Normal eruption of teeth is considered a critical phase for the development of hard and soft tissue apparatus of the craniofacial system. Disturbance in tooth eruption, in general, may lead to delay of eruption time or abnormal eruption position or both. Early orthodontic assessment and intervention can have a decisive role in the future of ectopically erupting or impacted teeth. While, the objective of orthodontics in these cases is to return teeth to their normal position within the alveolar housing, it may be complicated by deficiencies in hard and soft tissue surrounding these teeth. This paper presents a successful management of ectopically impacted maxillary central incisor by a combined periodontal surgery and orthodontic treatment.
Ectopic eruption, Periodontal surgery, Tooth impaction
Case Report
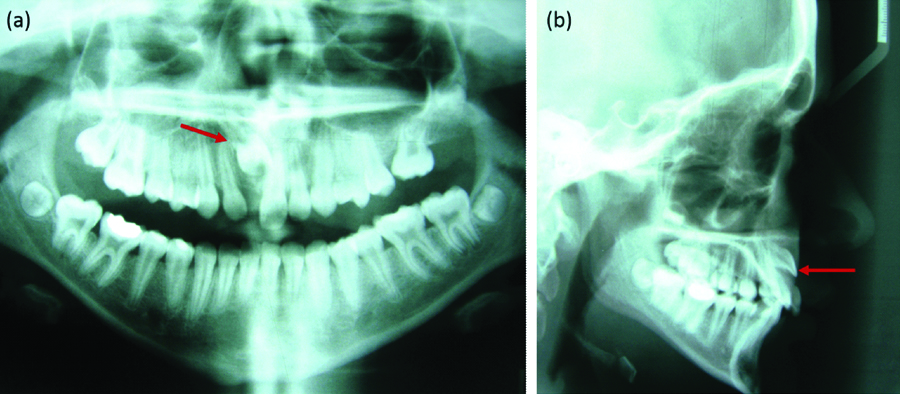
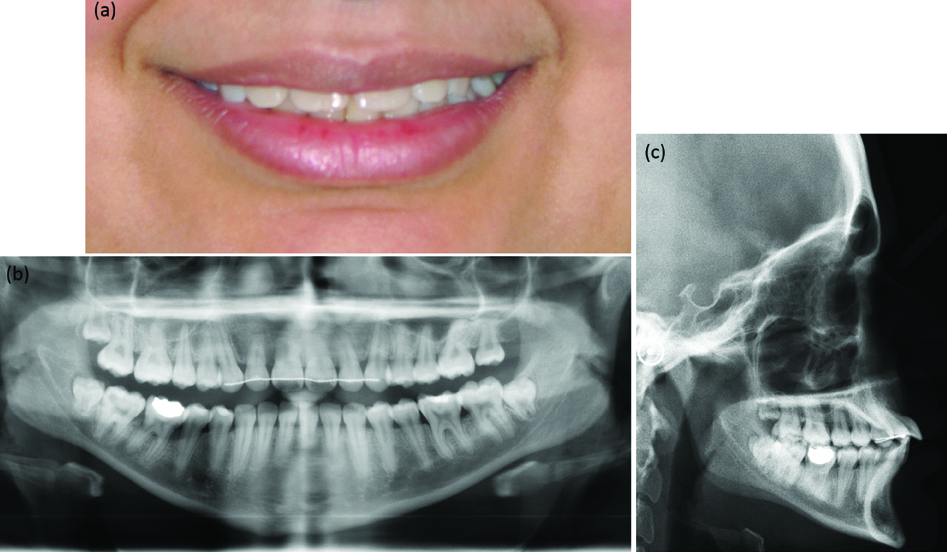
A 12-year-old healthy girl with an unremarkable medical history presented to the orthodontic clinic with a chief complaint of unerupted upper right anterior tooth [Table/Fig-1a]. On intraoral examination, tooth #11 was visible in the vestibular area [Table/Fig-1b], class I malocclusion with a moderately crowded upper anterior segment, rotated upper left first premolar, and extracted upper left first molar, which was severely decayed. The early extraction resulted in mesiopalatal rotation of the adjacent second molar [Table/Fig-1c]. Radiographic evaluation revealed the vertical location of tooth #11 in the apical third of adjacent teeth, with more labial path of eruption [Table/Fig-2a,b]. There was a history of multiple odontomas in the region of tooth #11. Although, the odontomas were surgically removed one year previously, no signs of eruption progression were observed, indicating the need for proper orthodontic assessment and intervention. Furthermore, the crown of tooth #11 was clearly bulging labially, exhibiting distinct labio-version orientation of the tooth. Given that, the root was likely to follow the same labial positioning path, a provisional periodontal prognosis was established, and an effort was made to maximise the keratinised gingival zone upon completion of forced eruption. Early collaboration was established with a periodontist to ensure this multidisciplinary goal was achieved.
