Subarachnoid Haemorrhage Following Spinal Anaesthesia in Pregnant Women: A Rare Occurrence
Vineet V Mishra1, Sunita Lamba2, Kavita Mistry3, Ruchika Verneker4
1 Professor and Head, Department of Obstetrics and Gynaecology, Institute of Kidney Diseases and Research Centre, Ahmedabad, Gujarat, India.
2 Clinical Fellow, Department of Obstetrics and Gynaecology, Institute of Kidney Diseases and Research Centre, Ahmedabad, Gujarat, India.
3 Assistant Professor, Department of Obstetrics and Gynaecology, Institute of Kidney Diseases and Research Centre, Ahmedabad, Gujarat, India.
4 Clinical Fellow, Department of Obstetrics and Gynaecology, Institute of Kidney Diseases and Research Centre, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vineet V Mishra, Professor and Head, Department of Obstetrics and Gynaecology, Institute of Kidney Diseases and Research Centre, Asarwa, Ahmedabad, Gujarat, India.
E-mail: vineet.mishra.ikdrc@gmail.com
With the increasing trend of caesarean delivery, spinal anaesthesia is the most common anaesthetic procedure performed today. The most common complication following this procedure is post spinal headache. However, more dreadful and devastating complication like Subarachnoid Haemorrhage can occur and should be considered in case of persistent headache. We present a case of Subarachnoid Haemorrhage (SAH) following spinal anaesthesia in a woman who underwent full-term caesarean section. Post spinal anaesthesia, she had continuous headache and vomiting. On fourth postoperative day, headache was aggravated and imaging studies revealed subarachnoid haemorrhage with intraventricular bleeding. This article discusses the consideration of SAH following dural puncture, its differential diagnosis and management. Post spinal headache should always be evaluated properly taking into consideration the various differential diagnosis of postoperative headache. Dreadful complication like SAH should be timely diagnosed and treated for better outcome.
Intraventricular haemorrhage, Pregnancy, Spinal headache
Case Report
A 27-year-old, primigravida woman underwent lower segment caesarean section for failed induction of labour. Labour induction was done at 38 weeks for intrauterine growth restriction and oligohydroamnios. The anaesthetic registrar performed spinal anaesthesia with the patient in the left lateral position, at the level of the L2/3 interspaces with 23G spinal needle under standard aseptic conditions. Free flow of Clear Cerebrospinal Fluid (CSF) was obtained in second attempt which was followed by slow injection of 2.2ml heavy Bupivacaine. At five minutes, a sensory block to T6 was achieved and caesarean section commenced. Her intraoperative period was uneventful. A healthy baby of 2.53 kg (Apgar 8 at 1 min and 10 at 5 minutes) was delivered. Patient had light headache and vomiting multiple times in immediate post-partum period. Analgesic and antiemetic were given. On day 1 after confirming bowel peristalsis; oral liquid and semisolid diet was started. However, patient was intolerant to oral intake due to vomiting and was thus shifted to intravenous fluid. Complain of vomiting and intolerance to oral intake persisted even on postoperative day 2 and 3. Headache was persistent and patient was anxious. Management in line of paralytic ileus and spinal headache was started. Serum electrolytes were done (serum Sodium 130.6 meq/L and potassium 3.4 meq/L). X-ray abdomen erect showed multiple air filled loops of intestine which was suggestive of paralytic ileus. Ryle’s tube was inserted and potassium supplement was given as advised by gastro surgeon.
