Torsion of adnexal structures; namely the ovaries, tubes or both, account for 2.7-7.4% [1,2] of gynaecological emergencies. The twisting of the mass on its pedicle results in reduced venous return, stromal oedema, internal haemorrhage, and infarction with subsequent sequelae. It most frequently occurs in an unilateral, often pathologically enlarged ovary and is most common among young children [3]. Pregnancy may be associated or be responsible in 20% of torsion cases [4], while benign and malignant ovarian masses account for 50-60% of cases. Torsion is seen in 17% women in premenarchal and postmenopausal age group [5].
Delay or misdiagnosis results in loss of ovarian function and reduced reproductive function in future. However, diagnosis is not straightforward, and there are challenges faced on a regular basis when patients arrive at odd hours in emergency. Torsion can also be confused for a number of gynaecological and surgical emergencies.
The novelty of this study was that this was the first prospective attempt, to analyse this scoring by an independent group of investigators, having no conflict of interest with the original study done by Huchon C et al., in Paris, with an aim to correctly identify ovarian torsion among different cyst accidents, its overall incidence, the types of surgery involved and the histopathological diagnoses of the twisted adnexal masses in a prospective observation over two years [6].
Materials and Methods
This prospective observational study was conducted over the last two years from August 2015 to August 2017 at a Rural Medical College and Hospital in Eastern India. All procedures in this study were done in accordance with the ethical standards as laid down by the Helsinki Declaration in 1975 and amended in 2000. Institutional ethical body clearance was obtained. Women less than 45 years with acute onset lower abdomen/right or left iliac fossa/ suprapubic pain with negative urine pregnancy test were included in present study. Women with chronic pelvic pain, menorrhagia/dysmenorrhoea, pregnancy (intra-uterine/ectopic) or those following ovarian/adnexal surgery were excluded. In this prospective observation, we used a scoring system and clinical points to delineate torsion better from other emergencies, corroborate our predictions with intraoperative findings, as well as discuss unique clinical scenarios intraoperatively that can be important learning points for others. Histopathological diagnoses were also analysed. There were two groups in which the included women were randomly allocated-one in which Huchon’s scoring was used and another where torsion was diagnosed without any formal scoring.
For the purpose of present study, in the scoring group a total score of more than 60 was used to allocate into ‘suspected torsion’ and surgery was done; scores ≤40 were not operated upon. For an intermediate score of 41-60, it was decided that other clinical signs like abdominal tenderness, adnexal and cervical motion tenderness, ultrasound appearance of adnexal mass and clinical judgement was used to allocate into ‘suspected torsion’ or ‘not suspected’ groups accordingly.
The group where scoring was not used, women with acute onset abdominal/pelvic pain, vomiting, leukocytosis, adnexal and cervical motion tenderness with ultrasound appearance suggestive of congested ovarian/adnexal cyst was used to suspect torsion and operate. The clinical scoring system by Huchon C et al., has been described [6]. This preoperative scoring was first developed after a retrospective study of 142 patients with acute pelvic pain in Paris between 2000-04 (derivation cohort). Patients with and without adnexal torsion were compared using Pearson’s Chi-square test for qualitative variables and Student’s t-test for quantitative variables. A total of 15 clinical/biochemical/radiological variables were found to be significantly associated with torsion (p<0.05) and for each of these variables, univariate analyses calculating sensitivity, specificity, positive and negative likelihood ratios were calculated. Multiple logistic regression model was then used in selecting the best model to diagnose torsion. The best model included five variables independently associated with torsion confirmed by surgery, namely unilateral lumbar or abdominal pain, pain duration of less than 8 hours at first presentation, vomiting, absence of leucorrhoea and metrorrhagia, and cyst size more than 5 cm on ultrasound. The stability of this predictive model was also tested using a jackknife method of statistical sampling. The adjusted odds ratios and scoring points of these five variables were as shown in [Table/Fig-1]. The total score was calculated and the predicted risks were 3.7%, 20% and 69% based on total score of 0-40, 45-60 and >60 respectively. The score was validated thereafter in a prospective study of 35 women the year after (validation cohort). A score of ≤40 (low risk) had a specificity of 100% and negative predictive value of zero, while the high risk group (score >60) produced high specificity (97%) and positive likelihood ratios indicating patients with acute pelvic pain and at least having three or four of the five variables had a high probability of torsion.
