Introduction
The prevalence of HIV and AIDS continues to grow worldwide. Urological manifestations of HIV and AIDS such as urolithiasis, obstructive uropathy, complicated UTI and malignancy are often first clinical signs. With the availability of antiretroviral drugs and surgical intervention, the prognosis of HIV-infected patients is same as that of general population.
Aim
To evaluate incidence of urological manifestations, their treatment and outcome in HIV and AIDS patients.
Material and Methods: This was retrospective study conducted at Institute of Nephro-Urology, Bengaluru from June 2011 to May 2016. Inclusion criteria were all HIV and AIDS patients suffering from urological diseases. The data were collected in a Microsoft® Excel database and analysed through SPSS 20 version.
Results
A total of 161 patients (male -93, female-68) with HIV and AIDS were analysed retrospectively. The most common presentations were Urosepsis (31.05%), Urolithiasis (27.32%), Malignancy (16.77%), Renal dysfunction (11.18%), Stricture urethra (7.45%), GUTB (Genito-Urinary Tuberculosis) (3.10%) and others (2.4%). The most common surgical intervention done was DJ stenting. Renal abscess, psoas abscess and stricture urethra patients underwent surgical intervention. Uncomplicated UTI was treated conservatively. Sepsis and pyogenic infections were more common in patients with CD4 count <200 cells/mm3. Out come was compared with non HIV-AIDS patients.
Conclusion
Complicated UTI followed by calculus disease were most common in our study. It is important to create awareness of the urologic manifestations of HIV and AIDS among the retroviral positive patients.
CD4 count, DJ stenting, Highly active antiretroviral therapy
Introduction
HIV is a retrovirus that replicates rapidly and kills helper T cells, which are the body’s main cellular defense against infection [1,2]. HIV spreads through contact with blood, semen and cerebrospinal fluid. Low concentrations are found in tears, saliva, breast milk, urine and cervical and vaginal secretions. HIV virus has also been isolated from brain tissue, lymph nodes, bone marrow cells and skin [3,4]. Both viral load and CD4 T-cell count are reliably used to monitor and prognosticate disease progression to AIDS.
Many studies have revealed that Urologic complications like renal dysfunction, urinary tract infection, urogenital tuberculosis, prostatitis, prostatic abscess, epididymo-orchitis, urologic malignancies, sexual dysfunction and infertility are often the first clinical signs of HIV and AIDS [5-9]. With Highly Active Antiretroviral Therapy (HAART) and antibiotic prophylaxis, HIV positive patients have a life expectancy of >20 years [10].
Now with longer survival to an almost normal life expectancy, there is an increase in the prevalence of HIV-related disorders, including urological problems that arise relating to infections, malignancies or drug treatment [11-13]. These patients with common urologic disorders are now actively treated for quality of life. Thus the population living with HIV, needs treatment for expected age related conditions, complications of the disease and therapies they receive and therefore, the need of the awareness of the urologic manifestations of HIV and AIDS arises and advising these patients for the subsequent management of the respective disorders is good for both the patient and the Urologists.
This study was designed to evaluate the incidence of urological manifestations in HIV and AIDS patients and various treatment modalities with outcomes. To evaluate incidence of urological manifestations, their treatment and outcomes in HIV and AIDS patients.
Materials and Methods
This retrospective study was conducted in the department of urology, Institute of Nephro-Urology, Bengaluru, Karnataka, India from June 2011 to May 2016. The data were collected in a Microsoft® Excel database from the hospital records and analysed through SPSS 20 version.
Inclusion criteria: Patients with urological and nephrological manifestations, newly diagnosed HIV Positive and already on HAART were included and their treatment modality and treatment outcome were assessed.
Exclusion criteria: Negative HIV and AIDS cases. The institutional ethical committee approval was obtained for the study.
