Odontogenic Fibroma Associated with an Impacted Tooth
Reema Talat Ayesha1, Balaji Pachipulusu2, Poornima Govindaraju3, Sanjana Ravindra4
1 Postgraduate, Department of Oral Medicine and Radiology, Raja Rajeswari Dental College and Hospital, Bangalore, Karnataka, India.
2 Professor and Head, Department of Oral Medicine and Radiology, Raja Rajeswari Dental College and Hospital, Bangalore, Karnataka, India.
3 Professor, Department of Oral Medicine and Radiology, Raja Rajeswari Dental College and Hospital, Bangalore, Karnataka, India.
4 Postgraduate, Department of Oral Medicine and Radiology, Raja Rajeswari Dental College and Hospital, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Reema Talat Ayesha, Postgraduate, Department of Oral Medicine and Radiology, Ramohalli Cross, Mysore Road, Raja Rajeswari Dental College and Hospital, Bangalore-560098, Karnataka, India.
E-mail: reematayesha@gmail.com
Central Odontogenic Fibroma (COF) is an extremely rare benign tumour caused by proliferation of mature odontogenic mesenchyme that accounts for 0.1%-0.5% of all odontogenic tumours. It has a female predilection and often affects patients in between 2nd and 4th decade. Mandible is more commonly affected than maxilla. Clinically, it presents as a slow growing, asymptomatic, swelling which may cause expansion of cortical plates. Radiographically, it presents as a unilocular or multilocular radiolucency, with large lesions showing scalloped margins. Few cases show occurrence of calcification in the form of flecks and may be associated with an unerupted tooth. Histological appearance is characterized by presence of small inactive odontogenic islands in matrix of collagenous connective tissue with variable amounts of calcification. Typical conservative surgical intervention includes enucleation and curettage with good prognosis. Here we present a case of Odontogenic Fibroma in a 25-year-old female involving the maxilla.
Benign lesion, Calcification, Impacted tooth, Odontogenic fibroma, Pericoronal radiolucency
Case Report
A 25-year-old female complained of a swelling in her upper front teeth region since one year. She noticed a swelling one year back which was insidious in onset, initially small in size and had gradually progressed to the current size. It was not associated with any history of trauma, pain, paresthesia, discharge or epistaxis. No other associated symptoms were present. Patient consulted a dentist earlier, underwent radiographic examination and extraction of retained upper deciduous tooth after which she was referred for further evaluation of swelling. Medical history, drug history, family history and habit history were noncontributory. Patient was moderately built and nourished with all vitals within normal limits.
On extra oral examination, gross facial asymmetry was noticed due to a diffuse swelling measuring approximately 2×3 cm extending superoinferiorly from left infraorbital rim up to alatragal line and mediolaterally from left ala of nose up to 3 cm away from it. Obliteration of the left nasolabial fold was present with skin over the swelling and surrounding area appearing normal [Table/Fig-1a,b]. On palpation, all the inspectory findings were confirmed with no local rise in temperature. It was firm and non-tender with no regional lymphadenopathy.
On intra oral examination of the lesion proper, soft tissue examination revealed a diffuse swelling present in left anterior portion of hard palate measuring approximately 1.5×2 cm, extending anteroposteriorly from lingual aspect of #21 region to mesial aspect of #25, and mediolaterally from 0.5 cm away from mid palatal raphae to attached gingiva of #23 #24 [Table/Fig-2]. The overlying mucosa appeared normal. On palpation, swelling was firm in consistency, non-tender with no yielding points present and expansion of buccal and palatal cortical plate.
Other findings include, clinically missing #22 and healing extraction socket irt #62 region. Based on the history, clinical examination and on the basis of a possibly impacted tooth, a provisional diagnosis of Dentigerous cyst associated with an impacted #22 was made. Differential diagnoses of Adenomatoid Odontogenic Tumour on the basis of its location, odontogenic keratocyst due to its prevalence, ameloblastoma and odontogenic fibroma (rare) were considered.
