The objective of the study was to fabricate definitive prosthesis by modifying the splints used for fracture reduction, so as to simplify the treatment of edentulous patient. Traumatic fractures are known to present with clinically debilitating repercussions, and when occurring in edentulous jaws, achieving effective management becomes an even more herculean task for the clinician. Thus, deciding the most appropriate line of management, whether surgical or conservative, becomes crucial, which is guided by a plethora of factors, namely patient factors, nature of mandibular fracture (displaced or undisplaced, favourable or unfavourable), type of armamentarium available and the surgeon’s skills. Closed reduction of undisplaced fractures of edentulous mandible using Gunning splint, though an old concept, still reckons a trust worthy treatment aid in treating such types of fractures. This study illustrates a case report of edentulous mandibular fracture in which a gunning splint with posterior teeth as occlusal stops were used for achieving adequate immobilisation and fixation of parasymphyseal fracture segments, and it was subsequently modified to complete denture prosthesis as a simplified rehabilitation measure.
Dexterous approach, Geriatric lower jaw fractures, Maximally conservative, Minimally invasive
Introduction
A 50-year-old male patient was referred to Department of Prosthodontics from Oral and Maxillofacial Surgery for contemplating and deciding the most suitable treatment option following a mandibular fracture. Patient elicited history of sustained trauma in lower front region of the face due to road traffic accident, which had occurred seven days before reporting to the department. Patient was hypertensive since 5-6 years and was on medication for the same.
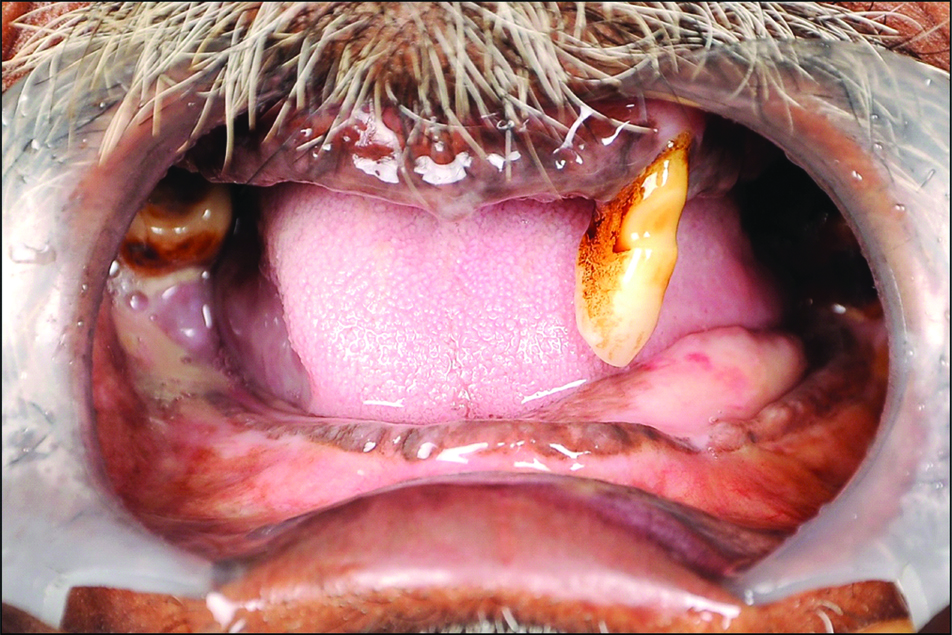
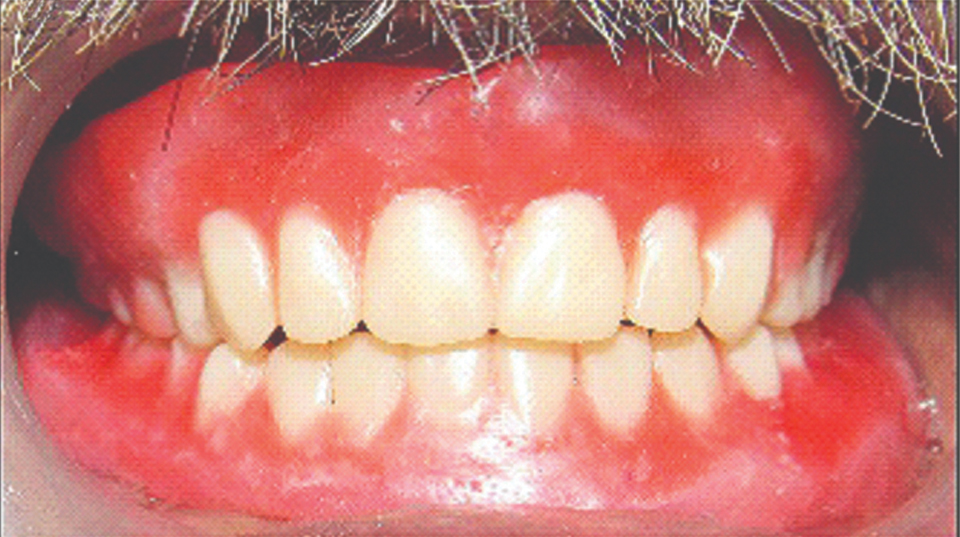
No extra oral bruise, laceration or bleeding was present. Intraoral examination revealed the mandibular ridge to be atrophic and partially edentulous maxillary and mandibular arches, with maxillary left canine (#23) being supra erupted and mandibular arch’s isolated teeth mandibular left third molar (#38) and mandibular right third molar (#48) presented with Grade II mobility [Table/Fig-1].
Preoperative intraoral view.
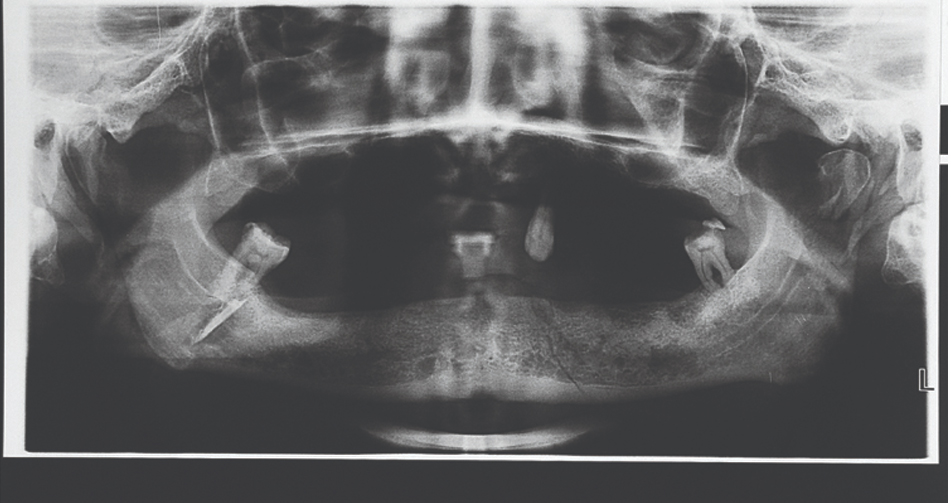
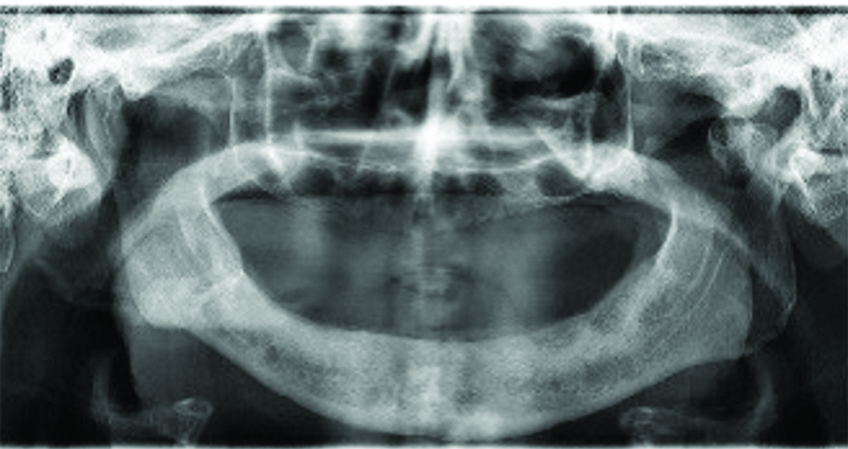
Orthopantograhic examination showed a single fracture line present along the course of left para symphyseal region, running downwards and backwards unto the lower border of mandible superio-inferiorly [Table/Fig-2].
