Tuberculosis of Intestine with Concurrent Complex Enterovesical and Enterocutaneous Fistula
Deepak Balachandra1, Hirdaya Hulas Nag2, Puja Sakhuja3, Sandip Barman4
1 Senior Resident, Department of Gastrointestinal Surgery, GB Pant Hospital, New Delhi, India.
2 Professor, Department of Gastrointestinal Surgery, GB Pant Hospital, New Delhi, India.
3 Professor, Department of Pathology, GB Pant Hospital, New Delhi, India.
4 Senior Resident, Department of Pathology, GB Pant Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepak Balachandra, Senior Resident, Department of Gastrointestinal Surgery, GB Pant Hospital, New Delhi-110002, India.
E-mail: deepakbmys@gmail.com
Intestinal tuberculosis is one of the common presentations of tuberculosis. It can manifest with various complications. However, spontaneous development of enterovesical fistula especially in association with colovesical and enterocutaneous fistulae is extremely rare in the era of highly effective Antituberculosis Treatment (ATT). This particular situation poses a management difficulty. Although initial treatment includes medical management, these patients may require some sort of surgical resection and reconstruction. Here, we report the case of a 21-year-old male patient who presented with recurrence of intestinal TB with spontaneous complex ileovesical, sigmoid colovesical and enterocutaneous fistulae. The diagnosis was established with an array of investigations including colonoscopy and biopsy, Contrast Enhanced Computed Tomography (CECT) of the abdomen with fistulogram and cystoscopy. This unusual complex fistula was successfully managed by staged surgical procedure along with ATT.
