Mesenteric cysts are rare, benign, intra-abdominal tumour. Mesenteric cysts occur not only in children, but also in adults. The incidence for mesenteric and omental cysts is approximately 1 in 105,000 hospital admissions for adults, and 1 in 20,000 admissions for paediatric cases [1]. It involves the mesentery of the terminal ileum in more than half of the cases [1]. Clinical presentation varies from asymptomatic abdominal lump to an acute abdomen/acute intestinal obstruction [1-4]. The best and standard modality of therapy for mesenteric cysts is complete excision of the cysts [1,2,5,6]. The excision of the mesenteric cysts can be accomplished either by doing laparotomy or using laparoscopic techniques [1,2,6,7].
The purpose of this present study was to review the clinical presentation, operative procedures executed, and the outcome of the surgical therapy of the n=10 cases of mesenteric cysts in children.
Materials and Methods
This was a retrospective study, conducted at the Department of Paediatric Surgery. During Jan 01, 2000 to Dec 31, 2016, 10 children with mesenteric cysts under the age of 12-years were treated by author and were included for this review. This is a single author study and included only the cases managed by the author during the above period. This study included only the cases that were managed by surgical excision of the mesenteric cysts. Children with mesenteric cysts seen by author, but refused surgical therapy were excluded from this study.
All the 10 cases were investigated with skiagram and Ultrasonography (USG) of the abdomen. USG of the abdomen was advised in all the cases and was supportive in preoperative diagnosis of mesenteric cysts. Computed Tomography (CT scan) scans of the abdomen of five children were also available for review, and were diagnostic of mesenteric cysts in all of them.
Results
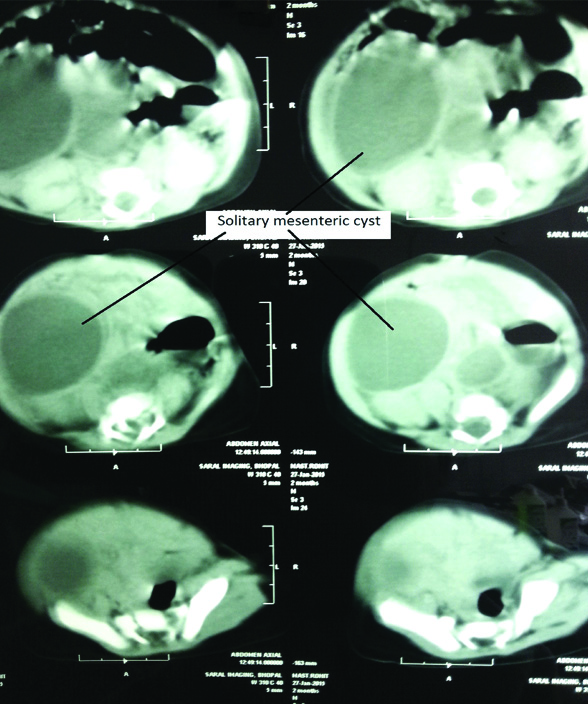
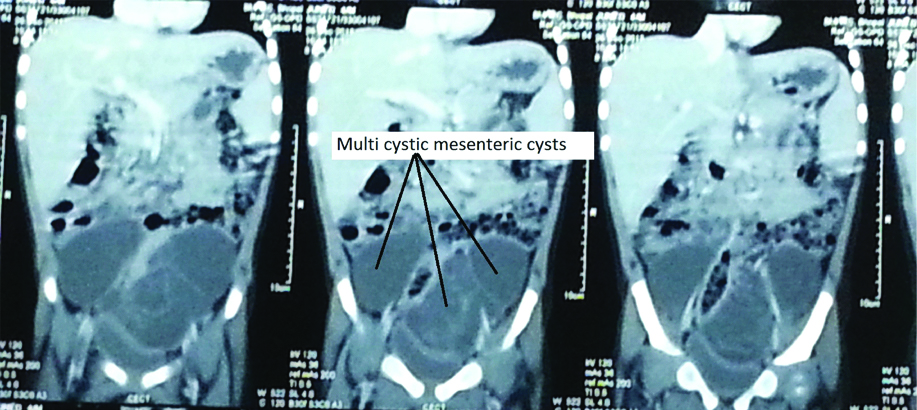
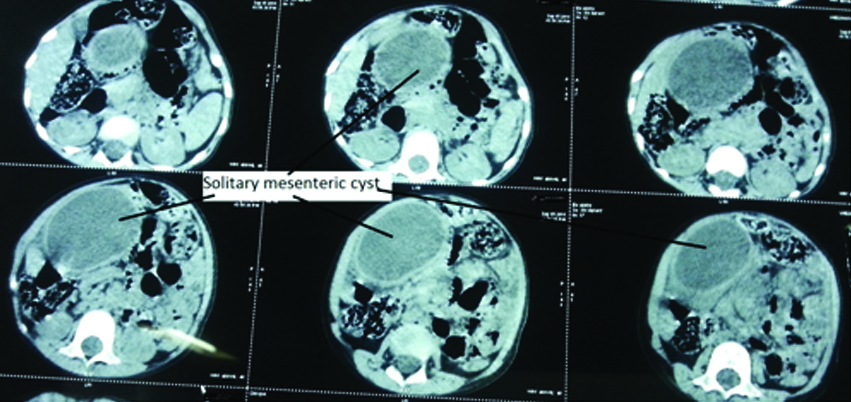
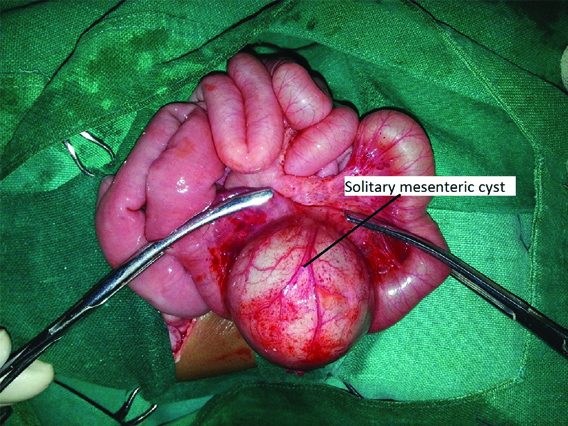
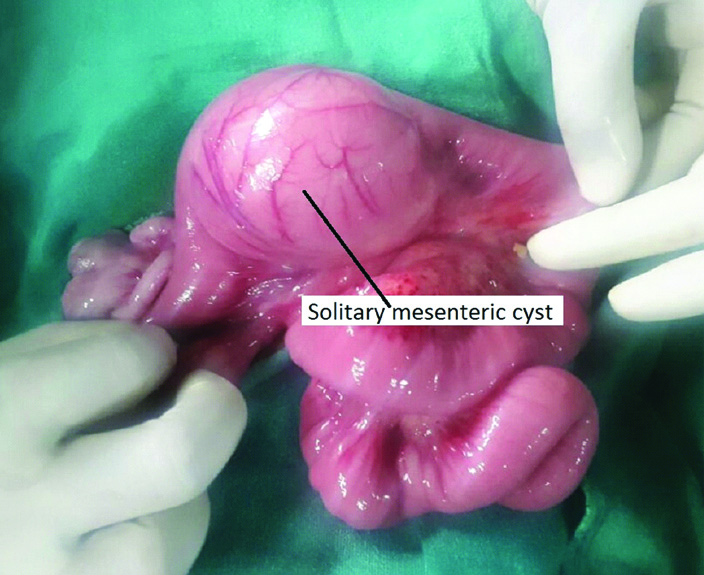
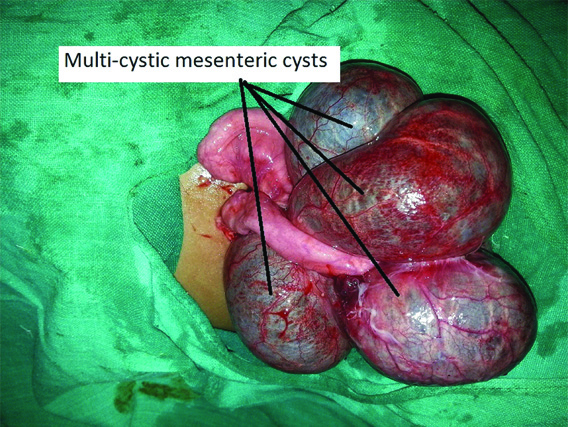
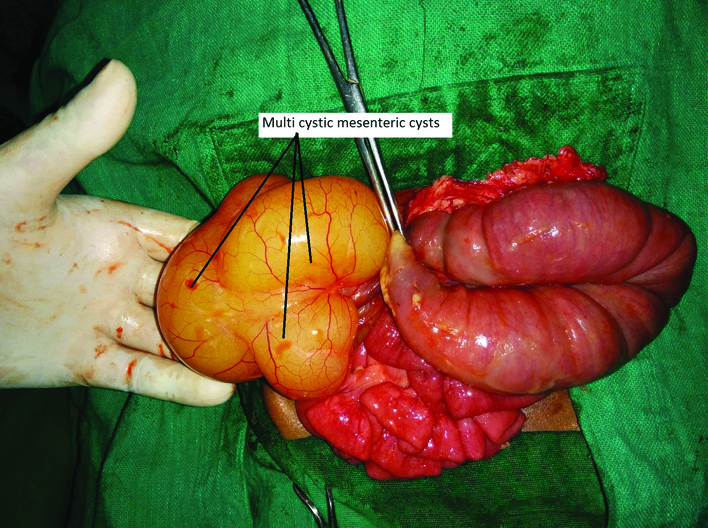