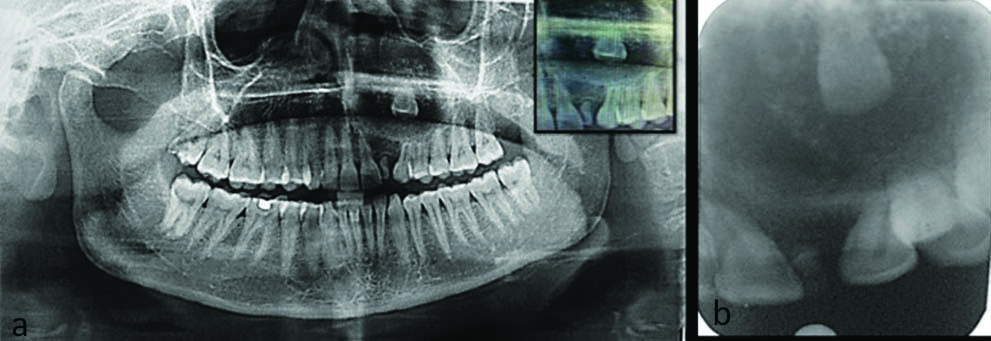
Intraoral Periapical Radiograph (IOPAR) and Orthopantomogram were done one week prior by the previously consulted dentist before doing the extraction. They revealed a well-defined radiolucency with calcifications surrounding the crown of the impacted tooth structure extending from the cervical third of the tooth with its superior limit being beyond the limit of the radiograph. A retained deciduous #62 and diffuse radiolucency involving enamel, dentin and approximating pulp was present irt #18 [Table/Fig-3a,b].
a) Facial asymmetry with a swelling on the left middle third region of face; b) Swelling as seen from inferior aspect with obliteration of left nasolabial fold present.

Intraoral clinical picture.

a) Orthopantomogram showing well defined solitary radiolucency present with calcifications and impacted tooth Inset: Crown of impacted tooth surrounded by calcifications; b) IOPAR revealing retained deciduous 62 with an impacted tooth visible superiorly.
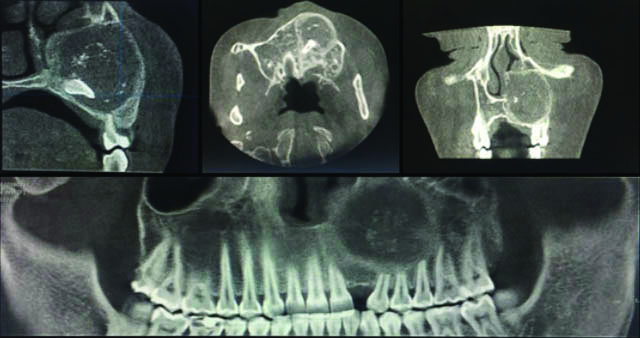
To ascertain the clear extent of the lesion and its effect on surrounding structures, a 3D imaging modality of CBCT was advised. CBCT revealed a solitary, unilocular radiolucency present with a sclerotic rim in left maxillary sinus region measuring 27.89×29.39 mm in its greatest dimensions [Table/Fig-4]. It extended medially till the lateral wall of nose and laterally till medial wall of sinus, superiorly up to the infraorbital margin and inferiorly till the root apex of #23 #24 #25 #26. Radiopaque flecks were present in center of radiolucency surrounding crown of impacted tooth. External root resorption was seen irt #23 #24 #25 #26 in multiplanar fashion. A radiographic diagnosis of adenomatoid odontogenic tumour irt left maxilla associated with an impacted tooth was given with a differential diagnosis of calcifying epithelial odontogenic tumour and central odontogenic fibroma irt left maxilla due to the presence of radiopaque flecks surrounding the crown of impacted tooth.
