Metastatic Renal Cell Carcinoma in Nasopharynx-A Paradox: Case Report and Review of Literature
Kachnar Varma1, Faheema Hasan2, Vatsala Misra3, PA Singh4
1 Associate Professor, Department of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
2 Final year Postgraduate Resident, Department of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
3 Professor and Head, Department of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
4 Professor, Department of Pathology, Moti Lal Nehru Medical College, Allahabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Faheema Hasan, Final year Postgraduate Resident, Department of Pathology, Moti Lal Nehru Medical College, Allahabad-211002, Uttar Pradesh, India.
E-mail: 1faheemahasan@gmail.com
Metastatic renal cell carcinoma of the head and neck is extremely rare. Metastasis to the nasopharynx is extremely unusual and can be misdiagnosed as primary of the specific site hindering further management. The present case report of an 82-year-old male presenting with epistaxis was found to have a nasopharyngeal mass on radiology. Microscopic evaluation of the nasopharyngeal mass revealed a highly vascular clear cell tumour with cells arranged in alveolar and trabecular pattern. Immunohistochemical assessment revealed positive PAX 8, CD10 and vimentin which are highly specific for metastatic renal cell carcinoma. Retrospective computed tomography scan revealed a renal mass; however, the patient succumbed before any biopsy could be performed.
Clear cell tumour, Epistaxis, Immunohistochemistry
Case Report
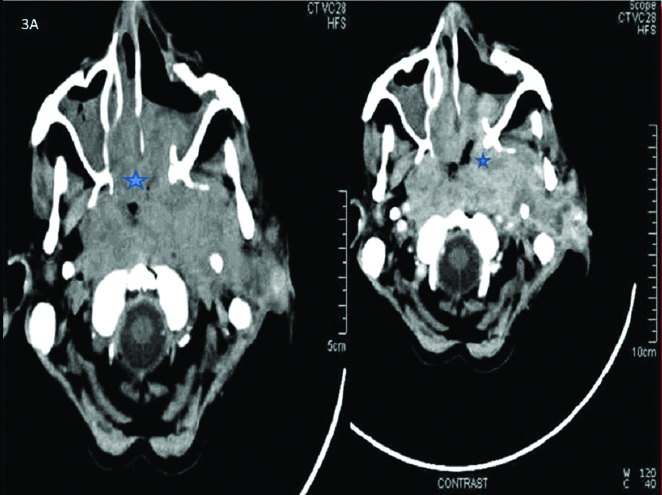
A 82-year-old man presented with recurrent epistaxis for a month. Endoscopy revealed a highly vascular mass in the nasopharynx. CT scan of the head and neck was done which revealed a large extensive infiltrating mass lesion in the nasopharynx extending into the posterior part of both halves of nasal cavity. Lesion was inhomogeneously enhancing on post contrast scan. Erosion of petrous bones and extension into left infra temporal fossa was also noted [Table/Fig-1a].
Pre and post contrast CT showing a vascular enhancing nasopharyngeal mass marked with a star.
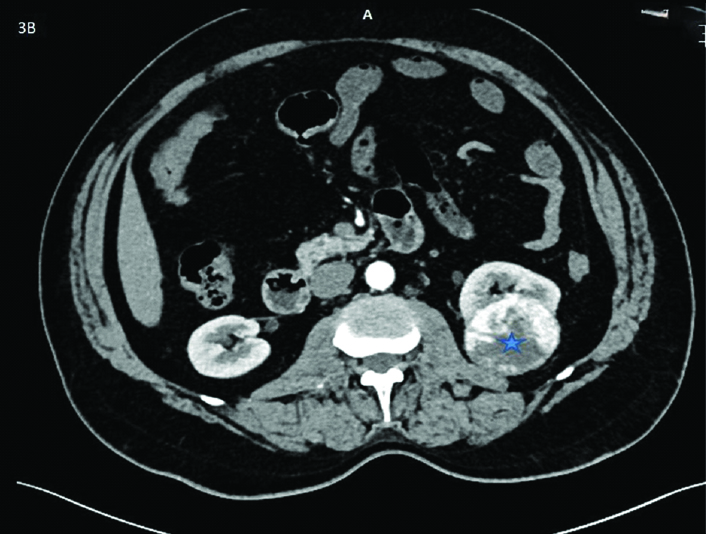
Computed tomography was performed and showed a focal well marginated space occupying lesion of size 55×48 mm at posterior cortex interpolar region of left kidney [Table/Fig-1b]. Hence, a diagnosis of metastatic renal cell carcinoma was made. However, biopsy or nephrectomy could not be performed as the patient succumbed to the disease.