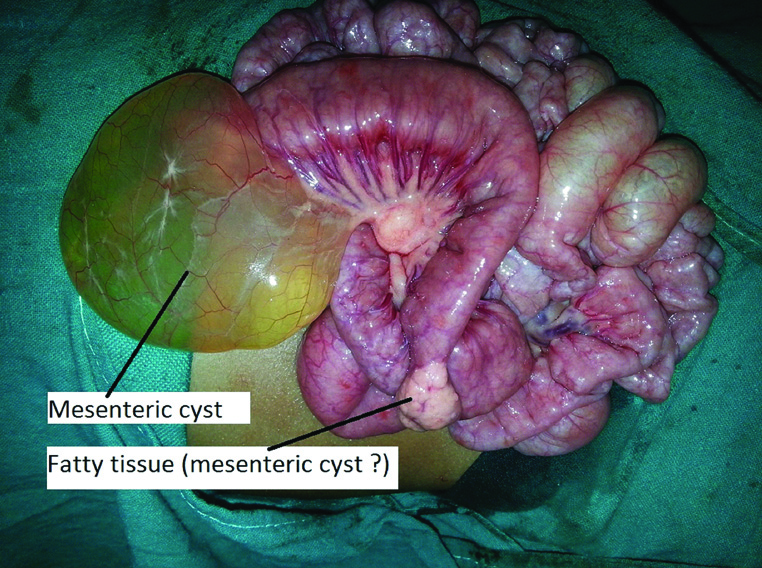
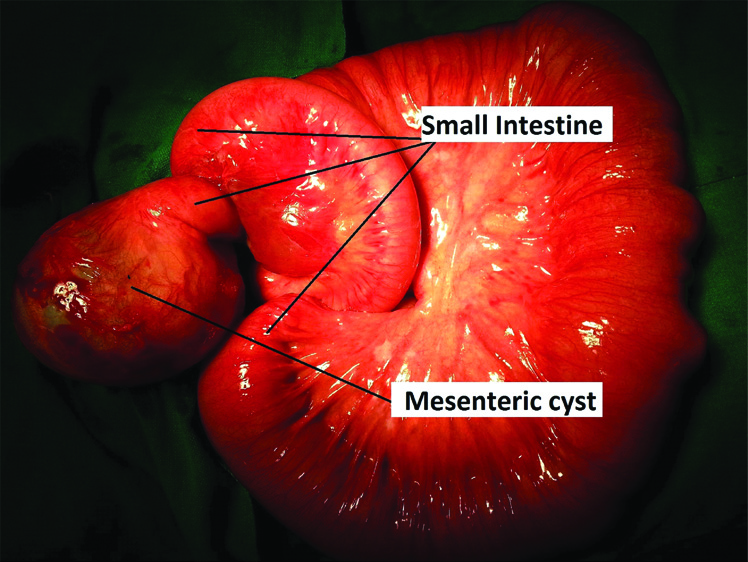
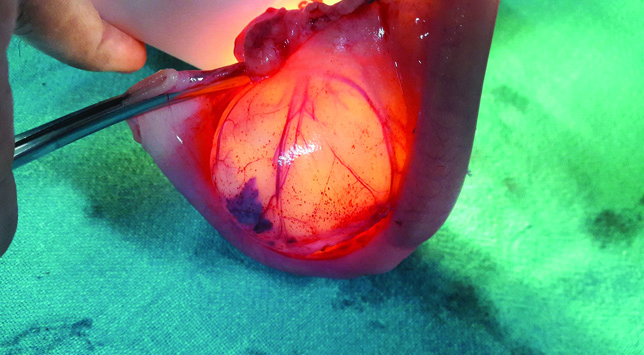
This present review of the management of mesenteric cysts included six boys and four girls. Demographics relating management of the cases are given in [Table/Fig-1]. The age at the time of presentation ranged from 2 to 96 months, with a mean of 43.6±26.84 months. Seven of them presented with features of an acute abdomen/acute intestinal obstruction, and remaining three presented with abdominal lump and abdominal pain. USG of the abdomen was advised in all the cases and was supportive in making a preoperative diagnosis of mesenteric cysts. CT scans of the abdomen were also advised and available for review in five children, and were diagnostic of mesenteric cysts in all the five cases [Table/Fig-2ab,c and d]. Anatomical locations of the cysts were-mesentery of proximal jejunum in five cases, mesentery of distal jejunum in one case, mesentery of proximal ileum in one case and mesentery of distal ileum in three cases. The size of mesenteric cysts ranged from 6 to 11.2 cm in its maximum length. Solitary mesenteric cyst [Table/Fig-3a, 3b], and multi-cystic mesenteric cysts [Table/Fig-3c,d] were equally observed. In one child there were mesenteric cysts at two locations, one was mesenteric cyst and another was fatty tissues/developing mesenteric cyst [Table/Fig-3e]. Volvulus of the small intestine due to mesenteric cysts was observed in 7 (70%) of the cases [Table/Fig-4]. Surgical procedures executed in order of frequency were - en bloc excision of the cysts along with involved jejunum and jejuno-jejunal anastomosis (in five cases); en bloc excision of the cysts along with involved ileum and ileo-ileal anastomosis (in two cases); complete excision of the cyst and repair of mesenteric defects (in two cases); and en bloc excision of the cyst along with involved ileum and ileostomy, which was closed later (in one case). Trans-illumination test was done in all the excised mesenteric cysts, and were either partially or completely positive [Table/Fig-5a,b and c].