Initial view: a) Extraoral front photo showing #21 in midline position. b) Intraoral front photo showing the profile of impacted tooth #11 in vestibular area and narrow spacing. c) Occlusal view showing labial deficiency of area #11 and mesiopalatal rotation of tooth #27.

Radiographic evaluation show: a) Panoramic radiograph indicate location of tooth #11 relative to adjacent incisors. b) Lateral cephalometric radiograph indicate the labioeruption pattern for #11.
The treatment plan included construction of a Trans Palatal Arch (TPA) to derotate the upper left second molar, followed by stabilisation and correction and space maintenance using a Nance appliance. This process was to be followed with comprehensive fixed upper appliance therapy to level and align the upper teeth, create space for impacted tooth #11, expose the active eruption of the impacted tooth and realign the upper arch. The treatment plan was initiated soon after consent from the patient’s parents was obtained, and the activated TPA was cemented. Two months later, the second molar rotation was corrected and a Nance appliance was then cemented to initiate upper fixed appliance therapy using a 0.022″ slot bracket. After a series of flexible and stainless-steel arch wires, and the use of open coil springs, alignment was completed and space was re-established for the impacted tooth.
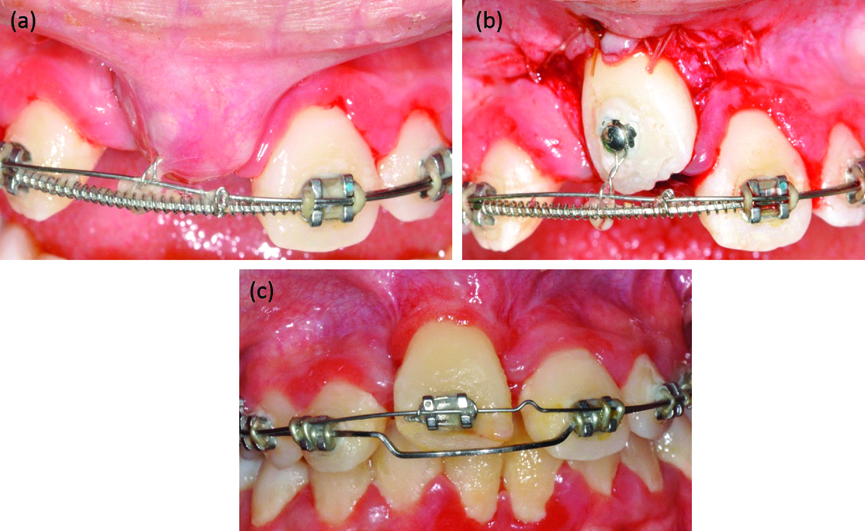
One year later, the case was referred for surgical exposure of tooth #11 and bonding of the gold chain attachment. This was followed by an overlay arch wire technique to facilitate eruption of the impacted tooth [Table/Fig-3a,b]. A combination of 0.019″×0.025″ base stainless-steel and 0.014″ Nickel Titanium (Niti) arch wire was used successfully for that purpose. After two activations, a new panoramic radiograph revealed satisfactory root alignment without root resorption. Thereafter, a bracket was bonded onto tooth #11 to continue levelling and alignment [Table/Fig-3c].