Panoramic radiograph showing fracture line.
Past dental history revealed that patient had not been wearing any removable prosthesis. After having contemplated the surgical treatment options, giving due respect to all the clinical and radiographic findings, and paying heed to patient’s insistence for a conservative treatment modality a conclusive decision for non invasive closed reduction of fractured para symphyseal segment was undertaken, by fabricating gunning splint. Informed consent for the same was obtained from the patient. As teeth #23, #38 and #48 were adjudged with poor clinical prognosis, and speculated as hindrances with the prosthetic clinical steps; they were extracted beforehand and allowed to heal undisturbed for two weeks before proceeding with the impression making.
Clinical Procedure
Preliminary impressions of maxillary and mandibular arch were made with irreversible hydrocolloid impression material (Imprint DPI Mumbai). Impressions were poured immediately in Dental plaster (Type 2 model Plaster, Kalabhai Karson Pvt., Ltd., Mumbai, India) to obtain diagnostic casts. As there was no evident notable mobility between the fractured segments of edentulous mandible, the casts were not altered.
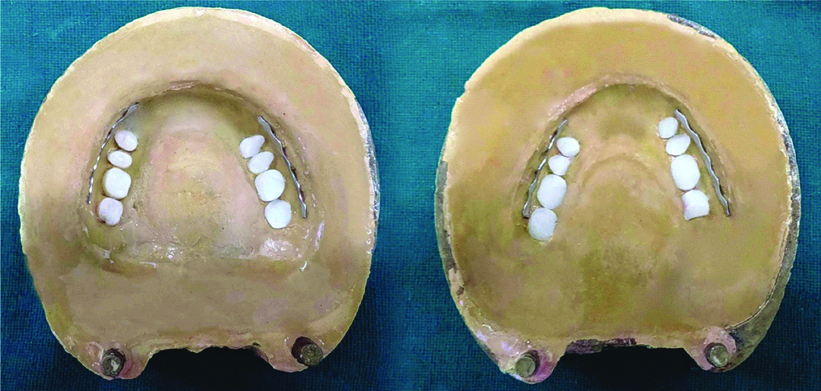
Border molding was done on special trays made up of auto-polymerising acrylic resin (Acralyn R Pink Mumbai) with low fusing green stick compound (DPI Pinnacle tracing stick, Mumbai) and final impressions were made with Light Body Elastomeric impression material (Zhermack, OranWash Inc.) [Table/Fig-3]. Master casts were poured using dental Stone (Goldstone Stone Plaster type 3). No alteration of cast was required as it was an undisplaced fracture. Temporary record bases were fabricated using auto-polymerising acrylic resin and occlusal rims were made on the master casts obtained. A tentative jaw relation was recorded with adequate freeway space, and the maxillary mandibular jaw relation was carefully sealed.
Final Impressions made of the edentulous arches.

Teeth arrangement was performed, and try-in was approved. After try-in, maxillary and mandibular canine to canine teeth of both arches were removed to create space and enabling patient’s feeding, and Erich’s arch bars were incorporated in wax trial itself, from premolar to second molar flanges bilaterally [Table/Fig-4]. Precisely, this very manoeuvre allowed the waxed up denture trials to serve as modified gunning splints, because these arch bars were utilised for achieving inter maxillary fixation. Thereafter, the maxillary and mandibular splints were invested separately in varsity type flasks using three pour technique. Dewaxing was done. Splints were processed with acrylisation using heat cured acrylic resin (Acralyn H Pink Mumbai) by conventional compression moulding technique. Splints were retrieved, finished and polished and finally seated in patient’s mouth. Prosthesis were checked for correctly achieved extension, retention, stability and disinfected in glutaraldehyde solution.