Scoring system for identification of women with adnexal torsion.
| Serial Number | Criteria | Score Points | Adjusted Odds Ratio (95% CI)+ |
|---|
| 1 | Unilateral lumbar or abdominal pain | 15 | 4.1 (1.2-14) |
| 2 | Pain duration (<8 hours) | 20 | 8.0 (1.7-37.5) |
| 3 | Vomiting | 20 | 7.9 (2.3-27) |
| 4 | Absence of leucorrhoea/menorrhagia | 25 | 12.6 (2.3-67.6) |
| 5 | Ovarian cyst >5 cm by USG | 25 | 10.6 (2.9-38.8) |
+CI: Confidence Intervaladmissions
Adnexal and cervical motion tenderness with a palpable tender mass in the anterior/posterior vaginal fornix (as a result of rotation) in presence of a negative urine pregnancy test is another reliable sign. However, this examination could only be attempted in married/parous women with informed consent.
Statistical Analysis
Simple measures like specificity, sensitivity, PPV were calculated in both groups and compared between the two groups using Fischer’s-exact test for significance.
Results
A total of 374 patients admitted as gynaecological emergencies in the two year period from August 2015 to August 2017. Out of which 315 (84.2%) were ectopic pregnancies and were omitted. Of the remaining 59 women with a negative urine pregnancy test, there were 33 admissions for heavy menstrual bleeding/puberty menorrhagia, women with advanced cervical malignancy with severe bleeding/uraemia, and advanced ovarian malignancy with acute/sub-acute bowel obstruction. Having ruled out ectopic pregnancies, 26 women were emergency admissions with clinical suspicion of cyst accidents (6.9% of all gynaecological emergencies), with actual cyst accidents including torsion noted in 19 (5%) women and torsion noted in 14 (3.7%) of these women respectively [Table/Fig-2]. Five women had haemorrhagic cysts. The mean age of these 26 women was 25.54±6.61 years, the youngest being 18 years and oldest of 40 years. They were randomly distributed as 14 emergency Intervaladmissions in units using the clinical scoring [Table/Fig-1], and 12 in which no formal scoring was used. The scoring enabled us to plan surgery for 9 patients with suspected torsion, all of whom scored more than 60 using Huchon’s scoring. The diagnosis was proved to be correct in eight women with sensitivity of 100%, specificity of 83.3% and PPV of 88.9%, positive Likelihood Ratio (LR+) of 5.98; one patient however was found to have a haemorrhagic cyst intraoperatively [Table/Fig-2]. The scoring enabled us to rule out 5 other women with acute onset pain, with two of them diagnosed as Pelvic Inflammatory Disease (PID) as straight forward exclusions. Both had vaginal discharge/leucorrhoea and no cysts on ultrasound. One of them presented with right iliac fossa pain over last few days (increased in last 24 hours) and the other had chronic abdominal pain with vomiting and fever, resulting in total scores of 15 and 35 respectively. Both received intravenous and oral antibiotics; as per CDC in patient PID treatment guidelines, and responded well.