CT scan showing a well marginated lesion in the left kidney marked with a star.
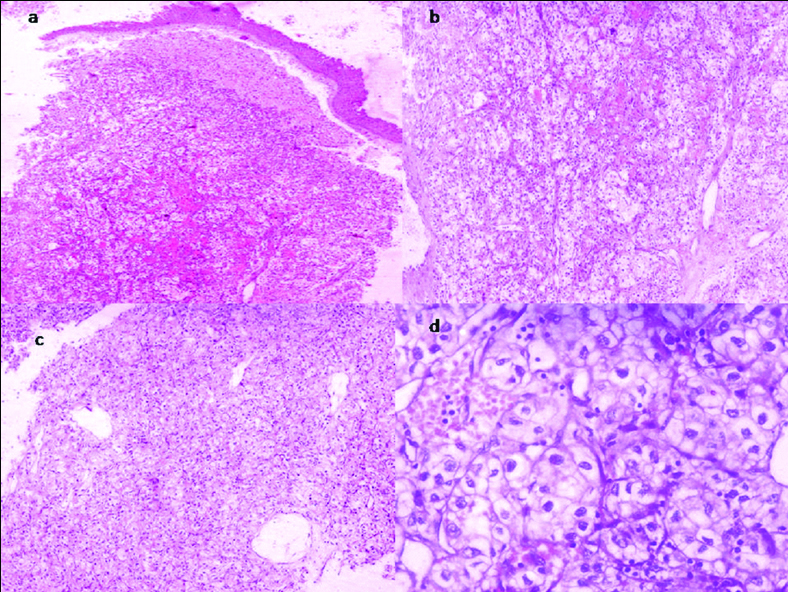
Biopsy of the mass was performed and sent for histopathological examination. It showed a clear cell lesion arranged in alveolar and trabecular pattern with extensive vascularity, just below the repiratory epithelium [Table/Fig-2a-c]. These cells were large and had high nuclear: cytoplasmic ratio, hyperchromatic nuclei with inconspicuous nucleoli [Table/Fig-2d]. A review of clinical symptoms was demanded from the clinician and no abdominal or urinary symptoms were observed. A thorough clinical examination was also performed and no abdominal mass was found.
H&E showing: a) diffuse infiltrative tumour cells arranged in nests just below the pseudostratified ciliated columnar lining of the nasopharynx at 4X; b) and c) Tumour cell population consisting of clear cells with prominent vascular proliferation at 10X; and d) individual tumour cells arranged in alveolar pattern with hyperchromatic nuclei, inconspicuous nucleoli and abundant clear cytoplasm at 40X.
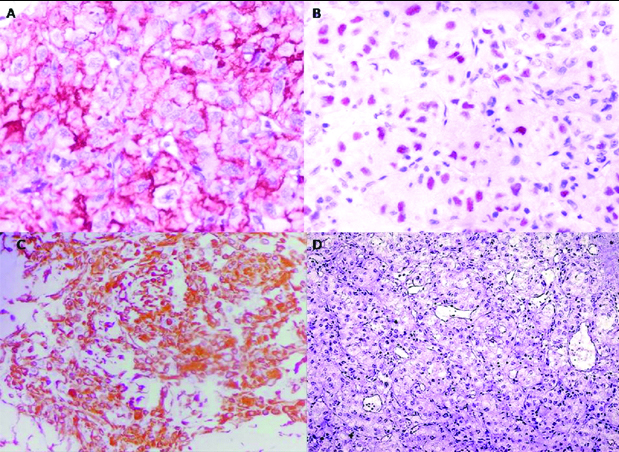
Even though many lesions can have clear cells in the nasopharynx [Table/Fig-3], the characteristic alveolar arrangement and high vascularity, made us suspect metastatic renal cell carcinoma too, despite it being a remote possibility. A panel of immunohistochemical markers consisting of Melan A, HMB5, synaptophysin, chromogrannin, CK 5/6, p63, CD45, CD10, PAX 8 and vimentin was done. Immunohistochemistry turned out positive for CD10, PAX 8, Vimentin [Table/Fig-4a-c]. This made us hint the surgeon on the possibility of metastatic renal cell carcinoma.