Intraoral photos show: a) Mucosal tissue covering tooth #11 with bracket attached to ortho wire. b) Exposure of tooth #11 after apically positioned flap. c) Initial alignment of tooth #11 and healing of soft tissue after six weeks of exposure and wire activation.
Cone Beam Computed Tomography Assessment
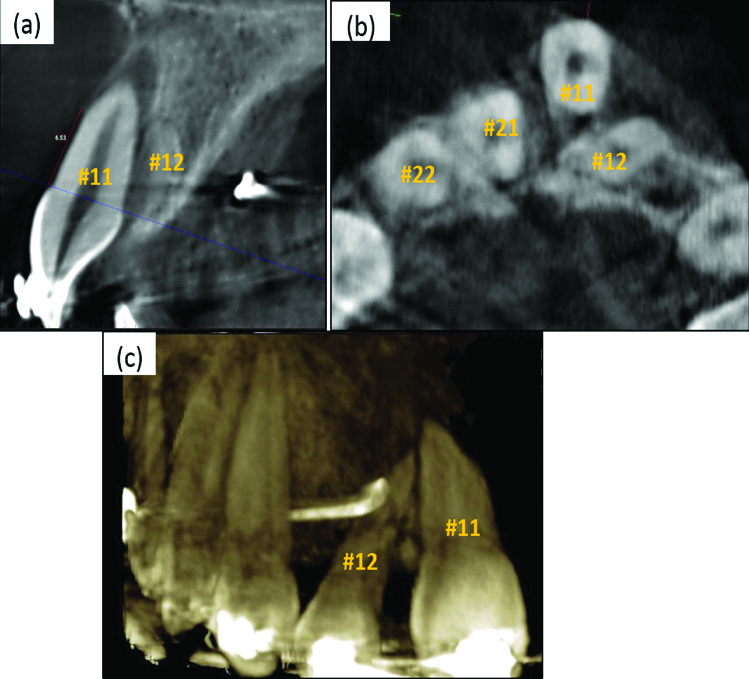
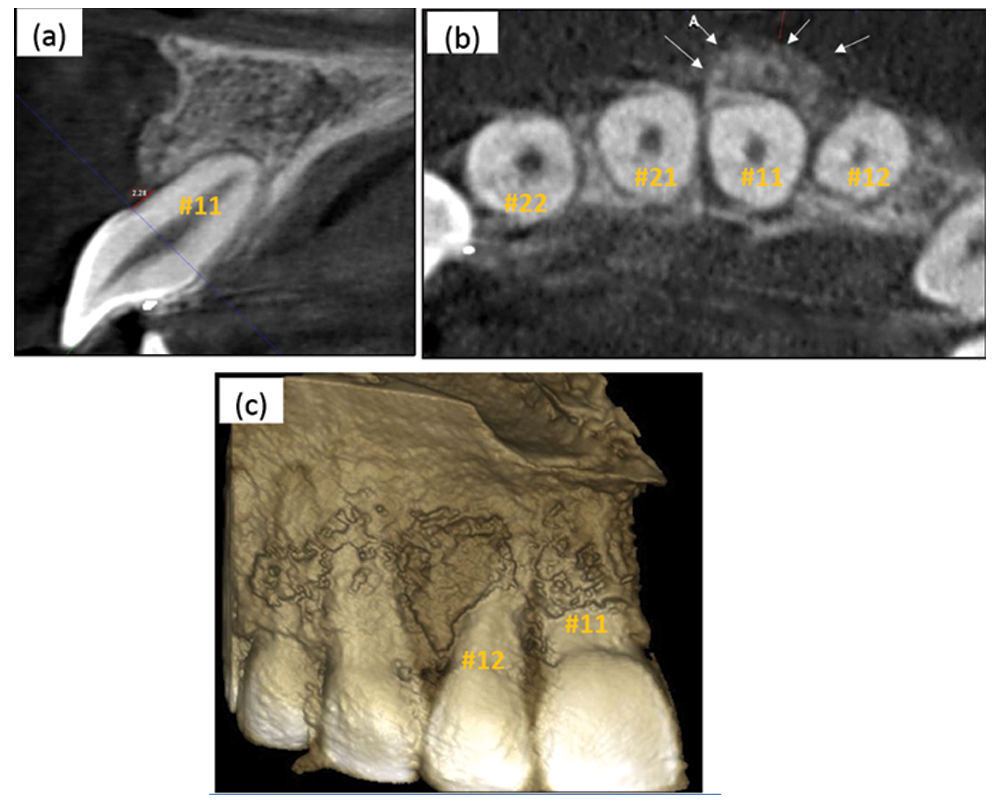
After reviewing treatment progress with a periodontist, Cone Beam Computed Tomography (CBCT) was performed to evaluate the bone level and positioning of teeth #11 and #12. Careful examination confirmed that root formation of teeth #11 and #12 was complete. Additionally, it was noted that tooth #11 was positioned labially relative to the dental arch, while the root apex of #12 was located palatal to #11 [Table/Fig-4a]. No lamina dura and very little interdental space were noted between #11 and #12 [Table/Fig-4b]. A significant amount of bone loss labial to 11 was noted and measured; there were no signs of ankylosis.
CBCT images during orthodontic phase revealed: a) Sagittal view indicate labial positioning of #11 with significant loss of labial bone, while root apex of #12 is positioned palatal relative to #11. b) Axial view shows labial positioning (out of the dental arch) of #11 at the middle third of the roots with loss of lamina dura relative to #12. c) 3D reconstruction shows improper orientation of tooth #12 relative to #11 within the alveolar arch.
Periodontal Surgical Management
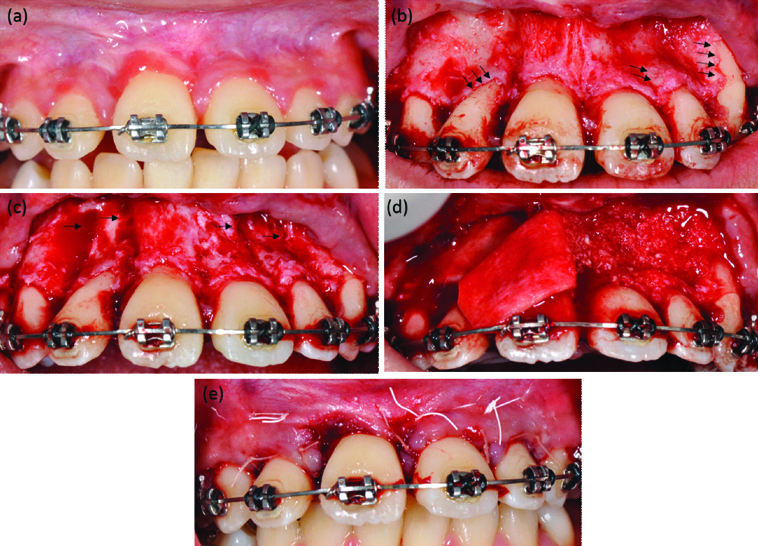