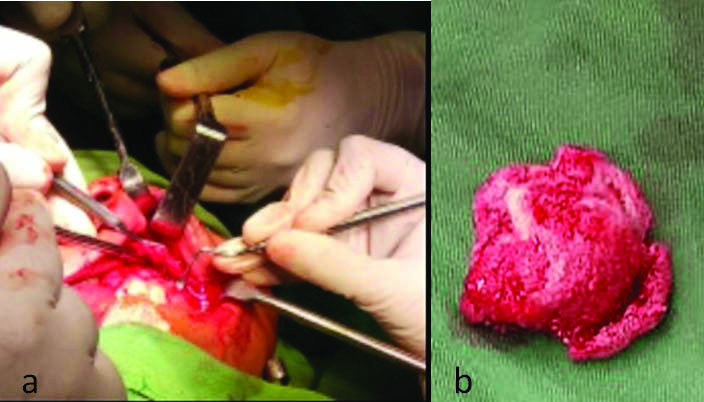
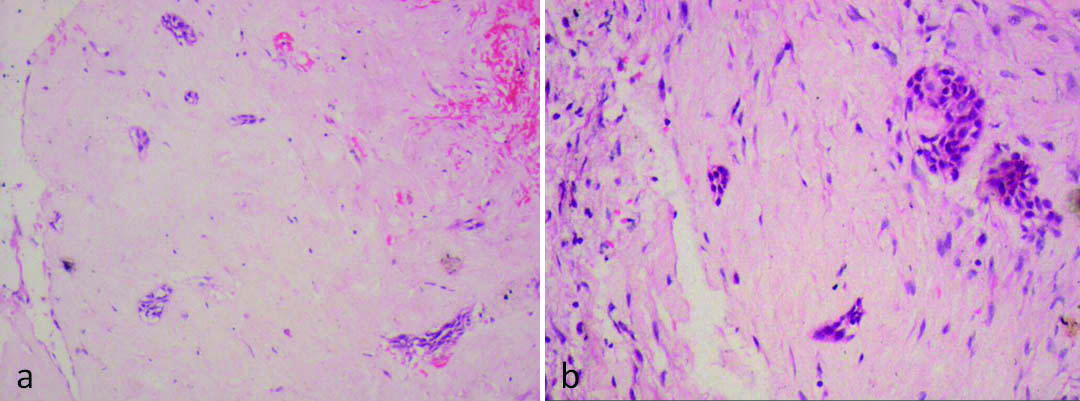
All hematological investigations were found to be within normal limits. The treatment included enucleation of the lesion followed by antibiotic (Amoxicillin 500 mg) and analgesic (Diclofenac 50 mg) therapy [Table/Fig-5a,b]. Histopathological evaluation (H&E section) of specimen revealed areas of cellular connective tissue with fibroblastic area along with areas of low cellularity. Foci of calcification were present with small islands of odontogenic epithelium dispersed in the connective tissue [Table/Fig-6]. The overall features were suggestive of odontogenic fibroma. The absence of ‘tumour droplets’ and duct like structures ruled out Adenomatoidodontogenic tumour whereas calcifying Epithelial Odontogenic Tumour (CEOT) was dismissed due to absence of amyloid-like material.
Cone Beam Computed Tomography slices from L-R (Sagittal, Coronal, Axial and Reformatted Panoramic View) reveal radiopaque flecks in centre of solitary, unilocular radiolucency surrounding crown of impacted tooth with external root resorption irt 23 24 25 26.
a) Surgical Removal of lesion by enucleation; b) Spherical, well circumscribed lesion 2cm x 2cm with a lateral incisor in its substance.
Photomicrograph showing islands of odontogenic epithelium surrounded by fibrous stroma (40x).
Based on clinical presentation and considering all the investigations a final diagnosis of Central Odontogenic Fibroma of left maxilla associated with an impacted tooth was made. Following treatment, there was a naso-antral fistula which was surgically excised and subsequently healed with good prognosis over the following six months.
Informed concent for publishing case report and photographs were obtained from patient.
Discussion
Odontogenic Fibromas are rare mesenchymal tumours with a prevalence of 0.1%-1.5% [1]. The WHO classification in 2017, defined it as “a rare neoplasm of mature fibrous connective tissue, with variable amounts of inactive-looking odontogenic epithelium with or without evidence of calcification” [2]. It has a potential to occur either in intraosseous or extraosseous location. The extraosseous counterpart is designated as Peripheral Odontogenic Fibroma (POF). It can be distinguished from other odontogenic tumours on the basis of its distinct histopathological features and its appearance on radiological investigations. [1] A brief summary of classification has been summarised in [Table/Fig-7] [1-6].
Different classifications of odontogenic fibroma.
| Histological classifications |
|---|
| Gardner, 1980 [3] | Hyperplastic dental follicle-narrow well circum-scribed lesion around a crown of an unerupted tooth having fibrous connective tissue. | Simple type-fibrous neoplasm with collagenous fibrous connective tissue containing inactive-looking odontogenic epithelium | Complex or WHO-type lesion with dysplastic dentine or tissue like cementum, fibrous tissue with myxoid area and sparse or often conspicuous inactive looking odontogenic epithelium | |
| Lukinmaa PL et al., [4];Langlais RP et al., [5] | | Simple Type | Complex or WHO type | Granular cell Type |
| WHO [6] | | Epithelium-poor type | Epithelium-rich type | |
| WHO, 2017 [2] | Subtypes excluded due to inadequate literature |
| Topographical classification [1] | Intraosseous or central | Extra-osseous or peripheral |
With a female predilection of 2.8:1, it commonly occurs in the third and fourth decade of life. It has a slight predilection for the mandible as compared to the maxilla, occurring in the maxillary anterior region of the case discussed [6].