Results
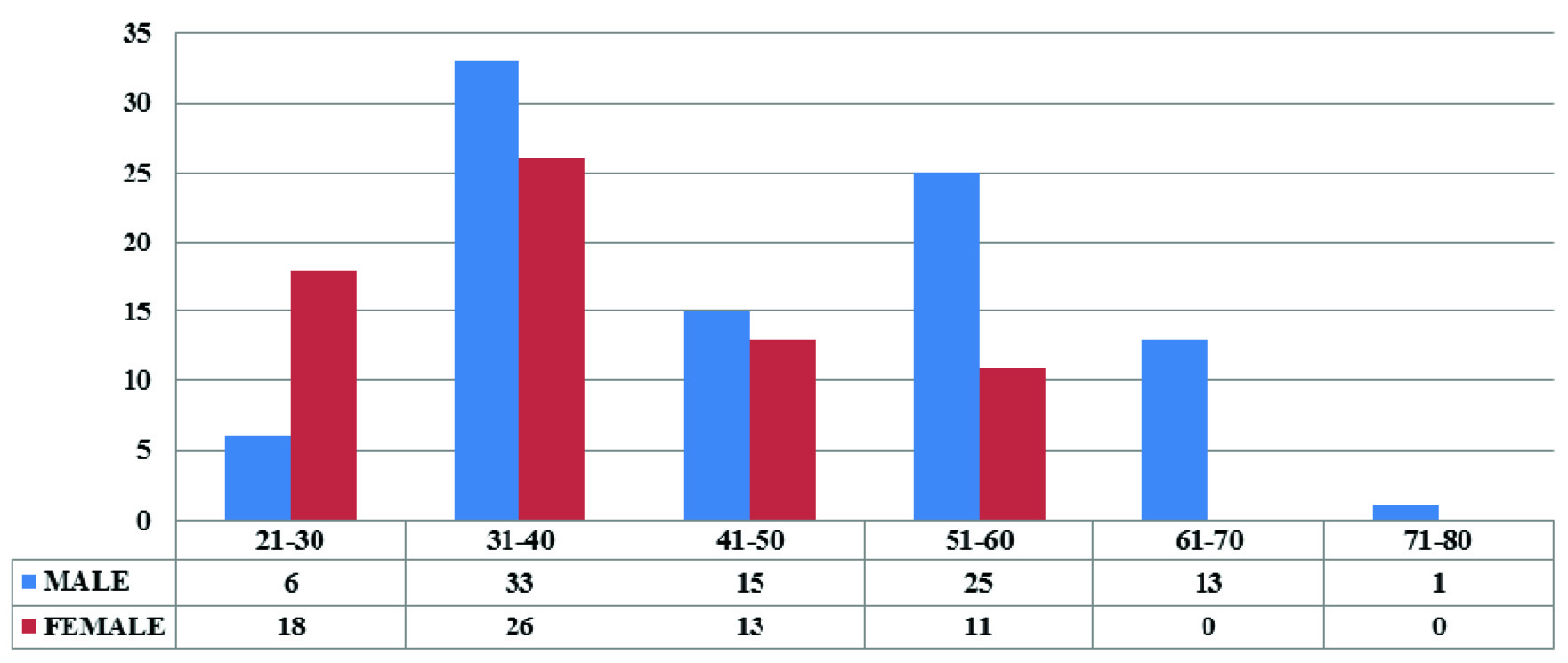
From 2011 to 2016 total institutional admissions were 20922, out of these 161 (0.77%) patients were retroviral positive. Among these 93 (57.8%) were male and 68 (42.2%) were female. Prevalence was more in the age group of 31-40 years i.e., 59 patients (36.6%) followed by 36 patients (22.4%) in the 51-60 years age group [Table/Fig-1]. In total 57(35.4%) patients were newly detected retroviral positive on admission and 104(64.6%) patients were retroviral positive already taking HAART with mean duration varying between 3 to 6 years and mean CD4 count varied between <100 to >400mm3 [Table/Fig-2]. In 28 (17.4%) patients duration of retroviral disease was 4-5 years followed by 5-6years in 18 (11.2%) patients and one patient was retroviral positive since 10 years [Table/Fig-3,4].
Graph showing prevalence of retroviral positive cases among age groups.