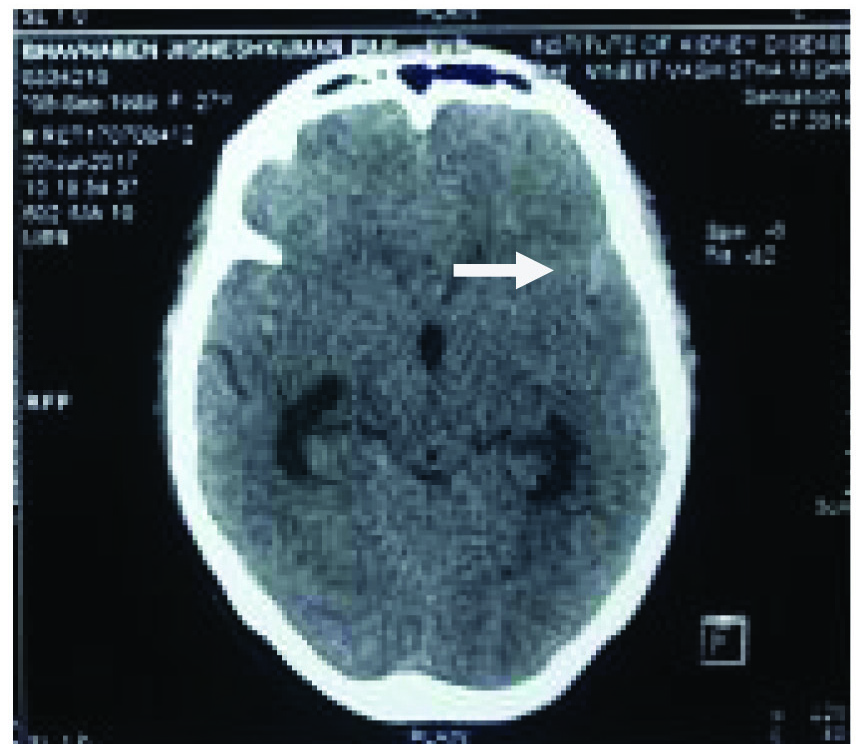
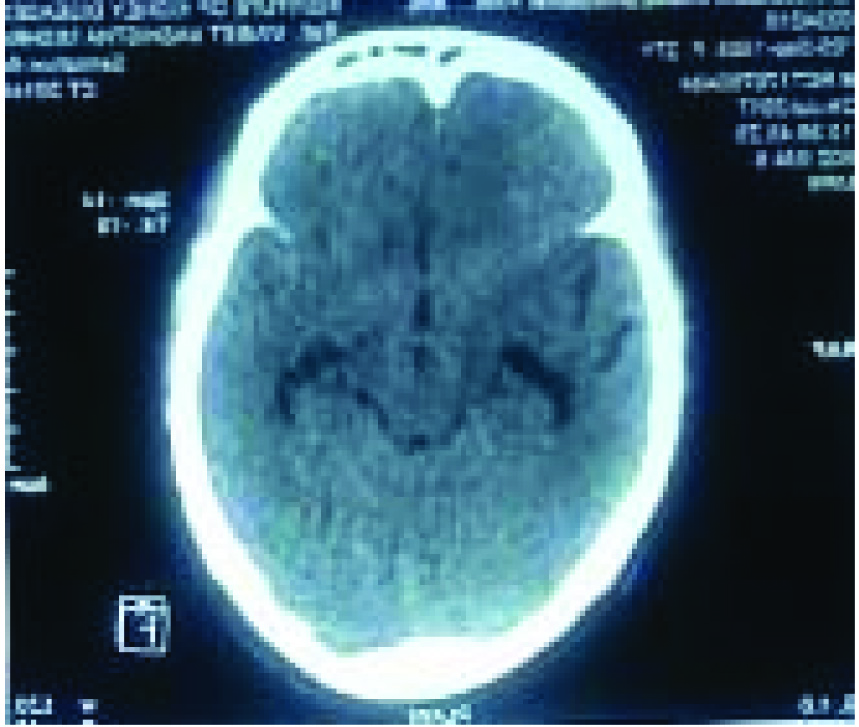
On postoperative day-4 she had a single episode of convulsion which lasted for about 20 seconds. It was associated with frothing from mouth, generalized tonic movements and altered consciousness. She regained consciousness after 5 minutes and complained of severe headache with radiation to occipital and cervical region, along with nausea and uneasiness. On examination, the patient was conscious, well oriented to time, place and person, but looked unwell and distressed. She was afebrile with a pulse rate of 60/min and blood pressure of 138/90 mm/Hg. Neurological examination revealed neck stiffness but there was no sensory and motor deficit. Rest of systemic examination was also normal. ECG was normal. Investigations at that time showed a normal coagulation profile and normal complete blood counts. Renal and liver function tests were also normal. Cranial tomogram was performed which showed Subarachnoid haemorrhage in both Sylvian fissure and in basal cisterns along with mildly dilated ventricular system and cerebral oedema [Table/Fig-1]. Magnetic Resonance (MR) angiography of intracranial arteries did not show any aneurysm and no evidence of acute infarct/ischemic area was seen. The diagnosis of SAH (Grade 2 on the Hunt and Hess Scale) [1] was established. Patient was shifted to critical care unit under neurosurgeon. Patient was kept on Injectable Nimodipine 2 mL/min, injection Mannitol 100cc 6 hourly and injection Furesamide 10 mg 12 hourly. Anti-convulsant drug, injection Levetiracetam 500 mg/8 hourly was started. Blood pressure was maintained according to brain perfusion pressure. Cranial Tomography was repeated after 48 hours which showed mild reduction in hydrocephalus and brain oedema. Same treatment continued and patient showed progressive improvement clinically and thus managed conservatively. Repeat CT scan after 7 days was normal [Table/Fig-2]. Injection Mannitol was tapered off and replaced with oral glycerol. In addition, she recieved oral Nimodipine 60 mg QID. Patient had made an uneventful recovery.
CT scan showing Hyper dense area in sylvian fissure suggestive of Sub Arachnoid haemorrhage.
CT scan showing normal sylvian fissure.
Discussion