Clinical evaluation for anterior teeth showed acceptable level of Keratinised Gingiva (KG) except for tooth #11 where there was lack of KG, average probing depth measurement was 3 mm except tooth #11 it was 1 mm. Bleeding on probing was evident in all teeth due to poor oral hygiene. Radiographic findings indicated requirement of periodontal therapy for facilitating movement of teeth and augmenting hard and soft tissue around areas of #11 and #12. The patient underwent full mouth debridement including supra- and sub-gingival scaling; oral hygiene instructions were reinforced. One week later, periodontal surgery was performed, which involved palatal and buccal decortications of bony plates from teeth #13 to #23 [Table/Fig-5a-c], followed by bone grafting using slowly resorbing xenogenic bone particles (Bio-Oss, Geistlich Pharma AG, Wolhusen, Switzerland) covered with resorbable tissue matrix (Puros Dermis allograft, Zimmer Biomet Dental, Palm Beach Gardens, FL, USA) to enhance and maintain tissue volume in the area of the upper incisors, then sutured by nylon 4-0 (Ethilon*) non resorbable and Vicryl™ 5-0 resorbable sutures (©Ethicon, Inc) [Table/Fig-5d]. Three weeks later, orthodontic therapy was resumed with placement of a series of aligning arch wires, with individual palatal root torque directed on tooth #11 to further position its root within the alveolar bone to create a more favourable periodontal condition. The patient attended recall periodontal visits every three months owing to poor oral hygiene and recurrent biofilm formation in the area of concern.