Showing various urological manifestations, duration of HAART, mean CD4 count and HAART regimen.
| Manifestations | New retroviral positive cases on admission | Already on HAART | Mean duration of HAART (Yrs) | Mean CD4 count per mm3 | HAART regimen |
|---|
| Urosepsis | 16 | 34 | 3.8 | <100 | 3TC+NVP+ZDV |
| Urolithiasis | 17 | 27 | 6 | >400 | 3TC+NVP+ZDV |
| Malignancy | 9 | 18 | 3.6 | <200 | 3TC+NVP+ZDV |
| Renal Dysfunction | 11 | 7 | 5.5 | <150 | 3TC+NVP+ZDV |
| Genito urinary tuberculosis | - | 6 | 3 | <100 | EFV+3TC+TDF |
| Others | 4 | 12 | 3 | <200 | 3TC+NVP+ZDV |
Others- Stricture urethra, Voiding dysfunction and Amyloidosis. HAART-Highly active anti-retroviral therapy, 3TC-Lamivudine, NVP-Nevirapine, ZDV-Zudovudine, EFV-Efavirenz, TDF-Tenofovir
Showing total number of HIV positive cases (Newly detected) on admission.
| Sex | Positive on admission(New cases) | Total |
|---|
| Male | 35 | 57 |
| Female | 22 |
Showing duration of HAAART (in years) in already diagnosed retroviral positive cases (old cases-AIDS) on admission.
| Duration (yrs)of HAART in retroviral positive (old cases-AIDS) | 0-1Y | 1-2Y | 2-3Y | 3-4Y | 4-5Y | 5-6Y | 6-7Y | 7-8Y | 8-9Y | 9-10Y | Total |
|---|
| Male | 7 | 9 | 6 | 3 | 16 | 11 | 2 | 2 | 1 | 1 | 104 |
| Female | 5 | 7 | 4 | 5 | 12 | 7 | 2 | 4 | 0 | 0 |
Urological Manifestations
Among 161 retroviral positive cases, most common manifestation was Urosepsis 31% followed by Urolithiasis 27.3%, Malignancy 16.77%, Renal dysfunction 11.18%, Genito-urinary tuberculosis 3.72% and others which include Stricture urethra 7.45%, Voiding dysfunction 1.86% and Amyloidosis 0.62% of cases.
Urosepsis
Out of 161 retroviral positive cases 50 cases manifested with urosepsis among which 16 cases were retroviral positive on admission to hospital and 34 were already on HAART. The most common mode of presentation was pyelonephritis in 18 cases followed by urinary tract infections-15. The common clinical presentation was fever with chills, pain abdomen and hypotension. Mean CD4 count was <100 cells/mm3. On investigations total count was increased and E.Coli was the most common organism isolated on urine culture followed by candida, mixed aerobic and anaerobic growth and no growth in some cases. A total of 28 patients were treated conservatively and 22 patients underwent conventional surgical treatment as per general population with standard theatre precaution during surgery. Mean hospital stay varied between 3 days to 10 days with no mortality [Table/Fig-5].
Showing various intervention in Urosepsis and hospital stay
| Manifestation | Number of cases | Intervention | Mean hospital stay (days) |
|---|
| Pyelonephritis | 18 | DJ stenting-8Conservative-10 | 56 |
| UTI | 15 | Conservative | 3 |
| Psoas Abscess | 5 | Incision & Drainage | 5 |
| Renal Abscess | 4 | Incision & Drainage | 8 |
| Epididymorchitis | 3 | Conservative | 4 |
| Fournier Gangrene | 2 | Debridement | 10 |
| Prostatic Abscess | 1 | TUIP | 7 |
| Testicular Abscess | 1 | Orchiectomy | 3 |
| Periurethral Abscess | 1 | Incision & Drainage | 4 |
DJ stent-Double J stent, TUIP-Trans urethral incision of prostate.
