Inferior Epigastric Artery (IEA) is an important landmark in laparoscopic inguinal hernia surgery. Injury to this artery is although very rare, but it is vulnerable to injury if due care is not taken while doing Laparoscopic Inguinal Hernia (LIH) surgery. We report a case of accidental inferior epigastric artery injury in a LIH. It was a partial injury to the wall of artery, we were able to manage it by monopolar electrocautery on maryland forceps. This case report will discuss the anatomy of inferior epigastric artery, its mechanism of injury and management.
Intra-operative, Trans Abdominal Pre Peritoneal (TAPP), Total Extra Peritoneal (TEP), Vascular injury
Case Report
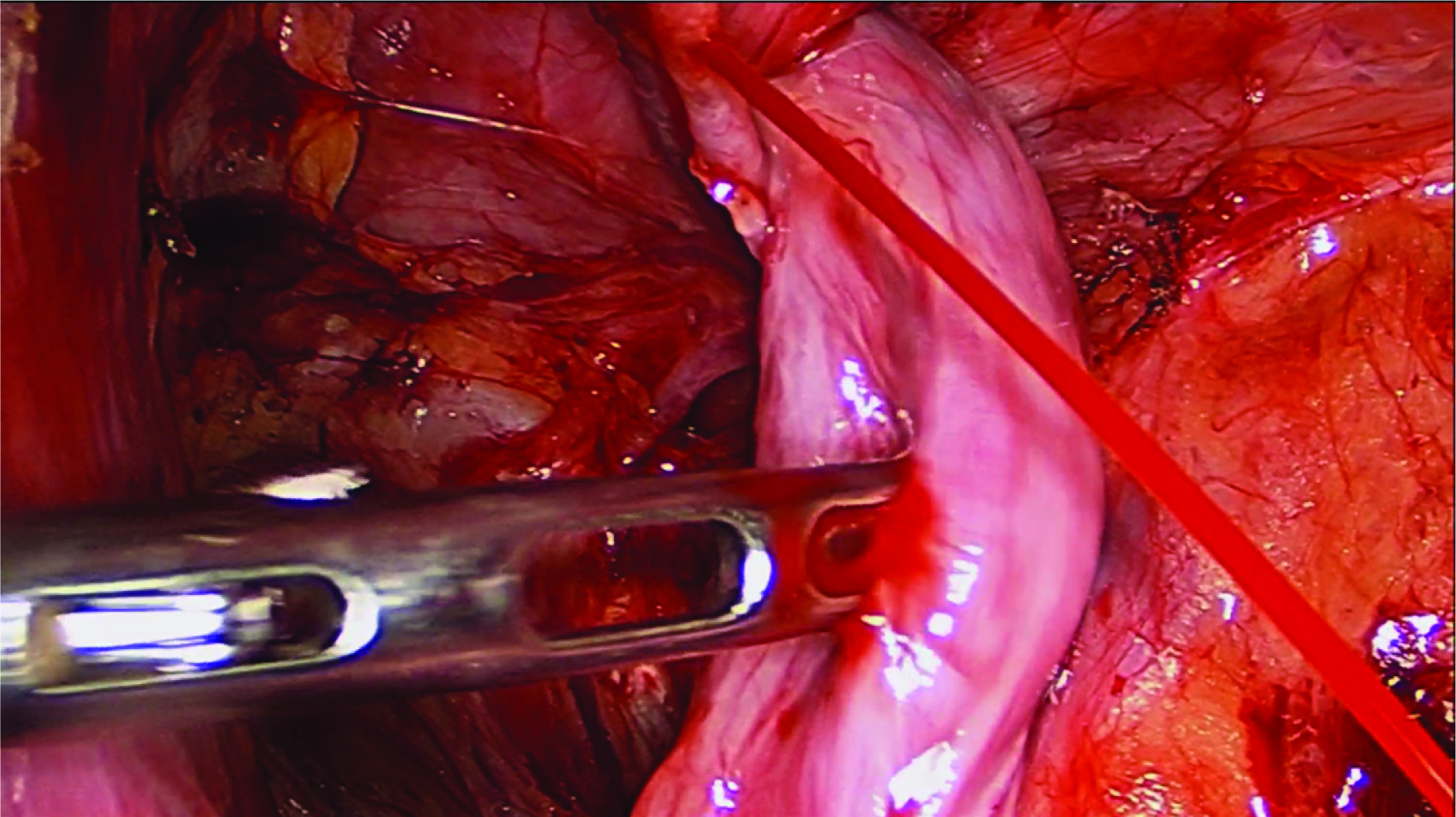
A 50-year old man who was admitted for Trans Abdominal Pre Peritoneal (TAPP) hernia repair for unilateral reducible complete inguinal hernia under general anaesthesia. A partial injury to the wall of IEA occurred while separating hernia sac from cord structure. Bleeding site was approximately 1-2 cm away from deep ring [Table/Fig-1]. This bleeding was controlled by using monopolar cautery on laparoscopic maryland forceps and procedure was completed. Postoperative period was uneventful and patient was discharged on second postoperative day without any complication. Stitches were removed on seventh postoperative day. Patient had a follow up of 3 month duration without any morbidity.