Distribution of patients.
| Scoring used (n=14) | Scoring not used (n=12) | Total (n=26) |
|---|
| Suspected torsion with score >60 and surgery (n=9) | Low risk score and conservative management (n=5) | Suspected torsion (n=10) and surgery | Clinically not suspected torsion | Total suspected torsion and surgery (scoring+non-scoring) n=19 |
| Actual torsion=8+one haemorrhagic cyst | 3 haemorrhagic cysts+2PID | Actual torsion n=6 +2 appendicular mass+1 To mass+1 ruptured chocolate cyst | 1 haemorrhagic cyst* +1 endometrioma | Total actual torsion n=14 |
TO mass: tubo-ovarian mass; PID: Pelvic inflammatory disease
*One lady with initial conservative management for haemorrhagic cyst in non-scoring group had to be operated later for enlarging cyst with intra-cystic haemorrhage and deterioration of vitals
The other three women in the scoring group but managed conservatively finally, were trickier to exclude. All three had acute abdominal pain less than 8 hours, with two among them having vomiting and fever in one. So they respectively scored total of 35, 55 and 55 (fever not included in scoring). All three had adnexal masses of less than 5 cm and no vaginal discharge/bleeding. There was no leukocytosis and C-reactive Protein (CRP) levels were normal and while there was adnexal tenderness, observations were normal and no acute abdominal tenderness/rigidity. The ultrasound in the latter two women with scores of 55, had appearances of 3.5 cm and 4 cm congested cysts with no changes in Doppler flow. Hence, all three were managed conservatively with analgesics with a clinical impression of haemorrhagic cysts, and recovered well.
The ‘non-scoring’ group however had 10 women operated upon with only 6 found to have adnexal torsion (sensitivity of 100%, specificity of 33.33%, PPV of 60%, LR+ of 1.49) as depicted in [Table/Fig-2]. By applying Fischer’s-exact test for comparing these 2 methods of screening for adnexal torsion in two different groups of women, only the specificity was found to be statistically significant (p=0.03), implying Huchon’s method being more reliable in ruling out torsion by identifying the true negatives, while there was no obvious difference in detecting number of true positives with torsion. Two women, in the non-scoring group with clinical suspicion of torsion were operated and had appendicular masses with a bulky ovary and small 3-4 cm simple ovarian cyst respectively. The other two had a ruptured chocolate cyst, and a complex tubo-ovarian 5 cm mass who had clinical symptoms and signs just like a cyst accident. Ultrasound did not provide conclusive evidence to overturn the clinical diagnosis of torsion in these patients, highlighting the limitations of an emergency ultrasound done by junior staff as well as limitations in clinical diagnosis.
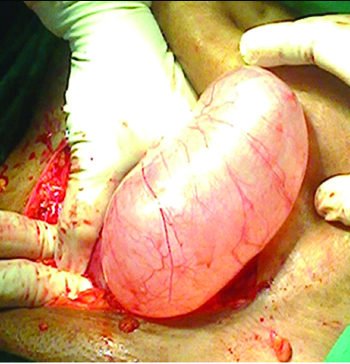
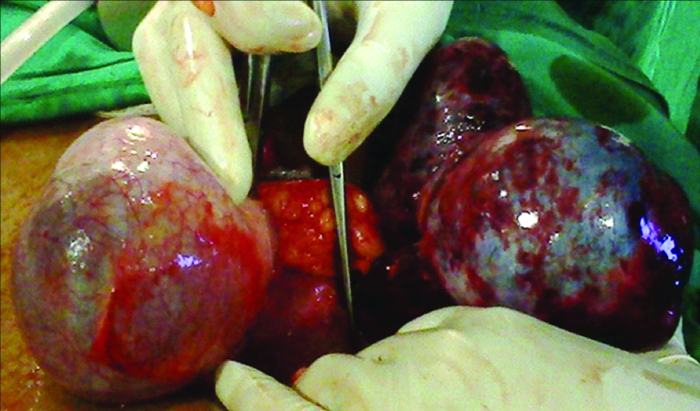
Four of the 14 women with torsion had para-ovarian fimbrial cysts. Interestingly these cysts were neither haemorrhagic nor gangrenous and we could attempt cyst excision after de-torsion [Table/Fig-3]. All the four women underwent para-ovarian/fimbrial cystectomies. The ovarian cysts with torsion were haemorrhagic and congested [Table/Fig-4] and it was very difficult to achieve de-torsion after long term twisting. Any attempt in such cases resulted in rupture of the pedicle and spillage of haemorrhagic material intra-peritoneally.