Urolithiasis
A total of 44 Retroviral positive cases had urolithiasis. Seventeen cases were newly diagnosed HIV positive on admission and 27 cases were already on HAART. Thirty cases had ureteric calculus and renal and vesical calculus were present in 10 and 4 cases respectively [Table/Fig-6]. The most common clinical presentation was abdominal pain in 28 cases followed by pain and fever in 5 cases. Mean CD4 count was >400 cells/mm3. Patients with urosepsis underwent surgical intervention after control of sepsis. All patients with urolithiasis underwent surgical procedures with standard operation theatre precautions with mean hospital stay varying between 2 days to 7 days with no mortality [Table/Fig-7]. Most calculi on evaluation were Calcium Oxalate.
Urolithiasis in retroviral cases.
| Incidence of calculus | Ureteric calculus | Renal calculus | Vesical calculus |
|---|
| Male | 17 | 7 | 4 |
| Female | 13 | 3 | 0 |
Various interventions done in urolithiasis patients and hospital stay
| Manifestation | No.of cases | Intervention | Mean hospital stay (days) |
|---|
| Urolithiasis | 44 | URSL+ DJ stenting- 21DJ- 9PCNL- 5PCN- 4Cystolithotomy- 2Cystolitholapaxy- 2Pyelolithotomy- 1 | 3453427 |
URSL-Ureteroscopic Lithotripsy, DJ stent-Double J stent, PCNL-percutaneous nephrolithotomy, PCN-percutaneous nephrostomy.
Malignancies
A total of 27 cases had malignancy with Carcinoma Cervix as most common manifestation in 13 cases followed by Carcinoma Bladder-8. Most common clinical presentation was Obstructive Uropathy in 15 cases. Mean CD4 count was <200 cells/mm3. All cases underwent surgical intervention with hospital stay between 2 days to 8 days with nil mortality. The final histopathological reports after surgery were transitional cell carcinoma in carcinoma bladder, squamous cell carcinoma in carcinoma penis, cervix and vagina and clear cell renal cell carcinoma in renal cell carcinoma [Table/Fig-8,9].
Incidence of malignancies in retroviral cases.
| Malignancy | Carcinoma bladder | Carcinoma penis | Renal cell carcinoma | Carcinoma cervix | Carcinoma vagina |
|---|
| Male | 6 | 3 | 1 | 0 | 0 |
| Female | 2 | 0 | 0 | 13 | 2 |
Surgical interventions done in malignancies and hospital stay
| Manifestations | No. of cases | Intervention | Mean hospital stay(days) |
|---|
| Carcinoma bladder | 8 | TURBT | 6 |
| Carcinoma penis | 3 | Partial Pennectomy | 3 |
| Renal cell carcinoma | 1 | Radical Nephrectomy | 8 |
| Carcinoma cervix | 13 | Dj Stenting | 2 |
| Carcinoma vagina | 2 | Dj Stenting | 2 |
TURBT-Trans urethral resection of bladder tumour, DJ stent-Double J stent
Renal Dysfunction
Among 18 Patients with renal dysfunction on dialysis, 11 cases were retroviral positive on admission and seven were already on HAART with mean duration of HAART 5.5 years. Mean CD4 count was <150 cells/mm3. All of them referred from nephrology for vascular access. Renal biopsy showed Nephritis. All patients underwent arterio-venous fistula creation under strict theatre precautions with one day hospital stay.
Genito-Urinary Tuberculosis
Six cases had genito-urinary tuberculosis. Out of which five cases presenting as obstructive uropathy underwent DJ stenting and one case had tubercular testis treated by simple Orchiectomy [Table/Fig-10]. Two cases in obstructive uropathy had active pulmonary tuberculosis as sputum examination showed AFB positive. Mean CD4 count was < 100cells/mm3 and mean hospital stay was six days with no mortality.
Genitourinary tuberculosis manifestations.
| Manifestations | Ureteric stricture | Testis |
|---|
| Male | 2 | 1 |
| Female | 3 | 0 |
Other Manifestations
Among 16 patients, four were detected retroviral positive on admission and 12 were already on HAART with mean duration of HAART was three years. Mean CD4 count was <200 cells/mm3. They clinically presented with dysuria, thinning and reduced urinary stream and increased urinary frequency. On radiological evaluation, diagnosed to have stricture urethra. Eight cases underwent direct visual internal urethrotomy as stricture was short segment, thin with less spongiofibrosis on palpation, present at proximal bulbar urethra. Three cases under went buccal mucosal graft urethroplasty for long segment anterior urethral stricture and in one case staged urethroplasty was done for pan anterior urethral stricture. Mean hospital stay varied from 5 days to 10 days. Three patients had voiding dysfunction with sterile urine underwent urodynamic study and found to have overactive bladder treated with anti-cholinergic. One patient underwent TURBT for bladder growth presenting clinically as hematuria. Histopathological examination reported as amyloidosis and hospital stay was five days [Table/Fig-11].