IEA injury in laparoscopic inguinal hernia.
Discussion
Vascular injury during LIH surgery is very rare, incidence of IEA injury in laparoscopic inguinal hernia repair ranges from 0.1 to 0.4% [1]. IEA is an important landmark in inguinal hernia surgery [1], it differentiates between direct and indirect hernia and is a guide for hernia dissection [1]. IEA is most commonly injured vessel of anterior abdominal wall during surgery [1]. Bleeding from IEA may occur during laparoscopic as well as open inguinal hernia repair [2]. Because of large area of dissection in LIH surgery chances of injury are more [2], with greater risk in recurrent LIH surgery [2]. Understanding the IEA injury is very important for prevention of complication of LIH surgery [2]. Various case reports of IEA injury and bleeding in various other situation exists in literature [3-5] but to the best of our knowledge, this is first case report of IEA injury in LIH surgery.
IEA arises from the external iliac artery and anastomoses with the superior epigastric artery [5]. Along its course, it is accompanied by two inferior epigastric veins. It arises from the external iliac, immediately above the inguinal ligament. It curves forward in the sub peritoneal tissue and then ascends obliquely along the medial margin of the deep inguinal ring. Continuing its course upward, it pierces the transversal fascia, and passes in front of the linea semicircularis (arcuate line), ascends between the rectus abdominals and the posterior lamella of its sheath. It finally divides into numerous branches, which anastomose, above the umbilicus, with the branches of superior epigastric branch of the internal mammary (internal thoracic artery) and with the lower intercostal arteries [5].
Vas deferens in the male, as it leaves the spermatic cord and the round ligament of the uterus in the female, winds around the lateral and posterior aspects of the artery [5].
The variations of the course of the IEA have been well documented in the literature. Jakubowicz and Czarniawska-Grzesinska did cadaveric dissection of 76 lower limbs; they found that in 76% of cases, the IEA arose from external iliac artery and above the inguinal ligament, 12% arose behind the ligament, 8% arose from the femoral artery below the inguinal ligament and in 4% the IEA shared a common trunk with an abnormal obturator artery [6].
IEA is an important artery of anterior abdominal wall; it is an important subject of study by scientists. Importance of IEA lies in plastic surgery, minimal access surgery, intervention radiology, gynaecologic surgery, general surgery [7], cardiothoracic surgery, orthopaedics and trauma [4]. Surgeries where IEA got injured are caesarean section, vascular intervention, cardiac catheterization, while putting accessory port in minimal access surgery and flap surgery.
For discussion purpose IEA injury can be grouped as bleeding disorder or coagulation disorder, surgery, vascular intervention and trauma related.
Paul R reviewed IEA injury on intervention radiology and he found that aetiology was Paracentesis (40%), surgical trauma (5%), percutaneous drain placement (15%), blunt trauma (10%), subcutaneous injection (5%), stabbing (5%) and unknown (10%). Majority (79%) had underlying coagulopathy [8]. The diagnosis was confirmed by contrast medium-enhanced CT (70%), tagged red blood cell scan (10%) and non-contrast CT (5%) [9].