Erich’s arch bars incorporated into flask molds prior to packing of acrylic dough.
During surgical procedure, first the maxillary splint was fixed using per-alveolar and circum-zygomatic wirings, while the mandibular splint was secured to the underlying bone by circum-mandibular wiring [Table/Fig-5]. Next, intermaxillary fixation was carried out with arch wires to provide firm immobilisation [Table/Fig-6]. Patient was strictly instructed for liquid diet consumption so as to ensure his general health maintenance. He was specifically harped upon for oral hygiene maintenance post diet, while on follow-up visits to the hospital, flushing and debridement with povidone iodine and normal saline were carried out. Periodic follow-up visits were scheduled at intervals of 48 hours, one week, and four weeks. Oral hygiene was optimally maintained by the patient during this time frame.
Surgically performed circum zygomatic and circum-mandibular wiring.

Inter maxillary fixation.
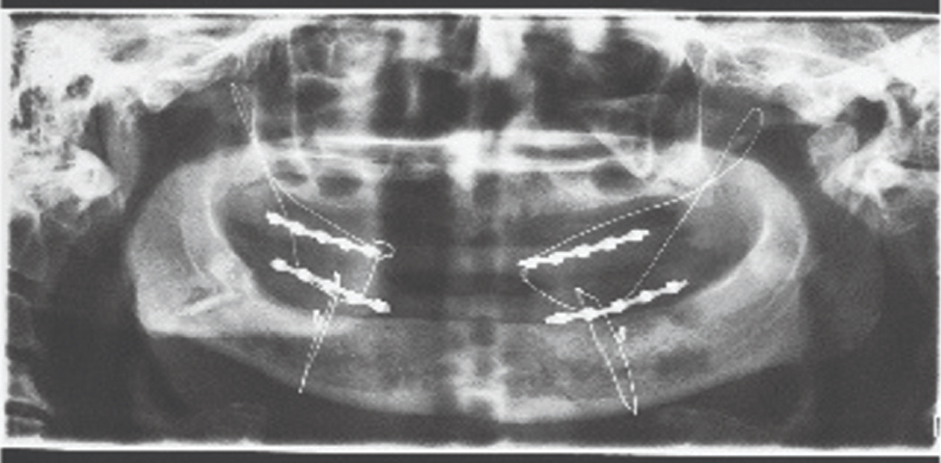
These arch bars with wirings were held in place for six weeks. After verification of healing on orthopantograph arch bars were removed [Table/Fig-7]; the excess acrylic was also trimmed in areas where teeth were previously removed (maxillary and mandibular canine to canine teeth), thereby allowing these splints to be converted into definitive complete denture prosthesis. Retention and stability of dentures were re-evaluated and were found to be adequate. Next anterior wax rims were made and definitive maxillary mandibular relation was recorded and verified. Midline was marked in patient’s mouth and was transferred and mounted onto semi adjustable articulator. Remaining anterior teeth in both dentures were arranged and anterior try-in was verified [Table/Fig-8]. Wax-up was done in labial areas all over the dentures and was again invested and dewaxing was done. Same heat cure material was again used for packing of dentures using compression moulding technique. Final dentures were retrieved and finished, polished and delivered to the patient with post insertion care and maintenance instructions. Patient was recalled for follow-up after 24 hours, three days, one week, one month, six months and 12 months, without any notable complaint or discomfort. Orthopantograh evaluated on one year follow-up depicted adequate osseous healing [Table/Fig-9].
Arch bars removed after OPG verification post six weeks of reduction and fixation.

Panoramic radiograph taken on one year follow-up visit.