Subarachnoid haemorrhage is a dreadful condition, often resulting in severe neurological disability or death. In SAH blood extravasates into the subarachnoid space between the arachnoid membranes and the pia mater. The annual incidence of spontaneous subarachnoid haemorrhage is 2 to 25 per 100,000 people [2]. Incidence of subarachnoid haemorrhage is more common in women [2,3]. The incidence of spontaneous SAH is estimated to be increased five-fold, to 2 in 100,000 deliveries compared with the non-pregnant population, but no reliable data exists [3]. This diagnosis should be considered when assessing obstetric patients with headaches and vomiting after dural puncture.
Rupture of cerebral aneurysm, is the most common cause of non-traumatic subarachnoid haemorrhage (75%), even during pregnancy and postpartum [3]. Risk of aneurysmal SAH increases with maternal age and trimester. The other common causes of SAH in the post-partum period are hypertension, vascular malformation, cerebral venous thrombosis, reversible cerebral vasoconstriction syndrome and idiopathic. Rarer causes include meningeal infection, tumors and blood dyscrasias [4].
Symptoms of SAH include sudden onset of severe headache, vomiting, confusion or a lowered level of consciousness and sometimes seizures [5]. Our patient also presented with these symptoms. In patient, headache and vomiting started 2 hours after spinal anaesthesia. The onset was sudden, persisted for several days with no other associated elements. After exclusion of other causes, CT scan was performed in suspicion of intracranial pathology which revealed the SAH. MR angiogram was negative for vascular causes.
It is important to note that these symptoms may be mistaken for pre-eclampsia/eclampsia. The suggested hypothesis for hypertension induced SAH in pregnancy is failure of cerebral auto regulation with propagation of the high arterial pressure waves to the relatively thin walled pial veins, resulting in their rupture [4,6]. Our Patient was normotensive and routine Urine examination showed no proteinuria throughout pregnancy so this diagnosis was ruled out. The other differential diagnosis was postpartum cerebral angiopathy (PPCA). PPCA may present as intracerebral bleed in normotensive women [7]. PPCA was ruled out as MR angiogram showed normal caliber of brain vessel. Migraine headache classically cause severe headache, nausea and vomiting. Migraine is well established risk factor for ischaemic stroke but migrainous haemorrhage stroke is uncommon [8]. Our patient had no previous personal and family history of migraine.