Showing comparative IHC panel of clear cell tumors of nasopharynx.
| IHC | CK 5/6 | HMB 45 | CD 10 | PAX 8 | SYNAPTOPHYSIN | VIMENTIN | P63 |
|---|
| Metastatic renal cell carcinoma [12] | -ve | -ve | +ve | +ve | -ve | +ve | -ve |
| Nasopharyngeal squamous cell carcinoma [13] | +ve | -ve | -ve | -ve | -ve | -ve | +ve |
| Melanoma | -ve | +ve | -ve | -ve | +ve | -ve | -ve |
| Paraganglioma [14] | -ve | -ve | -ve | -ve | +ve | -ve | -ve |
| Hyalinising clear cell carcinoma [15] | +ve | -ve | -ve | -ve | -ve | -ve | +ve |
| Present case | -ve | -ve | +ve | +ve | -ve | +ve | -ve |
Immunohistochemistry showing: a) membrane positivity of CD10 (40X); b) nuclear positive staining of PAX 8 (40X); c) Positive staining of vimentin (40X); (d) negative staining of LCA (10X).
Discussion
Renal cell carcinoma is a highly aggressive, vascular and lethal malignancy of elderly patients in age group of 65-74 years with propensity to metastasise. It accounts for 90% of renal malignancies in adults and approximately 3% of adult malignancies [1]. Clear cell renal cell carcinoma accounts for 70-80% of renal cell carcinoma [2]. It is more common in men than women (SEER stat fact sheets). The well known triad of renal carcinoma i.e., haematuria, flank pain and renal mass is seen in only 10% of patients with the disease [3].
More than one-third of the patients with renal carcinoma presents with distant metastases as the initial presentation. The common sites of metastasis of renal cell carcinoma are lungs (75%), regional lymph nodes (65%), bone (40%), liver (40%) and brain (5%) [4,5]. The metastatic pattern of renal cell carcinoma is unpredictable with many unusual sites. While metastasis to head and neck per se is very rare, with thyroid and brain being the preferred sites; the nasopharyngeal metastases are much rarer. It is an extremely unusual site with less than 50 cases reported till date [6].
The clinical impression of vascular space occupying lesion in nasopharynx raises the possibilities of primary lesions like angiofibroma, glomus tumours, haemangioma or haemangiopericytoma [7]. In an elderly patient, distant metastasis should be given a considerable thought. Metastasis to nasopharynx are extremely rare and includes melanoma, renal, lung and breast cancers [8].
The tumour cells of the clear cell renal cell carcinoma can metastasise to the nasopharynx via two possible routes. One, the caval route, where the tumour cells ascends via the inferior vena cava to the right heart and then to the lungs coming via the pulmonary vein and then entering the aorta and then via the maxillary artery reach the nasopharynx. In the second retrograde route, the tumour cells enter the Batson’s plexus and enter the cranium via the internal jugular vein and reach the nasopharynx by unusual flow patterns [9].
Even though patients with metastatic renal cell carcinomas have bad prognosis, the further patient outcome depends on the histological grade and clinical status of the patient [10]. However, the National Comprehensive Cancer Network practice guidelines for kidney cancer states that patients with a resectable tumour and a single metastasis would benefit from nephrectomy and metastasectomy. Also, radiotherapy has been proven to be a useful adjunctive therapy for symptomatic control in patients with metastatic renal cell carcinoma of the nose and paranasal sinuses, offers good symptomatic control even if the primary tumour is not resectable [11].
Histopathological examination of the lesion showed an encapsulated tumour mass lying beneath the lining respiratory epithelium composed of clear cells arranged in an alveolar pattern with extensive vascular proliferation. Based on histology, a differential diagnosis of melanoma, lymphoma, paraganglioma, nasopharyngeal carcinoma and hyalinising clear cell carcinoma were considered. A detailed immunohistochemical workup was performed and immunopositive markers have been shown in [Table/Fig-4]. PAX 8 was considered to be more sensitive than PAX 2 even in metastatic renal cell carcinomas [16], and RCC antigen has been reported to be positive in a number of non renal tumours [17]. Therefore the immunohistochemical workup with CD10, PAX 8, HMB45, Leucocyte Common Antigen (LCA) (CD45), Vimentin, P63 and CK 5/6 was performed. Positivity for CD10, PAX 8 and Vimentin and negativity for LCA confirmed the diagnosis of metastatic renal cell carcinoma of nasopharynx [Table/Fig-4a-d].
Conclusion
In conclusion, nasopharyngeal metastasis of an asymptomatic renal cell carcinoma is very rare. It should be suspected and investigated in patients presenting with highly vascular tumours of the head and neck and more so, if the microscopy shows clear cells. Hence, in every person with a nasopharyngeal mass, a histological diagnosis is a mandatory requirement despite the risk of heavy bleeding. Early suspicion and prompt diagnosis can be beneficial to the patient and even curative surgery or radiotherapy can be offered for a good quality of life. Therefore, this case report highlights the importance of histopathology along with immunohistochemistry in the diagnosis of a nasopharyngeal mass even with apparently innocuous clinical presentation and throws light on the indispensable and vital role of pathologists.
