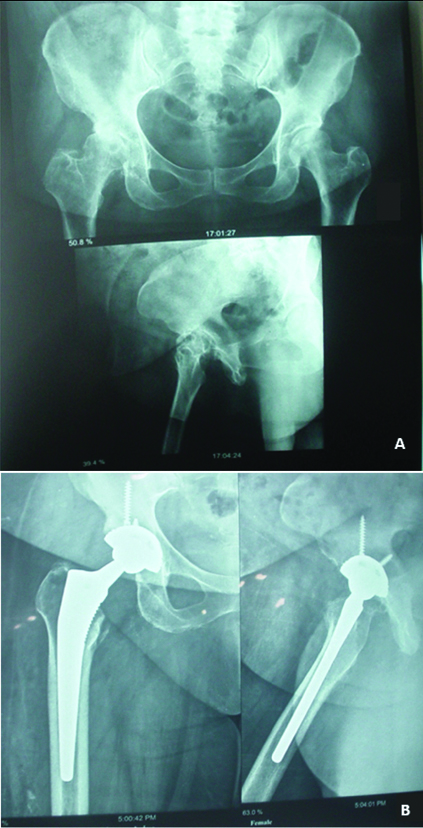
The HHS in patients at different times is presented in [Table/Fig-2]. As demonstrated, although mean HHS decreased during the first three weeks, after that, it was associated with an increase in the amount over time. The mean HHS before surgery was 49.69±5.00 and it progressed to 88.02±4.04 after 24 weeks (p<0.001). [Table/Fig-3] shows good outcome for a female patient, who was first presented with disruptive osteoarthritis of right femoral head, six months after the surgery. The patient was able to walk well and without lagging, and do all the necessary routine work with no pain and limitation.
The Harris Hip Score in patients before and after total hip arthroplasty in the third, sixth, telfth and twenty-fourth weeks.
| Time of Evaluation | Harris Hip Score |
|---|
| Mean | Low Level-High Level |
|---|
| Before Surgery | 49.69±5.00 | 48.37-51 |
| 3rd week | 42.77±5.66 | 41.28-44.26 |
| 6th week | 70.36±6.05 | 68.76-71.95 |
| 12th week | 76.56±4.39 | 77.41-79.73 |
| 24th week | 88.02±4.04 | 87.05-89.18 |
(a) Patient with disruptive osteoarthritis of right femoral head before total hip arthroplasty; (b) After six months, the femoral and acetabular components were stable.
We tried to investigate the association between HHS and diseases of RA and diabetes mellitus in different times. In this regard, no significant differences were found in HHS between the groups with and without these two diseases [Table/Fig-4,5].
Comparison of Harris Hip score between Rheumatoid Arthritis (RA) patients and non-rheumatoid arthritis patients.
| Time of Evaluation | Harris Hip Score | p-value |
|---|
| RA* subjects (Mean±SD) | Non-RA subjects (Mean±SD) |
|---|
| Before Surgery | 47.87±2.29 | 49.98±5.27 | 0.27 |
| 3rd week | 41.62±3.11 | 42.96±5.97 | 0.35 |
| 6th week | 72.25±6.04 | 70.06±6.06 | 0.34 |
| 12th week | 79.62±4.98 | 78.40±4.32 | 0.46 |
| 24th week | 88.12±4.58 | 88.12±4.00 | 0.99 |
* Rheumatoid arthritis
Comparison of Harris Hip score between diabetic patients and non-diabetic patients.
| Time of Evaluation | Harris Hip Score | p-value |
|---|
| Diabetic subjects(Mean±SD) | Non-diabetic subjects(Mean±SD) |
|---|
| Before Surgery | 47.50±6.02 | 49.85±4.95 | 0.36 |
| 3rd week | 41.00±6.37 | 42.90±5.65 | 0.52 |
| 6th week | 70.00±2.16 | 70.38±6.25 | 0.90 |
| 12th week | 76.75±4.57 | 78.70±4.39 | 0.39 |
| 24th week | 84.50±5.91 | 88.38±3.81 | 0.06 |
Discussion
In the present study, we assessed the outcome of the patients who underwent THA. As observed, HHS of the cases reached from 49.7 before the surgery to 88 six months after THA, indicating a satisfactory result. Study by Sachde B et al., indicated that preoperative mean HHS in the patients underwent THA was 49.1, and after four years, it reached to 89.9 and the patients were fully satisfied with their surgery [13]. Gross AE et al., also stated that THA could result in improvement of quality of patients’ lives [14]. Besides, a long-term study on the patients aged <30-year-old showed high rate of survival (>90%), concluding that long-terms outcomes of THA in young patients are similar with those in older patients [15]. In a study by Sharma et al., who compared the outcomes of hemiarthroplasty and THA, the mean HHS in THA group was significantly more than hemiarthroplasty group (90 vs. 80) [16]. Such good outcomes were achieved in other surveys too [17-20], emphasizing the usefulness of THA for the patients’ health recovery.
In our study, no significant differences were seen in the mean HHSs between RA and non-RA patients in different times. In their article, Schnaser EA et al., declared that RA and other inflammatory diseases could affect the status of the patients’ recovery after surgery [21]. On the other hand, reduced rate of postoperative complications were identified in the RA patients versus osteoarthritis patients despite more comorbidities seen in the RA patients. In a study, it was revealed that cases with RA underwent primary THA have a similar survival compared with osteoarthritis patients [22]. Another survey also showed that THA can be a good choice for RA patients who are candidate for the surgery [23]. These reports are in agreement with our results, suggesting that there are probably no limitations for THA in RA patients. However, more studies are necessary to confirm this issue.
Diabetic patients who underwent THA had non-significant higher HHS than non-diabetic ones. In a previous study, HHS does not differ between diabetic and non-diabetic patients, although diabetic subjects may have a higher risk of infection [24]. On the other hand, some researchers explained that the outcomes of the diabetic patients is controversial [25]. This can be caused by factors, such as duration of diabetes, how to control it, and other underlying diseases. Therefore, additional surveys are needed to be done in order to find out the relation between THA outcome and diabetes.
Complications seen postoperatively in our study included infection (one case), neural damage (one case) and posterior dislocation (two cases). In Trojani C et al., study, it was reported that deep vein thrombosis and pulmonary emboli were the most common postoperative complications [26]. Besides, Schairer WW et al., documented that rate of complications differ in various times after surgery [27]. They also stated that the infection mostly occurs in the first three month. One of the complications is infection which can cause a lot of problems for the patient. Therefore, surgeon and patient should both attempt to prevent the incidence of infection in the surgery site. Also, all infections must be treated prior to the surgery. Another potential complication is dislocation, seen more frequently in the cases underwent the surgery because of fractures, and/or in the subjects who have pelvic muscle weakness [28,29]. Differences in postoperative complications depend on many factors, such as surgical facilities, skill and experience of the surgeon, patient’s underlying diseases, his/her compliance to medical care instructions, and so on.
Limitation
One of the limitations that should be mentioned was that our study period was not so long enough that long-term postoperative complications could be investigated. Also, it is suggested that further studies to be performed with larger sample size.
Conclusion
THA had satisfactory outcomes for the patients of osteoarthritis and incidence of complications was not significant. These findings support the fact that THA is an appropriate choice for treatment.
* Rheumatoid arthritis