Surgical interventions done in other manifestations and hospital stay
| Manifestations | No.of cases | Intervention | Mean hospital stay (days) |
|---|
| Stricture urethra | 12 | DVIU- 8BMG Urethroplasty- 3Staged Urethroplasty- 1 | 4105 |
| Voiding dysfunction | 3 | UDS | 2 |
| Amyloidosis | 1 | TURBT | 5 |
DVIU-Direct Visual Internal Urethrotomy, BMG-Buccal Mucosal Graft, UDS-Urodynamic Study, TURBT-Trans Urethral Resection of Prostate
Between June 2011 and May 2016, a total of 4060 non HIV-AIDS patients were admitted with similar urological manifestations as that of HIV-AIDS positive patients in our study. These patients underwent treatment modality for respective urological disease similar to HIV-AIDS patients without mortality and there mean hospital stay was same as that of HIV-AIDS patients [Table/Fig-12].
Mean hospital stay of HIV-AIDS and non HIV-AIDS patients
| Manifestations | HIV-AIDS patients | Mean hospital stay (days) | Non HIV-AIDS patients | Mean hospital stay(days) |
|---|
| Urosepsis | 50 | 5.5 | 50 | 6 |
| Urolithiasis | 44 | 3 | 680 | 4 |
| Malignancy | 27 | 2 | 170 | 2 |
| Renal Dysfunction | 18 | 1 | 2500 | 1 |
| Genito urinary tuberculosis | 6 | 6 | 110 | 7 |
| Stricture urethra | 16 | 6.3 | 550 | 7 |
Discussion
Urologic disorders are often the first clinical signs that indicate possible HIV infection [4].
In our study the most common presentation was urosepsis in 50 cases of the study population. The most common mode of presentation is pyelonephritis in 18 cases followed by UTI in 15 cases and the mean CD4 count is <100 cells/mm3. On urine culture Escherichia coli was the most common organism isolated followed by candida, mixed aerobic and anaerobic growth and no growth in some case. Twenty eight patients were treated conservatively and 22 patients underwent conventional surgical procedures as per general population with standard theatre precautions during surgery. The result of this finding was in consonance with a similar study carried out in Calaber, Nigeria which recorded a prevalence of 25.3% [14] while a much higher prevalence of UTI 48.7% was recorded in South Africa [15]. These findings agreed that UTIs are higher in retroviral positive individuals than retroviral negative individuals with CD4 count <200 cells/mm3 with Escherichia coli as the most common isolated organism [15].
In our study 104 (64.6%) patients were taking HAART-regimen (3TC+NVP+ZDV) with mean duration of treatment four years. A 57(35.4%) patients were newly diagnosed on screening and referred to ART center. In the present study the incidence of urolithiasis was 7.32% with calcilum oxalate being the most common on stone analysis. According to Hoffmann C and Mulcahy F, and Meraviglia P et al., Indinavir caused urolithiasis in 5–25% of HIV positive patients treated with the drug [16,17]. In the present study non of the drugs of HAART regimen are known to cause crystaluria and stone formation [18].
In patients with HIV on HAART there has been an increase in the incidence of non-AAMs (AIDS-Associated Malignancies) including anal cancer, lung cancer, hepatocellular carcinoma, vaginal cancer, leukemia, oropharyngeal cancer, colorectal cancer, penile cancer, and renal cancer [19-23]. In our study the most common malignancy was carcinoma cervix 13 (19.11%) followed by carcinoma bladder 8(8.6%).