Fimbrial cyst with one loop torsion amenable to de-torsion.
Congested haemorrhagic twisted ovarian cyst.

The 10 women with ovarian torsion had predominantly dermoids (n=7) as histopathological diagnoses, while two were mucinous and one was serous cystadenomas. Of the 10 women with ovarian torsion, four women underwent detorsion and dermoid cystectomy, four women underwent corresponding side salpingo-ovariotomy, while two women underwent bilateral salpingo-ovariotomy due to contra-lateral diseased ovaries.
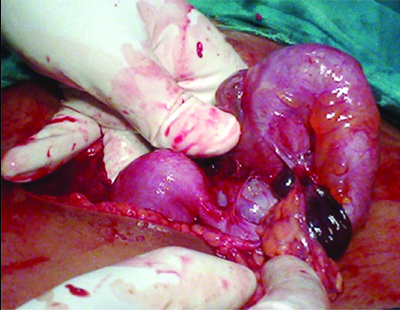
We experienced a number of unique scenarios when dealing with gynaecological emergencies suspected to be torsion. In one such case a 35-year-old with one child previously had presented with on and off lower abdominal pain that had worsened over the preceding eight days. Her last menstrual period was one week back and she had two episodes of vomiting but no fever. There was history of tubal ligation two years back. A urine pregnancy test was negative, and she was febrile with a temperature of 100° F. Abdominal examination revealed tenderness over right iliac fossa and on vaginal examination a mass was palpable in the right fornix with severe cervical motion tenderness. However the emergency ultrasound revealed a heterogenous right adnexal mass 5×6 cm adjacent to a clear left ovarian cyst of 6×7 cm. CA-125 level:31.21 IU/lt. Intraoperatively we noted to our surprise that there were bilateral ovarian masses [Table/Fig-5,6]; and the left sided ovarian mass was completely congested and gangrenous and shifted to the right, having twisted itself on the long pedicle of a clear cyst arising from right adnexa which in turn appears to the left [Table/Fig-5]. The proper anatomic orientation can be made out after excising the left sided gangrenous haemorrhagic ovarian mass and enucleating the right sided clear cyst (retaining the right normal ovary) that was revealed to be a serous cystadenoma on histopathology. The tight twisting of the pedicles did not permit untwisting and any attempt at salvaging the left ovary.
Both adnexal masses twisted on pedicles.
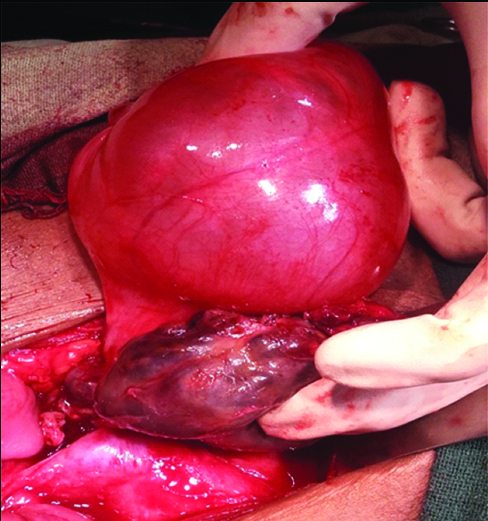
Correct orientation after excising cysts.