In minimal access surgery, IEA is prone to injury while putting ancillary ports especially in pelvic surgery [10]. To prevent IEA injury, trans- illumination method is suggested but this is not effective in obese patient [10,11]. Praisy Joy from his study of IEA anatomy in cadaver, suggested the safety zone on anterior abdominal wall and advised that to avoid injury to the IEA, ancillary trocars can be safely inserted at 5.5 cm away from the midline (or) more than one-third of the distance between the midline and a sagittal plane through anterior superior iliac spine [12]. Various methods for control of bleeding from IEA while putting ancillary port has been reported, like suturing with straight needle, trans-facial suture, clipping and use of Foley’s catheter [13]. Sometimes, this port side bleeding may be serious cause of postoperative bleeding and shock [14,15].
Various report of IEA injury leading to false aneurysm formation had been reported following injury to vessel wall either as a complication of intervention procedure of abdominal wall or following surgical trauma. These aneurysm when rupture, lead to rectus sheath hematoma, intra-abdominal bleeding and shock [15].
Injury to IEA in LIH surgery can occur at following steps [15], while creating space especially in TEP, while doing hernia sac separation from cord structure and tacking of mesh. Injury to IEA is prevented in these two places by remaining in proper plane while creating space, that mean IEA should remain on roof, it should not hang. While doing hernia sac separation from cord structure, sac separation should be done in middle part or in lower part of sac, not near to the deep ring, so that operating surgeon will be away from IEA, as in our case when we reviewed our own video we found that injury to IEA occurred because we were doing dissection near to deep ring. Injury might have been prevented by remaining away from deep ring. To prevent injury by tacker one should not tack the mesh in IEA territory.
In a TAPP procedure, while raising peritoneal flap, injury to IEA may occur if peritoneum is cut beyond the medial umbilical ligament. Procedure of LIH surgery had been well standardised by various authors [16]. Wijerathne S et al., in his review stressed that exact procedure should be followed so that procedure will not fall in disrepute [16]. Postoperative bleeding from IEA can be diagnosed by contrast CT scan and coil embolization is an effective method for control of haemorrhage.
International Endo hernia society has described LIH surgery as advanced surgical procedure and advised surgeon to go for proper simulator training [16]. The learning curve of LIH surgery is steep, they advised minimum 100-150 procedure to become master in procedure and to reduce complication [16]. Krishna A et al., also stressed the need to get peered by senior surgeon to reduce the complication by junior surgeon [17].
Wong C et al., in his review suggested various methods for intraoperative bleeding control that include bipolar coagulation, tamponade, suturing, open surgery, embolisation and ultrasound-guided thrombin injection or compression [18]. We used monopolar cautery on maryland forceps, which worked well and bleeding stopped.
Conclusion
LIH surgery has got steep learning curve, complications are common in early phase of learning curve. Proper knowledge of anatomy is must to prevent IEA injury in LIH surgery.
Abbreviations
Inferior Epigastric Artery (IEA), Laparoscopic inguinal Hernia (LIH), TEP (Total Extra Peritoneal), TAPP (Trans-Abdominal Pre Peritoneal).