Renal dysfunction in patients with HIV can be caused by nephrotoxic medications such as antibiotics and antifungals, metabolic dysfunction and volume depletion as a result of chronic diarrhea, uretheral obstruction from malignancy, infections, and intrinsic diseases such as HIV-Associated Nephropathy (HIVAN), which occurs in 10–30% of patients with HIV [24]. In our study, 18 (11.18%) patients were referred from nephrology for vascular access. Renal biopsy showed Nephritis.
Hospital stay was similar to that of general population admitted with similar manifestations as that of HIV and AIDS patients during the study period [Table/Fig-13] [25-31]. Coelho LE et al., have shown that the length of hospital stay in AIDS related and non-AIDS related events is almost similar [32].
Urological manifestations in other studies with respect to our study [25-31]
| Manifestations | Our Study | Mean CD4 count(cells/cumm) | Other studies | Mean CD4 count(cells/cumm) |
|---|
| UROSEPSISPyelonephritisUTI | 11.18%9.3% | <100 | 19.35% [26]17% [27] | 100<500 |
| UROLITHIASIS | 27.32% | >400 | 5-22% [28] | 300 |
| MALIGNANCYCa.cxCa.bladderpenile cancer | 8.0%(n=13/161),4.9% (n=8/161)1.86%(n=3/161) | <200 | 14.1% (n=20/141) [29]3.8% (n=1/26)7.6% (n=2/26) | 257 |
| RENAL DYSFUNCTION | 11.18% | <150 | 15.5% (n=192/1239) [30] | 200 |
| GUTB | 3.10% | <100 | 12.5% [31] | 150 |
| STRICTURE URETHRA | 7.45% | <200 | 37.5% [32] | <400 |
Conclusions
In our study, urosepsis is the most commonest presentation followed by urolithiasis with CD4 count between <100 cells/mm3 and CD 4 >400 cells/mm3 respectively. With timely diagnosis and prompt treatment of urological disorders, the outcome and prognosis is same as that of general population.
Others- Stricture urethra, Voiding dysfunction and Amyloidosis. HAART-Highly active anti-retroviral therapy, 3TC-Lamivudine, NVP-Nevirapine, ZDV-Zudovudine, EFV-Efavirenz, TDF-Tenofovir
[1]. Ho DD, Neumann AU, Perelson AS, Chen W, Leonard JM, Markowitz M, Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infectionNature 1995 373:123-26.10.1038/373123a07816094 [Google Scholar] [CrossRef] [PubMed]
[2]. Wei X, Ghosh SK, Taylor ME, Johnson VA, Emini EA, Deutsch P, Viral dynamics in human immunodeficiency virus type –1 infectionNature 1995 373:117-22.10.1038/373117a07529365 [Google Scholar] [CrossRef] [PubMed]
[3]. Levy JA, The transmission of HIV and factors influencing progression to AIDSAm J Med 1993 95:86-100.10.1016/0002-9343(93)90237-J [Google Scholar] [CrossRef]
[4]. Critchlow CW, Kiviat NB, Detection of human immunodeficiency virus type 1 and type 2 in the female genital tract: implications for the understanding of virus transmissionObstet Gynecol Surv 1997 52:315-25.10.1097/00006254-199705000-000249140133 [Google Scholar] [CrossRef] [PubMed]
[5]. Heyns CF, Groeneveld AE, Sigarroa NB, Urologic complications of HIV and AIDSNat Clin Pract Urol 2009 6(1):32-43.10.1038/ncpuro127319132004 [Google Scholar] [CrossRef] [PubMed]
[6]. Zouiten F, Bacterial infections in AIDS (mycobacterial infections excluded): study of 100cases [French]Tunis Med 2003 81:113-20. [Google Scholar]
[7]. Wise GJ, Shteynshlyuger A, How to diagnose and treat fungal infections in chronic prostatitisCurr Urol Rep 2006 7(4):320-28.10.1007/s11934-996-0012-216930504 [Google Scholar] [CrossRef] [PubMed]