Discussion
Position and prominence of the mandible poses it as the second most commonly fractured part of the maxillofacial skeleton [1]. According to Kazanjian VH and Converse JM, classification of edentulous fracture falls under Class III type [2]. The absence of teeth, thin bone, deficient blood supply and compromised medical condition of the patient makes treatment of these fractures particularly difficult. Non union and infection are the most feared complications when treating these fractures [3].
The edentulous fractured mandible can be harmoniously healed by adhering to the principles of general fracture management, so as to maintain the form and function and by reducing and fixing the fractured segments. Of the various treatment options available in the present study, closed reduction was chosen by maxillofacial surgeon that comes along with its own pros and cons. For the closed reduction of mandibular fractures, gunning splint holds a ground of solidarity and reliability till date. Gunning-type splints are relatively quick and easy to apply as a fixation devices for achieving closed reduction. Traditionally, the two-piece gunning splints were constructed with posterior bite blocks, serving as occlusal stops, and anteriorly a space was provided for feeding [4]. In the present study, an attempt has been made to modify these splints, and utilise them as complete denture prosthesis later on after having achieved adequate immobilisation and fixation of the para symphyseal fracture segments. The rationale behind this modification is to establish the mandibular to maxillary relationship with use of teeth in occlusion, so as to aid in adequate reduction of the fracture. Mere addition of the anterior teeth segments in these modified splints later on, ultimately reduced the acclimatisation time of the dentures (definitive prosthesis), thereby promoting a better acceptance on part of the patient. Edentulousness in context of severity of displacement of fractures happens to be a blessing in disguise, as larger percentage of such fractures yield up to be of non compound nature. Hence, minor displacement of the bones can be readily accommodated in the construction of gunning splints, subsequently modified to complete denture prosthesis [5].
Bruce RA and Strachan DS suggested the greater likelihood of non union with open reduction in comparison to closed methods, and exhorted attempting the later modality of treatment [6]. Indispensably occurring senile changes hamper the healing and regenerative capacities in older individuals, decreased osteogenesis, significant operative risk, local factors like atrophic, dense cortical bone and inadequate blood supply gravier the prognosis. This further convolutes decision to perform a non life saving surgical procedure under general anaesthesia.
With a wide array of treatment options and upsurging sophisticated technologies available, there is still controversy over the best treatment for each type of mandibular fracture. However, by incorporating innovative means, such as the one described through this study case report (a modified gunning splint), it can arguably prove to be pivotal in treating fracture cases satisfactorily, even by such closed conservative approaches, adhering to minimalism rather than extensively invasive surgical means.
Conclusion
Geriatric fractures of edentulous mandible is invariably encountered in contemporary clinical practice, the efficient management of which requires a meticulous diagnosis, treatment plan and multidisciplinary coordinated oral surgical and prosthodontic intervention. An attempt has been made to present a simplified yet effective treatment plan for such clinical presentations.
[1]. Ogundare BO, Bonnick A, Bayley N, Pattern of mandibular fractures in an urban major trauma centerJ Oral Maxillofac Surg 2003 61(6):713-18.10.1053/joms.2003.5011812796884 [Google Scholar] [CrossRef] [PubMed]
[2]. Kazanjian VH, Converse JM, The Surgical Treatment of Facial Injuries (ed 1) 1949 BaltimoreWilliams & Wilkins Company [Google Scholar]
[3]. Luhr HG, Reidick T, Merten HA, Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive casesJournal of Oral and Maxillofacial Surgery 1996 54(3):250-54.10.1016/S0278-2391(96)90733-8 [Google Scholar] [CrossRef]
[4]. Gunning TB, Treatment of fracture of the lower jaw by interdental splints: I-IIIAm J Dent Sci 1868 2:214-20. [Google Scholar]
[5]. Miloro M, Ghali GE, Larsen PE, Peterson’s Principles of Oral and Maxillofacial Surgery 2004 Hamilton, BCin: Decker Inc:224 [Google Scholar]
[6]. Bruce RA, Strachan DS, Fractures of the edentulous mandible: The Chambers J. Lyons Academy studyJ Oral Surg 1976 34:393 [Google Scholar]