[1]. Spaw AT, Ennis BW, Spaw LP, Laparoscopic hernia repair: the anatomic basisJournal of Laparoendoscopic Surgery 1991 1(5):269-77.10.1089/lps.1991.1.2691834279 [Google Scholar] [CrossRef] [PubMed]
[2]. Bendavid R, Complications of groin hernia surgerySurgical Clinics 1998 78(6):1089-103.10.1016/S0039-6109(05)70371-6 [Google Scholar] [CrossRef]
[3]. Sobkin PR, Bloom AI, Wilson MW, LaBerge JM, Hastings GS, Gordon RL, Massive abdominal wall hemorrhage from injury to the inferior epigastric artery: a retrospective reviewJournal of Vascular and Interventional Radiology 2008 19(3):327-32.10.1016/j.jvir.2007.11.00418295690 [Google Scholar] [CrossRef] [PubMed]
[4]. Meyers TJ, Smith WR, Ferrari JD, Morgan SJ, Franciose RJ, Echeverri JA, Avulsion of the pubic branch of the inferior epigastric artery: a cause of hemodynamic instability in minimally displaced fractures of the pubic ramiJournal of Trauma and Acute Care Surgery 2000 49(4):750-53.0.1097/00005373-200010000-0002611038096 [Google Scholar] [CrossRef] [PubMed]
[5]. Epstein J, Arora A, Ellis H, Surface anatomy of the inferior epigastric artery in relation to laparoscopic injuryClinical anatomy 2004 17(5):400-08.10.1002/ca.1019215176037 [Google Scholar] [CrossRef] [PubMed]
[6]. Jakubowicz M, Czarniawska-Grzesiñska M, Variability in origin and topography of the inferior epigastric and obturator arteriesFolia Morphologica 1996 55(2):121-26. [Google Scholar]
[7]. Taylor GI, Corlett R, Boyd JB, The extended deep inferior epigastric flap: a clinical techniquePlastic and Reconstructive Surgery 1983 72(6):751-65.10.1097/00006534-198312000-000016647599 [Google Scholar] [CrossRef] [PubMed]
[8]. Munro MG, Laparoscopic access: complications, technologies, and techniquesCurrent Opinion in Obstetrics and Gynecology 2002 14(4):365-74.10.1097/00001703-200208000-0000212151825 [Google Scholar] [CrossRef] [PubMed]
[9]. Lavery S, Porter S, Trew G, Margara R, Jackson J, Use of inferior epigastric artery embolization to arrest bleeding at operative laparoscopyFertility and sterility 2006 86(3):719-e13.10.1016/j.fertnstert.2006.01.05416893543 [Google Scholar] [CrossRef] [PubMed]
[10]. Hurd WW, Amesse LS, Gruber JS, Horowitz GM, Cha GM, Hurteau JA, Visualization of the epigastric vessels and bladder before laparoscopic trocar placementFertility and sterility 2003 80(1):20910.1016/S0015-0282(03)00555-7 [Google Scholar] [CrossRef]
[11]. Joy P, Simon B, Prithishkumar IJ, Isaac B, Topography of inferior epigastric artery relevant to laparoscopy: a CT angiographic studySurgical and Radiologic Anatomy 2016 38(3):279-83.10.1007/s00276-015-1513-926188502 [Google Scholar] [CrossRef] [PubMed]
[12]. Saber AA, Meslemani AM, Davis R, Pimentel R, Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vesselsAnnals of surgery 2004 239(2):18210.1097/01.sla.0000109151.53296.0714745325 [Google Scholar] [CrossRef] [PubMed]
[13]. Mitidieri M, Picardo E, Petruzzelli P, Ruffino MA, Garbagni G, Todros T, Pseudoaneurysm of the inferior epigastric artery after gynecological laparoscopy: minimally invasive managementEuropean Journal of Obstetrics and Gynecology and Reproductive Biology 2014 173:119-20.10.1016/j.ejogrb.2013.11.00224287287 [Google Scholar] [CrossRef] [PubMed]
[14]. Shokoohi H, Boniface K, Taheri MR, Pourmand A, Spontaneous rectus sheath hematoma diagnosed by point-of-care ultrasonographyCanadian Journal of Emergency Medicine 2013 15(2):120-23.10.2310/8000.2012.120721 [Google Scholar] [CrossRef]
[15]. Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]Surgical endoscopy 2011 25(9):277310.1007/s00464-011-1799-621751060 [Google Scholar] [CrossRef] [PubMed]
[16]. Wijerathne S, Agarwal N, Ramzy A, Lomanto D, A prospective randomized controlled trial to compare single-port endo-laparoscopic surgery versus conventional TEP inguinal hernia repairSurgical Endoscopy 2014 28(11):3053-58.10.1007/s00464-014-3578-724902814 [Google Scholar] [CrossRef] [PubMed]
[17]. Krishna A, Misra MC, Bansal VK, Kumar S, Rajeshwari S, Chabra A, Laparoscopic inguinal hernia repair: transabdominalpreperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trialSurgical Endoscopy 2012 26(3):639-49.10.1007/s00464-011-1931-721959688 [Google Scholar] [CrossRef] [PubMed]
[18]. Wong C, Merkur H, Inferior epigastric artery: surface anatomy, prevention and management of injuryAustralian and New Zealand Journal of Obstetrics and Gynaecology 2016 56(2):137-41.10.1111/ajo.1242626627186 [Google Scholar] [CrossRef] [PubMed]