[8]. Spano JP, Costagliola D, Katlama C, Mounier N, Oksenhendler E, Khayat D, AIDS-related malignancies: state of the art and therapeutic challengesJ Clin Oncol 2008 26(29):4834-42.10.1200/JCO.2008.16.825218591544 [Google Scholar] [CrossRef] [PubMed]
[9]. Lallemand F, Salhi Y, Linard F, Giami A, Rozenbaum W, Sexual dysfunction in 156 ambulatory HIV-infected men receiving highly active antiretroviral therapy combinations with and without protease inhibitorsJ Acquir Immune Defic Syndr 2002 30(2):187-90.10.1097/00126334-200206010-0000712045681 [Google Scholar] [CrossRef] [PubMed]
[10]. Lee LK, Dinneen MD, Ahmad S, The urologist and the patient infected with human immunodeficiency virus or with acquired immunodeficiency syndromeBJU Int 2001 88:500-10.10.1046/j.1464-410X.2001.02376.x11678742 [Google Scholar] [CrossRef] [PubMed]
[11]. Lewden C, May T, Rosenthal E, Burty C, Bonnet F, Costagliola D, Changes in causes of death among adults infected by HIV between 2000 and 2005: the ‘Mortalite 2000 and 2005’ surveys (ANRS EN19 and Mortavic)J Acquir Immune Defic Syndr 2008 48(5):590-98.10.1097/QAI.0b013e31817efb5418645512 [Google Scholar] [CrossRef] [PubMed]
[12]. Van Sighem A, Gras L, Reiss P, Brinkman K, Wolf F, Life expectancy of recently diagnosed asymptomatic HIV-infected patients approaches that of uninfected individualsAIDS 2010 24(10):1527-35.10.1097/QAD.0b013e32833a394620467289 [Google Scholar] [CrossRef] [PubMed]
[13]. Nakagawa F, Lodwick RK, Smith CJ, Smith R, Cambiano V, Lundgren JD, Projected life expectancy of people with HIV according to timing of diagnosisAIDS 2012 26(3):335-43.10.1097/QAD.0b013e32834dcec922089374 [Google Scholar] [CrossRef] [PubMed]
[14]. Samuel SO, Salami TAT, Adewuyi GM, Babatope E, Ekozien MI, Prevalence of Urinary Tract Infections among a cohort of HIV Positive Patients accessing care in a rural health centre in NigeriaJ Microbiol Biotech Res 2012 2(4):507-10. [Google Scholar]
[15]. Iweriebor BC, Obi CL, Akinyemi O, Ramalivhana NJ, Hattori T, Okoh A, Uropathogens isolated from HIV-infected patients from Limpopo Province, South AfricaAfri J of Biotechnol 2012 11(46):10598-604.10.5897/AJB10.2413 [Google Scholar] [CrossRef]
[16]. Hoffmann C, Mulcahy F, ART 2006. In: Hoffmann C, Rockstroh JK, Kamps SB, editorsHIV medicine 2006. Paris, Cagliari, Wuppertal: Flying 2006 :284-5.Available at: http://www. HIVMEDICINE.com. Accessed May 20, 2007 [Google Scholar]
[17]. Meraviglia P, Angeli E, Del Sorbo F, Rombolà G, Viganò P, Orlando G, Risk factors for indinavir-related renal colic in HIV patients: predictive value of indinavir dose/body mass indexAIDS 2002 16(15):2089-93.10.1097/00002030-200210180-0001912370513 [Google Scholar] [CrossRef] [PubMed]
[18]. Agu KA, Oparah AC, Adverse drug reactions to antiretroviral therapy: Results from spontaneous reporting system in NigeriaPerspect Clin Res 2013 4(2):117-24.10.4103/2229-3485.11178423833736 [Google Scholar] [CrossRef] [PubMed]
[19]. Nutankalva L, Wutoh AK, McNeil J, Frederick WR, Reddy RB, Daftary M, Malignancies in HIV: pre- and post-highly active antiretroviral therapyJ Natl Med Assoc 2008 100(7):817-20.10.1016/S0027-9684(15)31375-4 [Google Scholar] [CrossRef]