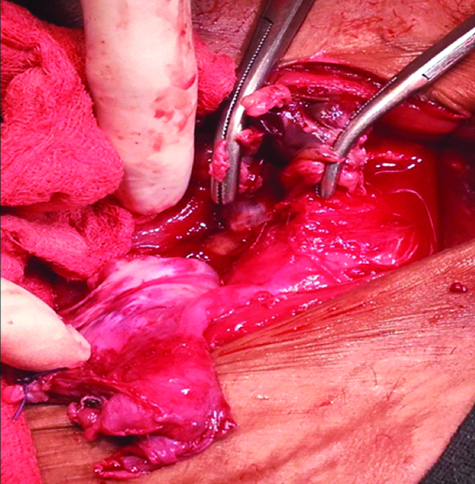
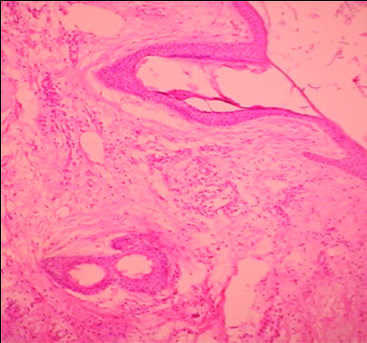
Yet another 23-year-old lady married but with no children, presented with severe lower abdominal pain for two days along with vomiting the previous day night. She had a pulse rate of 120/minute and abdominal examination revealed a large bosselated pelvic mass. USG was suggestive of a bulky haemorrhagic left sided ovary of 12×9 cm with a well defined hetero-echoic space occupying lesion of 7×5 cm within it, having focus of calcification, placed antero-superior to the uterus. To complicate matters, there was another large heterogeneous right sided mass of 7.6×7.2 cm with foci of calcification, and the ovaries could not be visualised separately bilaterally. This was a diagnosis of bilateral dermoids, confirmed by histopathology [Table/Fig-7], with the left sided having undergone torsion [Table/Fig-8] and completely congested and haemorrhagic. The left ovary could not be salvaged, while the right dermoid was enucleated and the right ovary preserved. She had onset of regular menses four weeks after surgery.
Neural elements with thyroid like glands in between (H&E stain; 10X).
Bilateral dermoids with left ovarian torsion
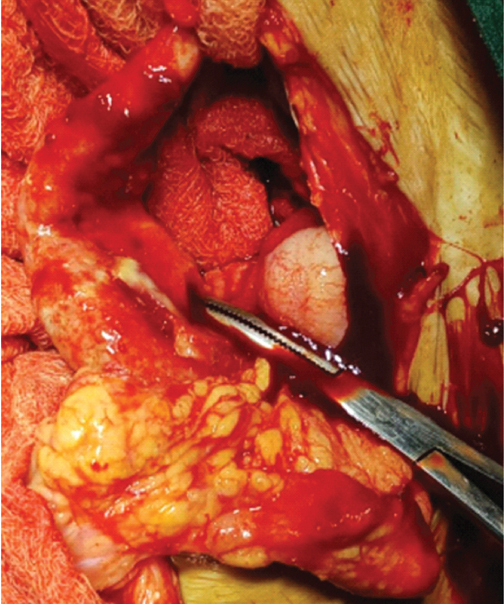
Overconfidence of a diagnosis of a torsion ovary with tell-tale acute abdominal symptoms in presence of an ovarian cyst on ultrasound, having ruled out an ectopic pregnancy, is also fraught with danger. The following scenario describes one such situation. This was a 32-year-old lady having completed her family, and presenting with severe suprapubic and right iliac fossa pain, along with fever and vomiting for four days. The emergency ultrasound was suggestive of a right ovarian cyst of 3×2 cm with free fluid and normal adnexal Doppler flow. The appendix could not be visualised, and while my senior consultant was confident of a diagnosis of torsion ovary, the size of the ovary just seemed to be too small. Thankfully due to high index of suspicion, the surgeon was at hand to remove the large, inflamed appendix encased with omental inflammation [Table/Fig-9,10] that we noticed intraoperative; the right ovary just bulky, but definitely did not mandate removal.
Enlarged inflamed appendix.

Encased by mass of omentum.
There was another unmarried 19-year-old girl who complained of acute left lower abdominal pain over last 1-2 weeks with concomitant fever and nausea. The emergency abdominal USG was suggestive of left complex tubo-ovarian mass with decreased blood flow on Doppler study. She was managed conservatively with intravenous antibiotics however, persisting pain and fever after 72 hours resulted in a decision for surgery. Here again our main suspicion was torsion though we had the differential diagnosis of chronic PID in mind. The latter was ultimately found intra-operative as evidenced by the retort shaped pus filled tube [Table/Fig-11]. She underwent left salpingo-ovariotomy followed by a further 14 day course of i.v., antibiotics in line with CDC guidance for inpatient treatment of PID.