This lesion causes an asymptomatic expansion of the cortical plate of the mandible or maxilla which manifests as swelling of the jaw as seen in this case. The lesion is related to the coronal or radicular portion of the tooth as it arises from the dental germ (dental papilla) or from the periodontal membrane. Mobility and displacement of adjacent teeth is seen in larger lesions.
Radiographically, it has a varied appearance ranging from a well-defined radiolucency, unilocular in smaller and multilocular in larger lesions. Some lesions have been reported to contain radiopaque flecks and were associated with an impacted or unerupted tooth, as was the finding in the current case [5]. The radiographic features may overlap with other fibrous lesions such as adenomatoid odontogenic tumour, odontogenic myxoma, ameloblastic fibroma and desmoplastic fibromas in aggressive cases. The appearance of locules, impacted teeth and calcifications needs to be assessed.
Histopathologically, it is often identified due to the following features: fibroid or myxoid stroma with islands of odontogenic epithelium and calcifications. It has been classified into two types (2015): The epithelium rich (WHO type) and epithelium poor (simple) types. The epithelium rich type lesions demonstrate epithelial islands or strands with typical foci resembling dysplastic cementum, osteoid tissue, or dentin. Whereas the epithelium poor type lesions are less cellular with foci of dystrophic calcifications. Odontogenic epithelium is often present as epithelial nests or epithelial cords [7]. The current case resembled the epithelium poor type of histologic appearance. In 2017, the subtypes were removed due to the poor specificity of literature present [2].
The stark resemblance of the lesion radiographically to a calcifying epithelial odontogenic tumour and mimicking its appearance as seen in this case, can lead clinicians to misdiagnose. Although the common site of occurrence for Odontogenic Fibromas is mandibular molar region, occurrence of similar swelling in uncommon locations should not be overlooked. Only a careful histopathological evaluation can reveal the true nature of this lesion, which eludes sufficient literature with only 100 cases having been published so far. Central odontogenic fibroma responds well to surgical enucleation with vigorous curettage and a long term follow up is advised [8].
Conclusion
The current case highlights the usage of 3D imaging modalities in exemplifying diagnosis of lesions that cannot be diagnosed accurately on clinical observation. Rare entities of mesenchymal tumours such as COF are often not included in chair side diagnoses, and can henceforth be included inclinical differential diagnosis. Despite various investigations, the appearances and features may overlap with other lesions, and only a careful systematic approach can enable us to reach to a final conclusion.
[1]. Pippi R, Santoro M, Patini R, The central odontogenic fibroma: How difficult canbe making a preliminary diagnosisJ Clin Exp Dent 2016 8:e223-25.10.4317/jced.5279527034766 [Google Scholar] [CrossRef] [PubMed]
[2]. Van Heerden WFP, Kusama K, Neville BW, Odontogenic and maxilofacial bone tumours. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg P. edsWHO classification of Head and Neck Tumours 2017 4th edLyonIARC:205-260. [Google Scholar]
[3]. Gardner DG, The central odontogenic fibroma: an attempt at clarificationOral Surg 1980 50:425-32.10.1016/S0030-4220(80)80011-9 [Google Scholar] [CrossRef]
[4]. Lukinmaa PL, Hietanee J, Anttinen J, Ahonen P, Continuous enlarged dental follicles with histologic features resembling the WHO type of odontogenic fibromaOral Surg Oral Med Oral Pathol 1990 70:313-17.10.1016/0030-4220(90)90147-K [Google Scholar] [CrossRef]
[5]. Langlais RP, Langland OE, Nortje CJ, Multilocular radiolucenciesIn: Diagnostic Imaging of the Jaws 1995 BaltimoreWilliams & Wilkins:370-76. [Google Scholar]
[6]. Philipsen HP, Reichart P, Sciubba JJ, van der Waal I, Odontogenic Fibroma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, edsPathology and Genetics of Head and Neck Tumours 2005 LyonIARC Press:315 [Google Scholar]
[7]. Barnes L, Everson JW, Reichart P, Sidransky D, World Health Organization Classification of TumoursPathology and Genetics of Head and Neck Tumours 2005 LyonIARC Press [Google Scholar]
[8]. Shanab HG, Enani NA, Warraich SR, Shata RB, Gorashi ASA, Epithelium rich type central odontogenic fibroma in maxilla a case report and review of literatureJ Dent Health Oral Disord Ther 2017 6(1):0018710.15406/jdhodt.2017.06.00187 [Google Scholar] [CrossRef]