Only few cases of intracranial haemorrhage after dural puncture have been described and most of these are subdural hematomas. Intracerebral haemorrhage and SAH are reported in very few cases [9]. Eggert SM and Eggers KA, described a 29-year-old woman who had SAH in post-partum period after administration of spinal anaesthesia for removal of retained placenta [9]. They postulated that potentially continuing CSF leak leads to low CSF pressure. The decrease in intracranial pressure could cause an increase in transmural pressure across the arterial wall, thus facilitating the rupture of potential vascular malformations [10].
In absence of other factors, there is a possibility that intracranial haemorrhage occurred when the spinal block was performed. On the other hand, concurrence of spinal anaesthesia and SAH might have been purely incidental as 5-10% of spontaneous SAH occurence is idiopathic [10]. The literature reports that the outcome is usually better in patient who are young and in whom no cause is found. The good clinical recovery seen in our patient is consistent with these observations.
There is no difference in maternal and foetal outcome whether vaginal or a caesarean section is performed in patient with untreated aneurysms and Arterio Vascular Malformations [10]. We should avoid spinal anaesthesia in this patient if she requires anaesthesia in future. General anaesthesia may be preferred.
Conclusion
Post spinal headache should always be evaluated properly taking into consideration the various differential diagnosis of postoperative headache. Dreadful complication like SAH should be timely diagnosed and treated for better outcome.
[1]. Mooij JJA, Grading and Decision-Making in (Aneurysmal) Subarachnoid HaemorrhageInterv Neuroradiol 2001 7(4):283-89.10.1177/15910199010070040220663360 [Google Scholar] [CrossRef] [PubMed]
[2]. Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, Guidelines for the management of aneurysmal subarachnoid haemorrhage: a statement for healthcare professional from a special writing group of the Stroke Council, American Heart AssociationStroke 2009 40(3):994-1025.10.1161/STROKEAHA.108.19139519164800 [Google Scholar] [CrossRef] [PubMed]
[3]. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Guidelines for the management of aneurysmal subarachnoid haemorrhage : a guideline for healthcare professional from the American Heart Association/American Stroke AssociationStroke 2012 43(6):1711-37.10.1161/STR.0b013e318258783922556195 [Google Scholar] [CrossRef] [PubMed]
[4]. Zak IT, Dulai HS, Kish KK, Imaging of neurologic disorders associated with pregnancy and the postpartum periodRadiographics 2007 27(1):95-108.10.1148/rg.27106504617235001 [Google Scholar] [CrossRef] [PubMed]
[5]. Bateman BT, Olbrecht VA, Berman MF, Minehart RD, Schwamm LH, Leffert LR, Peripartum Subarachnoid HaemorrhageAnaesthesiology 2012 116(2):324-33.10.1097/ALN.0b013e3182410b2222166951 [Google Scholar] [CrossRef] [PubMed]
[6]. Shah AK, Non-aneurysmal primary subarachnoid haemorrhage in pregnancy- induced hypertension and eclampsiaNeurology 2003 61(1):117-20.10.1212/01.WNL.0000069609.36517.A312847171 [Google Scholar] [CrossRef] [PubMed]
[7]. Sohoni CA, Subarachnoid haemorrhage caused by pregnancy induced hypertension: A rare occurrenceJ Sci Soc 2013 40(3):174-76.10.4103/0974-5009.12006120736268 [Google Scholar] [CrossRef] [PubMed]
[8]. Tobias K, Carlos KS, Markus S, Christophe T, Julie BE, Migraine and risk of haemorrhage stroke in women prospective cohort studyBMJ 2010 341:c3659 [Google Scholar]
[9]. Eggert SM, Eggers KA, Subarachnoid haemorrhage following spinal anaesthesia in an obstetric patientBritish J of Anaesthesia 2001 86(3):442-44.10.1093/bja/86.3.44211573540 [Google Scholar] [CrossRef] [PubMed]
[10]. Gonullua H, Karadasa S, Oncub MR, Tasdemirc M, Two patients with subarachnoid haemorrhage in pregnancyEastern J of Medicine 2013 18:76-80. [Google Scholar]