Anti-tubercular agents, Surgery, Unusual intestinal fistula
Case Report
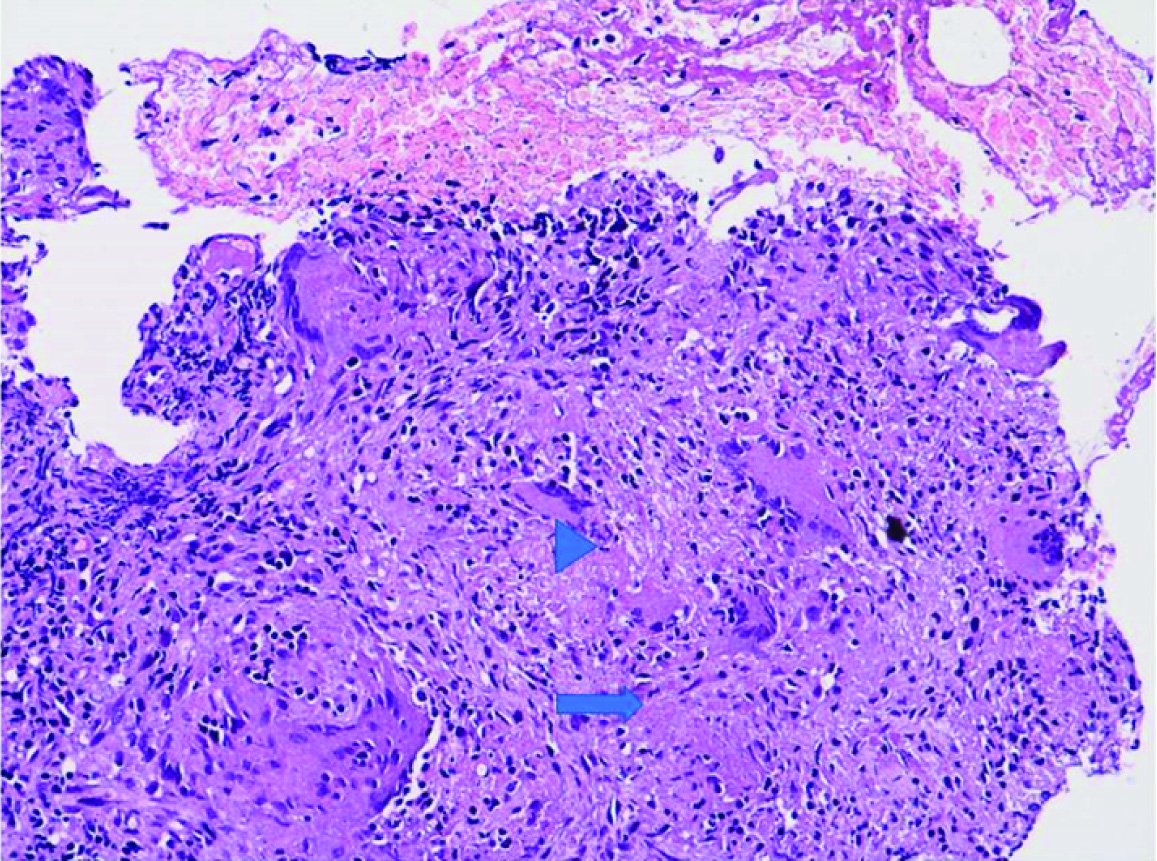
A 21-year-old male patient presented to the Department of Gastrointestinal Surgery with intermittent episodes of fever, colicky type of abdominal pain and presence of a lump in the right lower abdomen of 3 months duration. There was a history of decreased appetite and weight loss (unquantified). On clinical examination, the patient was poorly nourished with 5 x 4 cm non-tender, firm mass felt in the right iliac fossa. On evaluation, ultrasonography abdomen showed a mass in relation to the ileocaecal region and mild ascites. CECT abdomen demonstrated marked thickening of ileum, ileocaecal junction, ascending colon and ascites. Colonoscopy showed ascending colon stricture with ulceration. Histopathological examination of the lesion revealed epithelioid cell granuloma and giant cells [Table/Fig-1]. Chest X-ray was unremarkable. Blood tests showed haemoglobin of 9.2 gm/dL with lymphocyte predominate leucocytosis, erythrocyte sedimentation rate was 120mm/hr and serum ADA was 49.2 units/L. The ascitic fluid analysis was an exudative picture with lymphocyte predominance and fluid Adenosine Deaminase (ADA) level was 53.2 IU/L. With this background, the patient was diagnosed to have intestinal Tuberculosis (TB) and started on Antitubercular Treatment (ATT) under category I. After two months of treatment the patient deferred ATT for a month; however, was again started on category I ATT during the follow up and which was continued for nine months. The patient improved symptomatically with an increase in appetite and weight gain of 10 kg.