Demographics of children with mesenteric cysts (n=10).
| Case No. | Age/SexYear operated | Clinical Presentation | Radiological Investigations | Clinical Diagnosis | Operative Findings | Operation Procedure Executed |
|---|
| Site of lesion | Nature of cysts | Volvulus? |
|---|
| 1. | 4 yrs/M(Oct-2002) | Intestinal obstruction | USG-Abd | Mesenteric cyst | Proximal Ileum | Solitary cyst | No | Complete excision of cyst, and repair of mesenteric defect |
| 2. | 6 yrs/F(June-2003) | Intestinal obstruction | USG-Abd | Mesenteric cyst | Distal Ileum | Multicystic cysts | Yes | En bloc excision of cysts, involved ileum, and ileo-ileal anastomosis |
| 3. | 5 yrs/M(June-2004) | Intestinal obstruction | USG-Abd | Mesenteric cyst | Distal Ileum | Multicystic cysts | Yes | En bloc excision of cysts, involved ileum, and ileo-ileal anastomosis |
| 4. | 8 yrs/M(Jan-2014) | Intestinal obstruction | USG-Abd | Mesenteric cyst | Distal Ileum | Solitary cyst | Yes | (A) En bloc excision of cyst, involved ileum, and terminal ileostomy.(B) Ileostomy closure. |
| 5. | 3 yrs/M(Oct-2014) | Intestinal obstruction | USG-Abd CT scans-Abd | Mesenteric cyst | Proximal Jejunum | Multicystic cysts | No | Excision of cysts, wedge resection of involved jejunum, and jejuno-jejunal anastomosis |
| 6. | 2 mths/M(Jan-2015) | Intestinal obstruction | USG - Abd CT scans-Abd | Mesenteric cyst | Proximal Jejunum | Solitary cyst | Yes | En bloc excision of cyst, involved jejunum, and jejuno-jejunal anastomosis |
| 7. | 2.6 yrs/M(Jan-2016) | Abd lump and Abd pain (03 mths) | USG - Abd CT scans-Abd | Mesenteric cyst | Distal Jejunum | Multicystic cysts | Yes | En bloc excision of cysts, involved jejunum, and jejuno-jejunal anastomosis |
| 8. | 3 yrs/F(Jan-2016) | Intestinal obstruction | USG-Abd | Mesenteric cyst | Proximal Jejunum | Multicystic cysts | Yes | En bloc excision of cysts, involved jejunum, and jejuno-jejunal anastomosis |
| 9. | 20 mths/F(July-2016) | Abd lump and Abd pain (06 mths) | USG-Abd, CT scans-Abd | Mesenteric cyst | Proximal jejunum | Solitary cyst | No | Complete excision of cyst, and repair of mesenteric and meso-colic defects |
| 10. | 3 yrs/F(Sept-2016) | Abd lump and Abd pain (06 mths) | USG-Abd, CT scans-Abd | Mesenteric cyst | Proximal jejunum | Solitary cyst | Yes | En bloc excision of cyst, involved jejunum, and jejuno-jejunal anastomosis |
There were no postoperative complications. All the cases were confirmed to be mesenteric cyst on histopathological examination.
CT scan of abdomen showing solitary mesenteric cyst of size 5.4x4.8x4 cm (case 6).
CT scan of abdomen showing multi cystic mesenteric cysts of size 11.2x5.6x11.2 cm (case 7).
CT scan of abdomen showing solitary mesenteric cyst of size 10.2 x 6.9 cm (case 9).
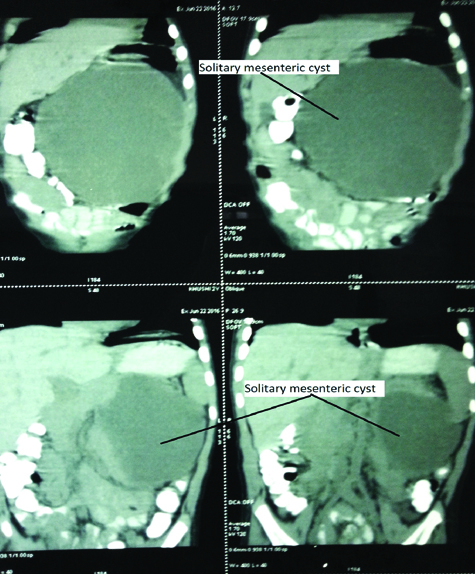
CT scan of abdomen showing solitary mesenteric cyst of size 6.1 x 5.5 cm (case 10).