[1]. Siegel RL, Miller KD, Jemal A, Cancer statistics, 2015CA Cancer J Clin 2015 65:05-29.10.3322/caac.2125425559415 [Google Scholar] [CrossRef] [PubMed]
[2]. Brugarolas J, Molecular genetics of clear cell renal cell carcinomaJ Clin Oncol 2014 32(18):1968-76.10.1200/JCO.2012.45.20032482187 [Google Scholar] [CrossRef] [PubMed]
[3]. Skinner DG, Vermillion CD, Pfister RC, Leadbetter WF, Renal cell carcinomaAm Fam Physician 1971 4:89-94. [Google Scholar]
[4]. Ziari M, Shen S, Amato RJ, Teh BS, Metastatic renal cell carcinoma to the nose and ethmoid sinusUrology 2006 67:19910.1016/j.urology.2005.07.05216413368 [Google Scholar] [CrossRef] [PubMed]
[5]. Campbell SC, Lane BR, Malignant renal tumors. In: Wein AJ, Kavoussi LR, Novick AC, editorsCampbell-Walsh Urology 2012 10th edPhiladelphia, PAWB Saunders:1413-1474.10.1016/B978-1-4160-6911-9.00049-922799341 [Google Scholar] [CrossRef] [PubMed]
[6]. Singh J, Baheti V, Yadav SS, Mathur R, Occult renal cell carcinoma manifesting as nasal mass and epistaxisRev Urol 2014 16(3):145-48. [Google Scholar]
[7]. Razek AA, Huang BY, Soft tissue tumors of the head and neck: imaging-based review of the WHO classificationRadiographics 2011 31(7):1923-54.10.1148/rg.31711509522084180 [Google Scholar] [CrossRef] [PubMed]
[8]. Leon B, John WE, Peter R, David S, World Health Organization Classification of Tumours: Pathology and genetics of head and neck tumors 2005 France, LyonInternational Agency for Research on Cancer (IARC):106 [Google Scholar]
[9]. Nahum AM, Bailey BJ, Malignant tumors metastatic to the paranasal sinuses: case report and review of literatureLaryngoscope 1963 73:942-53.10.1288/00005537-196307000-0000914043146 [Google Scholar] [CrossRef] [PubMed]
[10]. Ather MH, Masood N, Siddiqui T, Current management of advanced and metastatic renal cell carcinomaUrol J 2010 7:01-09. [Google Scholar]
[11]. Simo R, Sykes AJ, Hargreaves SP, Axon PR, Birzgalis AR, Slevin NJ, Metastatic renal cell carcinoma to the nose and paranasal sinusesHead Neck 2000 22:722-27.10.1002/1097-0347(200010)22:7<722::AID-HED13>3.0.CO;2-0 [Google Scholar] [CrossRef]
[12]. Truong LD, Shen SS, Immunohistochemical diagnosis of renal neoplasmsArch Pathol Lab Med 2011 135(1):92-109. [Google Scholar]
[13]. Lester DR, Thompson. Update on nasopharyngeal carcinomaHead Neck Pathol 2007 1(1):81-86.10.1007/s12105-007-0012-72061428 [Google Scholar] [CrossRef] [PubMed]
[14]. Johnson TL, Zarbo RJ, Lloyd RV, Crissman JD, Paragangliomas of the head and neck: immunohistochemical neuroendocrine and intermediate filament typingMod Pathol 1988 1(3):216-23. [Google Scholar]
[15]. Baghirath PV, Kumar JV, Vinay BH, Hyalinizing clear cell carcinoma: A rare entityJ Oral Maxillofac Pathol 2011 15(3):335-39.10.4103/0973-029X.8671422144841 [Google Scholar] [CrossRef] [PubMed]
[16]. Ozcan A, de la Roza G, Ro JY, Shen SS, Troung LD, PAX2 and PAX8 expression in primary and metastatic renal tumors. A comprehensive comparisonArch Pathol Lab Med 2012 136:1541-51.10.5858/arpa.2012-0072-OA23194047 [Google Scholar] [CrossRef] [PubMed]
[17]. Bakshi N, Kunju LP, Giordano T, Shah RB, Expression of Renal Cell Carcinoma antigen (RCC) in renal epithelial and nonrenal tumors: Diagnostic implicationsAppl Immunohistochem Mol Morphol 2007 15(3):310-15.10.1097/01.pai.0000213144.70148.8e17721277 [Google Scholar] [CrossRef] [PubMed]