Chronic PID with tubo-ovarian mass and retort-shaped fallopian tube; masquerading as cyst accident.
Discussion
Huchon’s scoring to screen for torsion among patients presenting with adnexal cyst accidents, involves a systematic approach using five key clinical/radiological parameters. The two most important parameters among these five parameters were absence of leucorrhoea and menorrhagia and cyst size >5 cm on USG and this trend was also noted in present study. However a limitation of Huchon’s study is that, being retrospective in essence, the high percentage of torsion rate may have been due to referral bias. Present study, while involving much smaller study in a single institute, provides a clearer picture of validity, due to its prospective nature. There also needs to be more clarity with those patients with total Huchon’s score falling into the intermediate range of 41-60 but overall, clinically strong suspicion of torsion. We have attempted to elucidate that, by adding other clinical parameters to screen such patients and did not miss out any torsion by our approach. Making a score >40 as high risk would have resulted in higher number of false positives and negative laparotomies/laparoscopies, and hence a higher cut-off score of 60 was chosen and proven to be correct in present study. Currently there are no other studies in literature who have adapted this scoring to screen for adnexal torsion, so there is limited scope for comparison. The less reliance on ultrasound alone also is an advantage of this scoring system. The most common ultrasound feature in torsion is ovarian congestion, and this is no different from other cyst accidents. The clinical features in the scoring will help in detecting torsion better in such situations.
Having excluded ectopic pregnancies, when faced with possibility of cyst accidents, torsion can often be confused for endometriosis, PID with tubo-ovarian abscess, simple cyst with appendicular masses among others. Nausea and vomiting is seen in 85% of women with adnexal torsion [7]. The pain may manifest as acute on chronic, particularly when torsion occurs in a setting of dermoid cysts, fluctuating, often radiating to loin or thigh. Low grade pyrexia with tachycardia is present. Abdominal tenderness is generalised but may be localised with guarding and rebound tenderness. Vaginal examination reveals cervical tenderness, adnexal tenderness and palpable adnexal mass through the fornices. Some studies suggest torsion may be more common when cyst size is greater than 5 cm [6,8]. Indeed in the scoring system adopted in our study, this was the most important feature that helped us to distinguish torsion from other types of cyst accidents. In the two cases with the ultimate diagnosis of appendicular abscess, while it was not picked up in ultrasound, torsion was less likely due to the smaller size of adnexal cysts and thus would have helped in having a clinical suspicion of appendicular lump and have a surgeon on standby and tailor the abdominal incision accordingly. Only one had the typical pain at McBurney’s point but both had acute pain of more than 8 hours with vomiting. On ultrasound the appendices were not seen and further imaging (CT/MRI) were limited by time and cost constraints. While both these patients had been randomised into non-scoring group; a retrospective scoring revealed scores of 35 and 55 respectively. The feature of pain less than 8 hours in absence of leucorrhoea was also helpful in going in favour of torsion instead of chronic PID when ultrasound appearances are equivocal.
Among the differentials, PID will be characterised by non-migratory pelvic pain in absence of nausea and vomiting. Appendicitis initially presents with poorly localised colicky lower central abdominal pain with anorexia, vomiting that gradually localises to right iliac fossa tenderness with guarding and rigidity with time. Sudden onset sharp, stabbing pain may indicate haemorrhage into a functional ovarian cyst. Complaints of bloating pelvic pain, nausea in a lady with history of ovulation induction may raise suspicion of ovarian hyperstimulation syndrome as a rare but possible differential diagnosis. Fibroid degeneration is uncommon outside of pregnancy. Renal colic will manifest with sudden onset colicky pain radiating from loin to groin mimicking torsion, but may be associated with microscopic haematuria.