Operative photograph showing solitary mesenteric cyst (case 6).
Operative photograph showing solitary mesenteric cyst (case 10).
Operative photograph showing multi cystic mesenteric cysts (case 7).
Operative photograph showing multi cystic mesenteric cysts (case 8).
Operative photograph showing mesenteric cyst at one and fatty tissue at another location (case 5).
Operative photograph showing solitary mesenteric cyst with volvulus (case 4).
Tran-illumination test of mesenteric cysts showing (partially positive cysts (case 7).

Tran-illumination test of mesenteric cyst showing completely positive cyst (case 4).
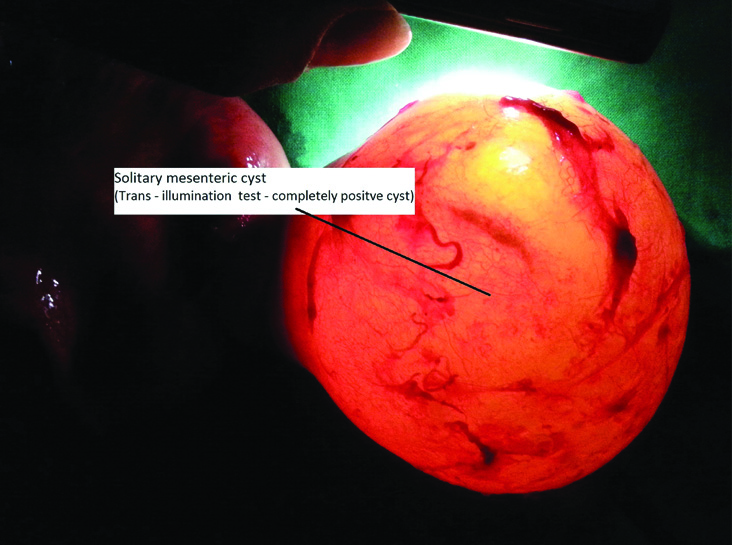
Tran-illumination test of mesenteric cyst showing completely positive cyst (case 10).
Postoperative period was excellent in all. All the excised cysts were subjected for histopathological examination and were reported as mesenteric cysts/cystic lymphangioma of mesentery. None of them reported recurrence in follow up periods that ranged from six months to two years.
Discussion
The exact aetiology of mesenteric cysts is not known. The most accepted theory for the occurrence of the mesenteric cysts was proposed by the Gross, accordingly benign proliferation of ectopic lymphatics in the mesentery that lack communication with the remaining of the mesenteric system [1]. Mesenteric cysts may present from an asymptomatic abdominal mass to an acute abdomen [1-4]. Complications are known to occur with mesenteric cysts and are intestinal obstruction (most frequent), intestinal volvulus, haemorrhage, infection, rupture, and torsion [1,5-7]. Amongst 10 children with mesenteric cysts in present series; seven presented with an acute intestinal obstruction, and remaining three presented with abdominal lump and mild abdominal pain of 3-6 months duration. Intestinal volvulus was observed in seven of the children, one had haemorrhagic fluid within the cysts, but none had intra-cystic infection.