[20]. Mayor AM, Gómez MA, Ríos-Olivares E, Hunter-Mellado RF, AIDS-defining neoplasm prevalence in a cohort of HIV-infected patients, before and after highly active antiretroviral therapyEthn Dis 2008 18(202):S2189-94. [Google Scholar]
[21]. Lewden C, May T, Rosenthal E, Burty C, Bonnet F, Costagliola D, ANRS EN19 Mortalité Study Group and Mortavic. Changes in causes of death among adults infected by HIV between 2000 and 2005: the “Mortalité 2000 and 2005” surveys (ANRS EN19 and MortavicJ Acquir Immune Defic Syndr 2008 48(5):590-98.10.1097/QAI.0b013e31817efb5418645512 [Google Scholar] [CrossRef] [PubMed]
[22]. Patel P, Hanson DL, Sullivan PS, Novak RM, Moorman AC, Tong TC, Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992–200Ann Intern Med 2008 148(10):728-36.10.7326/0003-4819-148-10-200805200-0000518490686 [Google Scholar] [CrossRef] [PubMed]
[23]. Spano J-P, Costagliola D, Katlama C, Mounier N, Oksenhendler E, Khayat D, AIDS-related malignancies: state of the art and therapeutic challengesJ Clin Oncol 2008 26(29):4834-42.10.1200/JCO.2008.16.825218591544 [Google Scholar] [CrossRef] [PubMed]
[24]. Rieke A, HIV and renal function: In HIV Medicine 2007 :567-80.[http://www.hivmedicine.com/hivmedicine2007.pdf] [Google Scholar]
[25]. Xavier TF, Auxilia A, Kannan M, Isolation and characterization of UTI pathogens from HIV positive patients of Karur District, Tamil Nadu, IndiaInt J Curr Microbiol App Sci 2015 4(1):558-63. [Google Scholar]
[26]. Hoepelman AI, van Buren M, van den Broek J, Borleffs JC, Bacteriuria in men infected with HIV-1 is related to their immune status (CD4+ cell count)AIDS 1992 6(2):179-84.10.1097/00002030-199202000-000061348416 [Google Scholar] [CrossRef] [PubMed]
[27]. Brodie SB, Keller MJ, Ewenstein BM, Sax PE, Variation in incidence of indinavir associated nephrolithiasis among HIV-positive patientsAIDS 1998 12:2433-37.10.1097/00002030-199818000-000129875581 [Google Scholar] [CrossRef] [PubMed]
[28]. Petoumenos K, Hui E, Kumarasamy N, Kerr SJ, Choi JY, Chen Y-M, Cancers in the TREAT Asia HIV Observational Database (TAHOD): a retrospective analysis of risk factorsJournal of the International AIDS Society 2010 13:51https://doi.org/10.1186/1758-2652-13-5110.1186/1758-2652-13-5121143940 [Google Scholar] [CrossRef] [PubMed]
[29]. Wyatt CM, Winston JA, Malvestutto CD, Fishbein DA, Barash I, Cohen A, Chronic kidney disease in HIV infection: an urban epidemicAIDS 2007 21(15):2101-03.10.1097/QAD.0b013e3282ef1bb417885301 [Google Scholar] [CrossRef] [PubMed]
[30]. Figueiredo AA, Lucon AM, Júnior RF, Ikejiri DS, Nahas WC, Srougi M, Urogenital tuberculosis in immunocompromised patientsInternational Urology and Nephrology 2009 41:32710.1007/s11255-008-9436-618649001 [Google Scholar] [CrossRef] [PubMed]
[31]. Getahun GM, Chane D, Urethral stricture and HIV: unusual presentations and treatment challengeAfrican Journal of Urology 2010 16(4):124-27.10.1007/s12301-010-0026-3 [Google Scholar] [CrossRef]
[32]. Coelho LE, Ribeiro SR, Veloso VG, Grinsztejn B, Luz PM, Hospitalization rates, length of stay and in-hospital mortality in a cohort of HIV infected patients from Rio de Janeiro, BrazilBraz J Infect Dis 2017 21(2):190-95.10.1016/j.bjid.2016.10.00727918889 [Google Scholar] [CrossRef] [PubMed]