HPE of colonscopic biopsy. H&E stain showing epithelioid cell granulomas (arrow); Giant cell (arrow head) H&E 200X.
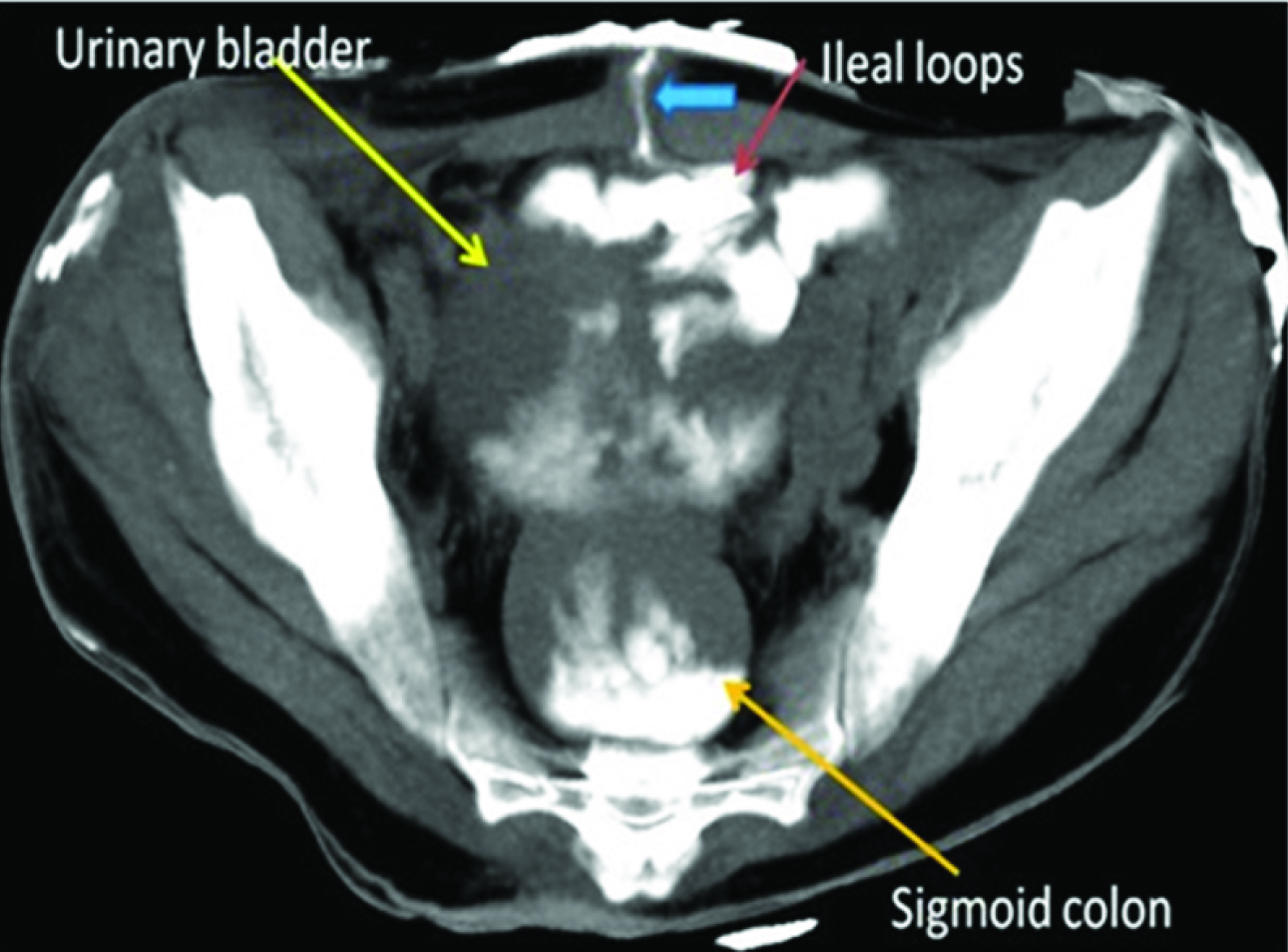
Two months after completion of ATT, the patient presented with fever and painful swelling in right lower abdomen for seven days. There was history suggestive of fecaluria, pneumaturia, and increase in the frequency of micturition for 10 days. On clinical examination, he was febrile with pulse rate of 112/minute, BP of 90/60 mmHg and there was tender fluctuant swelling in right iliac fossa suggestive of an abscess. Blood test showed an elevated leukocyte count of 15600 cells/cumm (4000-11000 cells/cumm). Sample for blood culture was taken and patient started on empirical broad spectrum intravenous antibiotics (Pipercillin Tazobactum, Amikacin and Metronidazole). CECT abdomen showed heterodense lesion noted in the right iliac fossa region with a linear tract extending to another heterodense lesion in the subcutaneous tissue that was surrounded by small bowel, sigmoid colon, omentum and closely abutting the right side of urinary bladder. Incision and drainage of the swelling showed foul smelling purulent discharge. CT abdomen was repeated after five days with fistulogram, revealing ileovesical fistula associated with simultaneous ileocutaneous and sigmoid colovesical fistula [Table/Fig-2]. Following the CT scan, the patient was taken up for laparotomy and diversion ileostomy.