Mesenteric cysts can occur in the mesentery along the gastrointestinal tract anywhere from the duodenum to the rectum [1]. In more than half of the cases the cysts are located in the mesentery of the small bowel and most commonly involve the ileum [1,4,7,8]. Other sites are mesentery of the large bowel, and the retro-peritoneum [5,8,9]. In a study author reviewed 162 cases of mesenteric cysts and found that 60% were located in the mesentery of small bowel, 24% located in the mesentery of large bowel, and 14.5% were retroperitoneal [1]. Mesenteric cysts may be solitary or multiple, unilocular to multilocular, and may contain serous, chylous, haemorrhagic, mixed, or infected fluid. Mesenteric cysts might occur at multiple sites within the peritoneal cavity and are most commonly solitary and multiloculated. It also varies in the size from 4 cm to 40 cm in its maximum length, and the lining of the cysts also vary from a flattened endothelial to the cuboidal or columnar linings [1,7,9-11]. In present series of 10 cases of mesenteric cysts in children, the size of cysts varied from 6 to 11.2 cm in its maximum length, and only one of the case had cysts at two places.
It is possible to diagnose the mesenteric cysts during antenatal sonography, but to supplement the sonographic findings a magnetic resonance imaging is superior and also advisable [1,5,12,13]. USG of the abdomen is the investigation of choice for mesenteric cysts and it provides all details about the size, location, and septations [1,3,6,7]. Although CT scans of the abdomen adds little to the USG findings, but also frequently advised for better anatomical orientation, and identification of its relation to the adjacent organs [1,8]. Although, USG and CT scan of the abdomen are helpful in making the preoperative diagnosis of mesenteric cysts in majority of the cases, but it is not always possible, and the diagnosis is confirmed during surgical exploration for an acute abdomen [1,5]. In present study, USG of the abdomen was done in all, and CT scans of the abdomen were also available for review in five of the cases, and all were diagnostic of mesenteric cysts during preoperative period, although few differential diagnosis were also mentioned in the reports. Differential diagnosis of mesenteric cysts includes omental cysts, choledochal cysts, hydronephrosis, cystic teratoma, and all can be differentiated with the help of clinical examination, x-ray abdomen, USG, and CT scans of the abdomen and other specific investigations [1].
Complete cysts excision remains the treatment of choice with an excellent result, and it is possible in majority of the cases. The excision of the mesenteric cysts can be accomplished either by laparotomy, laparoscopically or by laparoscopic assisted techniques [1,8,10,14,15]. During the management of mesenteric cysts, bowel resection and anastomosis is also required in 20% to 60% of the cases. Rarely, restoration of bowel continuity is not possible following en bloc resection of the mesenteric cyst along with involved bowel, and in that situation creation of a temporary ileostomy is a better option [16].
Few cases have also been reported that the mesenteric cysts were treated with USG guided cyst drainage and ethanol sclerotherapy with encouraging results [17,18]. Amongst 10 children of mesenteric cysts treated by author, seven were subjected to emergency laparotomy due to acute intestinal obstruction, and remaining three children who presented with abdominal pain and lump were explored electively. Small bowel resection along with mesenteric cysts was required in 8 (80%) of the cases and bowel continuity was restored primarily in seven of them. At one occasion due to the disparity in the bowel lumen a temporary ileostomy was created, which was closed selectively two and a half months later. In present study, there were no deaths, and recurrence was also not noticed during the follow up period. Prognosis following complete surgical excision of the mesenteric cyst is excellent, although recurrence has been reported and is more in the cases where the complete excision of the mesenteric cysts [1,2] was not possible. Mortality following surgical treatment of mesenteric cysts is rare, but reported in the literature.
Limitation
The limitation of this present review is that the number of the cases was limited, although mesenteric cysts itself is a rare entity.
Conclusion
Mesenteric cysts are rare, benign, intra-abdominal pathology in children, and 70% of them presented as an acute intestinal obstruction. USG of the abdomen was mostly helpful in making the preoperative diagnosis of the mesenteric cysts in most of the cases, but CT scans of the abdomen were also advised for better anatomical orientation. Volvulus of the small intestine due to mesenteric cysts was observed in 70% of the cases. During surgical excision for mesenteric cysts, bowel resection was also required in 80% of the cases. Early surgical intervention is advisable to prevent complications relating to mesenteric cysts.
There were no postoperative complications. All the cases were confirmed to be mesenteric cyst on histopathological examination.