At times when cyst haemorrhage is suspected instead of torsion, the initial tendency is to go for conservative management with fluids, NSAIDs for pain relief alongside vitals monitoring. At night in the presence of relatively less experienced radiologists who often give a confusing radiological diagnosis like a haemorrhagic cyst; it’s the clinical skill which will decide the further course of action. Large corpus luteal haemorrhagic cysts may have intraperitoneal haemorrhage and may not respond conservatively; gradually destabilising vitals is a prompt to thinking in terms of surgery. Just a radiological report of haemorrhagic cyst should be dealt with caution: even with torsion, cysts tend to be haemorrhagic but difficult to make a diagnosis till Doppler study of the suspected twisted vessels is made; either there will be an absent or reduced flow or a whirlpool sign. In fact the ultrasound appearance of torsion of a normal ovary may be highly variable; frequently it is described as unilateral enlargement of the ovary with oedema and peripherally arranged follicles [9]. It may also appear as a solid mass with hyper or hypoechoic areas [10] denoting areas of haemorrhage and necrosis. The twisted pedicle may be seen as a whirlpool on both grey scale and colour Doppler [11] and increases sensitivity of the diagnosis of torsion. However, ovarian enlargement with oedema appears to be the most common sonological sign across literature. While several studies have quoted doppler abnormalities in 100% cases of torsion [12], complete absence of perfusion is a relatively late event, and presence of perfusion does not rule out the diagnosis of torsion [9]. This complicates the clinical picture and the variable ultrasound appearances thus partially justify the clinical confusion that prevails even when the diagnosis of cyst accident is suspected. CT-scan and MRI may help in clearing the picture but may not be cost effective. Serum markers particularly the pro-inflammatory ones like CRP, interleukins and tumour necrosis factor may be elevated but are non-specific for adnexal torsion.
The definitive management of these patients with torsion is no longer straight forward with the decision for surgery determined by the patient’s age, menopausal or not, fertility consideration. Traditionally described surgeries include partial or complete salpingo-oophorectomies. However evidence suggest the haemorrhagic, necrosed appearance of torted ovaries do not correlate with residual function; in fact laparoscopic de-torsion has been associated with good long term outcomes even when the ovaries have turned dark purple or black [13,14]. Studies from a paediatric series of torsion of normal ovaries also support de-torsion with or without oophoropexy. However torsion duration of greater than 48 hours resulted in worsening of the prognosis [15], so de-torsion if possible should be attempted at the earliest. We did not experience any torsion of normal ovaries in present study, mostly they were associated with dermoid cysts and needed cyst removal and where this was not possible salpingo-oophorectomy. As discussed earlier the patients with torsion referred to us came quite late after initial onset of symptoms, and thus were not amenable for conservative surgeries like de-torsion. In fact in cases where torsion has happened in case of a true ovarian cyst, de-torsion and cystectomy in same sitting is often not advised due to friable nature of tissues and cystectomy 2-3 weeks after de-torsion has been described in literature [7]. The evidence regarding oophoropexy is less convincing and may be attempted in cases of recurrent torsion [16].
Limitation
This study is limited by the small numbers, which in turn is also reflected in the limited statistics and conclusions that can be drawn from this. However, this score does appear as a promising tool to screen torsion and can be adopted by a larger study across multiple centres over a longer period of time, in an attempt to detect torsion early and reliably.
Conclusion
At present there are no prediction tools available for detecting adnexal torsion. This scoring involves clinical and radiological signs only, and does not involve complex Doppler studies, and hence can be adopted by junior gynaecological residents/radiologists to better detect torsion.
+CI: Confidence Intervaladmissions
TO mass: tubo-ovarian mass; PID: Pelvic inflammatory disease*One lady with initial conservative management for haemorrhagic cyst in non-scoring group had to be operated later for enlarging cyst with intra-cystic haemorrhage and deterioration of vitals