Non contrast image taken through pelvis after injection of iohexol through the fistulous opening in the skin. Image shows the enterocutaneous fistula (blue arrow) communicating with the ileal loops (red arrow) and opacifying the ileal loops. The same contrast spilling into the urinary bladder (yellow arrow) and the sigmoid colon (orange arrow) posteriorly suggestive of enterovesical and vesicocolic fistula.
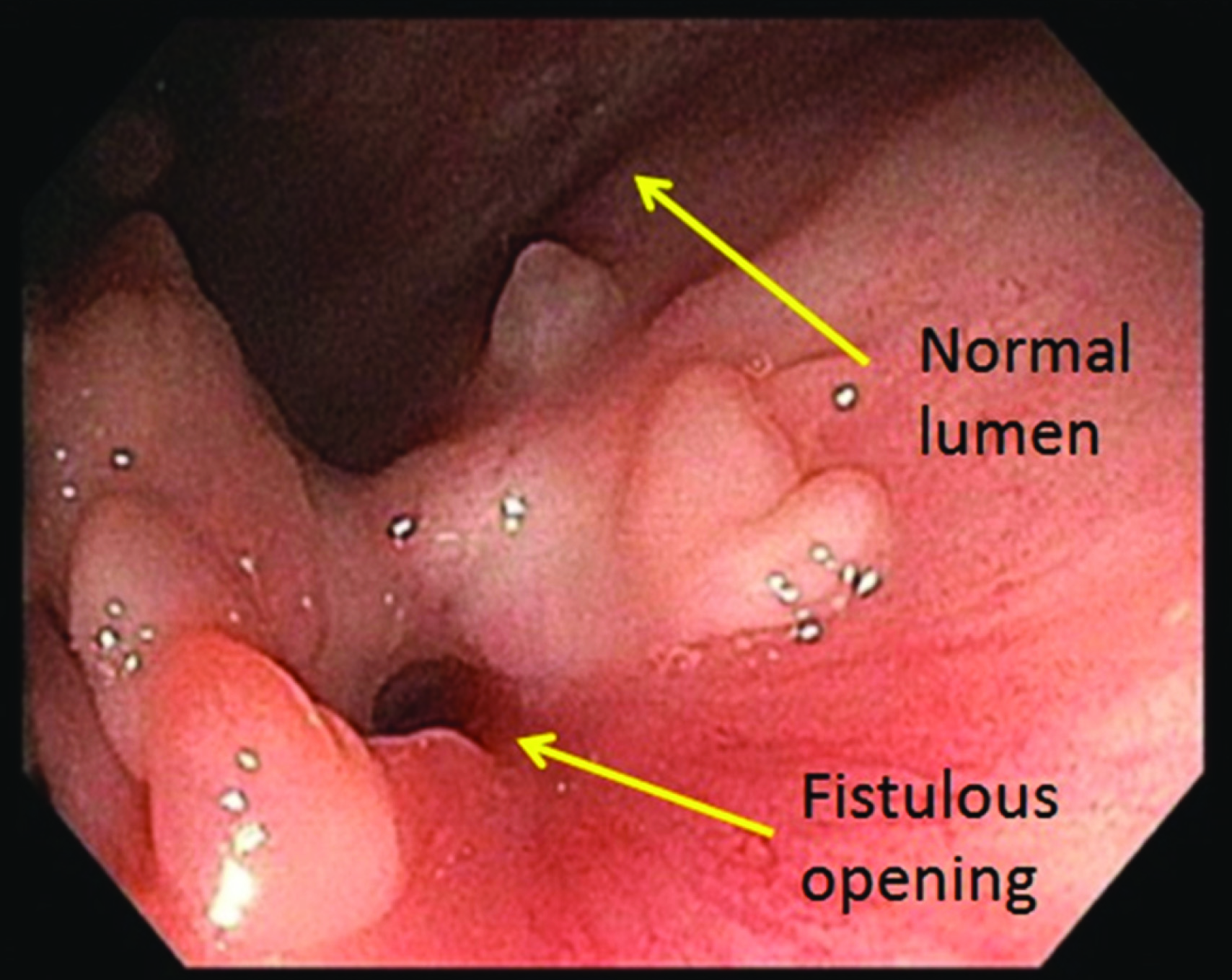
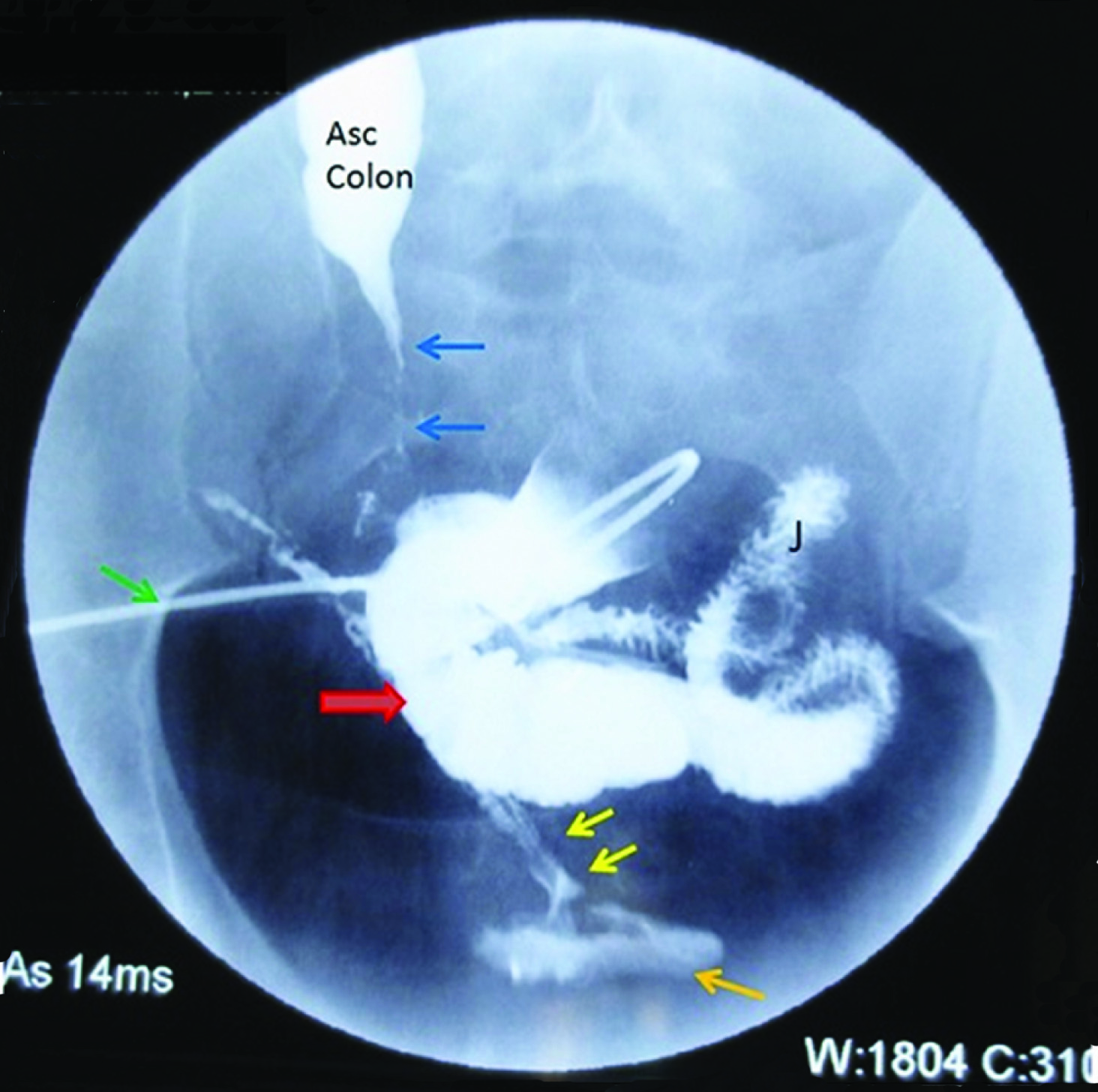
Intraoperatively, there was large inflammatory mass in the pelvis with dense adhesions which were left untouched. There was no peritoneal contamination. In the postoperative period, there was about 400 to 500 mL of urine per day coming out through distal ileal fistula while urine output per urethra was decreased. The patient was started on ATT under category II for disease relapse. Further evaluation with colonoscopy, demonstrated fistulous opening seen in the rectosigmoid junction [Table/Fig-3]. Cystoscopy showed fistulous opening in right posterior wall of the urinary bladder. Distal loopogram done later demonstrated persistent ileovesical fistula [Table/Fig-4]. Six months after bowel diversion along with ATT, he regained his appetite and weight. Meanwhile, urine via distal mucous fistula decreased to minimal but was persistent. In view of the persistent fistula with ileocolic stricture, the patient was subjected to surgery.
Fistulous opening seen in rectosigmoid junction, with scarred surrounding mucosa with multiple 5 mm to 1 cm size nodules seen at 15 cm from anal verge.
Distal loopogram showing catheter (green arrow) inserted into the ileal loop (red arrow). Few jejunal loops (J) are also opacified. Enterovesical fistula (yellow arrows) seen extending from the ileal loops (red arrow) to the urinary bladder (orange arrow). Stricture is also seen in the ascending colon (blue arrows).
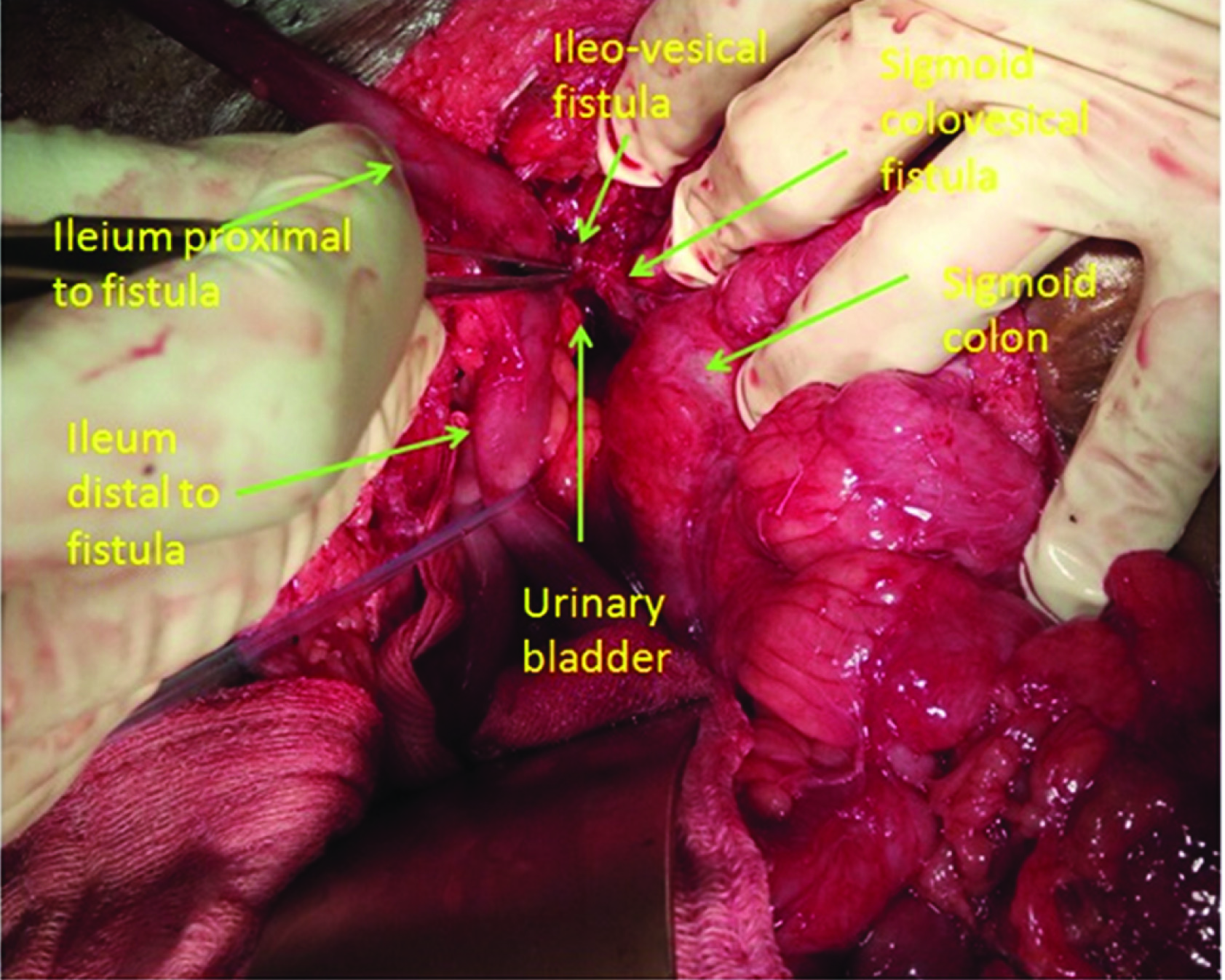
Intraoperatively, the ileocaecal wall was thickened with surrounding dense adhesions. A small fistulous tract was noted between distal ileum and the right posterior wall of the urinary bladder. Another small fistulous tract was noted between the distal sigmoid colon and the right posterosuperior part of the urinary bladder [Table/Fig-5].
Demonstrating ileovesical and sigmoid colovesical fistula.
Right hemicolectomy with ileo transverse anastomosis, sigmoid colon wedge resection and fistula excision with urinary bladder repair was done. Postoperative recovery was uneventful. Foley’s catheter was removed on postoperative day 15 after urinary bladder cystography showed no leak. Patient restored to normal urine flow. Second line ATT was continued. At four-month follow up the patient was doing well.
Discussion
Tuberculosis of intestine is the sixth most common site of extrapulmonary tuberculosis. The frequent site of involvement in bowel is the ileocaecal region, probably related to increased lymphoid tissue and stasis. It usually manifests with various complications such as intestinal obstruction, perforation, bleeding and very rarely enterocutaneous fistula (2.5%) [1,2]. An ileovesical fistula is a rare complication secondary to Crohn’s disease, diverticulitis, appendicitis and non-Hodgkin’s lymphoma. However, tuberculosis is a rare cause of ileovesical fistula [3]. Colovesical fistula is the most common form of the enterovesical fistulae and occurs mostly due to diverticular disease (70-90%), colorectal malignancy (20%) or Crohn’s disease (10%) and rarely due to infections like typhoid fever, amoebiasis, syphilis, tuberculosis [2]. Moreover, simultaneous presentation of complex ileovesical, colovesical and entero-cutaneous fistula is an extremely rare situation which was present in this case. In fact, to the best of our knowledge, this is the first case report describing the spontaneous development of three complex fistulae at the same time.
Pathophysiology behind TB enterovesical fistula is transmural inflammation of bowel causing adherence to adjacent bladder with subsequent erosion and fistula formation. The other mechanism is penetrating ulceration of diseased bowel resulting in contained perforation and formation of an abscess. When abscess necessitates into adjacent viscus (e.g., urinary bladder) or through a cutaneous wound it leads to fistula formation. Although most of the enterovesical fistulae are a result of underlying intestinal disease, predominate manifestations are urological [3]. This is probably related to high bladder compliance and low pressure in the bladder. Therefore, these patients manifest with pneumaturia and fecaluria (50 to 90%) than the flow of urine into the bowel (15%) [4]. Similar presentation was observed in the present patient. Diagnosis of enterovesical fistula is suspected based on clinical manifestation and further confirmed by CECT scan, colonoscopy with ileoscopy, cystoscopy, and barium study. CECT is the most sensitive investigation to diagnose enterovesical fistula. It may show bowel and bladder wall thickening, minimal extraluminal gas and contrast [5]. However, in the present patient, clubbed CECT abdomen with fistulogram clearly demonstrated fistula and its associated communications. Colonoscopy is particularly helpful to diagnose underlying bowel disease and to rule out malignancy. Cystoscopy is the useful method to confirm the diagnosis and to rule out urinary bladder malignancy. The features that suggest fistula communication are localised erythema, papillary/bullous mucosal changes and occasionally, material oozing through and fistula opening [6].
Initial management is done usually by medical treatment including ATT. Surgical management, if a fistula is not healing with ATT. Resection of the diseased bowel and primary repair of the bladder with catheter drainage usually suffice [7]. Similarly, our patient had the persistent fistula in spite of ATT which was successfully managed with the staged surgical procedure.
Conclusion
Concurrent complex ileovesical with colovesical and entero-cutaneous fistula is an extremely rare complication of TB intestine. However, one should suspect this diagnosis in a known case of TB intestine presenting with typical manifestations. Although, ATT is effective in alleviating some of the symptoms and overall improvement, these patients may require surgical resection of the underlying diseased bowel.
[1]. Akinoglu A, Bilgin I, Tuberculous enteritis and peritonitisCan J Surg 1988 31(1):55-58. [Google Scholar]
[2]. Das HS, Panda CR, Singh SP, Misra B, Nayak M, Mallik RN, Colovesical fistula: a rare presentation of colonic tuberculosisWorld Journal of Colorectal Surgery[Internet] 2013[cited 2017 Dec 21] 3(1)Art. 12 [about 5 p]. Available from: http://services.bepress.com/cgi/viewcontent.cgi?article=1117&context=wjcs [Google Scholar]
[3]. Ramchandra N, Mayank V, Sanjeev K, Akshay P, Vaibhav G, Abhishek M, Ileovesical fistula due to tuberculosis: a rare presentationInternational Journal of Health Sciences & Research 2015 5(2):414-17.Available from: http://www.ijhsr.org/IJHSR_Vol.5_Issue.2_Feb2015/61.pdf [Google Scholar]
[4]. Golabek T, Szymanska A, Szopinski T, Bukowczan J, Furmanek M, Powroznik J, Enterovesical fistulae: aetiology, imaging, and managementGastroenterology Research And Practice[Internet] 2013[cited 2017 Dec 21] 2013[ About 8 p]: Available from :https://www.hindawi.com/journals/grp/2013/617967/cta/10.1155/2013/61796724348538 [Google Scholar] [CrossRef] [PubMed]
[5]. Shinojima T, Nakajima F, Koizumi J, Efficacy of 3-D computed tomographic reconstruction in evaluating anatomical relationships of colovesical fistulaInt J Urol 2002 9(4):230-32.[Medline]10.1046/j.1442-2042.2002.00451.x12010319 [Google Scholar] [CrossRef] [PubMed]
[6]. Kwon EO, Armenakas NA, Scharf SC, Panagopoulos G, Fracchia JA, The poppy seed test for colovesical fistula: big bang, little bucks!J Urol 2008 179(4):1425-27.[Medline]0.1016/j.juro.2007.11.08518289575 [Google Scholar] [CrossRef] [PubMed]
[7]. Ferguson GG, Lee EW, Hunt SR, Ridley CH, Brandes SB, Management of the bladder during surgical treatment of enterovesical fistulas from benign bowel diseaseJ Am Coll Surg 2008 207(4):569-72.[Medline]10.1016/j.jamcollsurg.2008.05.00618926461 [Google Scholar] [CrossRef] [PubMed]