Intraoral photos showing: a) Front view the day of surgery with acceptable gingival health. b) Flap reflection revealed areas of fenestration and dehiscence in teeth 12, 11, 22, 23 with depression on the buccal bone plate. c) After buccal decortication mainly in the proximal bone. d) Placing bone particulate followed by tissue matrix allograft. d) Primary closure achieved using resorbable and non resorbable sutures..
Continuing Orthodontic Therapy
Individual torque application began with 0.017″×0.025″ and 0.019″×0.025″ stainless-steel wires. Overjet measurements were recorded from the tip of tooth #11 at each visit to determine the amount of correction gained and to monitor progress. Once final symmetrical alignment between the upper two central incisors was achieved and, on simultaneous recommendation from the periodontist, the teeth were debonded and a fixed upper palatal retainer was placed from canine to canine. The fixed retention ensures stability in addition to serving as a stent after periodontal surgery. The limited “upper only” orthodontic treatment plan, inspite of the bimaxillary protrusion presented [Table/Fig-6], has rendered finishing the overjet in a compromised increased value that was accepted by the patient’s guardians. Additionally, their desire to avoid premolar extractions and to limit treatment duration, that lasted for three and a half years, hindered performing a more comprehensive orthodontic treatment.
Final view: a) Extraoral front photo showing corrected midline position of teeth. b) Panoramic radiograph reveal good spacing between upper anterior teeth. c) Lateral cephalometric image reveal the prominent overjet of upper centrals.
At the six month recall visit, CBCT was performed for the upper anterior area focusing on tooth #11 to evaluate postsurgical tooth/root orientation relative to the arch and bony housing [Table/Fig-7a-c], which revealed improved outcome compared with the initial presentation. However, clinical examination of the area around tooth #11 revealed persistent localised gingival inflammation due to minimal KG and shallow vestibular depth. After discussing options with the patient’s guardian and to avoid possible future complications, it was decided to perform gingival augmentation in the area of #11 and #12 to reinforce and improve periodontal health condition [Table/Fig-8]. At this stage, the patient is under scheduled recall visit every six months for periodontal maintenance.
CBCT images at six month postsurgery revealed; a) Sagittal view indicating proper positioning of #11 within the bony housing. b) Axial view shows adequate amount of labial bone of #11 at the middle third of the roots. c) 3D reconstruction shows proper orientation and alignment of tooth #12 relative to #11 within the alveolar arch.
Intra oral photos show: a) Lack of keratinised gingiva in area of tooth 11 with signs of bleeding and inflammation. b) One month post gingival graft surgery with adequate amount of keratinised tissue and healthy periodontium.

Discussion
Although, impacted maxillary incisor is less common, it is a reason of aesthetic concern in young children [1,2]. The concurrent interdisciplinary orthodontic and periodontal approach is well documented in the literature [3,4]. A combined treatment protocol would help reducing level of inflammatory cytokines, improving the prognosis of drifted teeth in cases with periodontal disease and rendering better aesthetic outcomes [5-7]. Earlier combined orthodontic and periodontal treatment cases published focus on aspects such as implant site development and management of bony defects associated with teeth displacement [8,9]. The present case focused on illustrating the role of combined therapy in improving labial bony defect related to ectopic eruption.
The beneficial role of CBCT imaging in cases of impacted teeth is of diagnostic and prognostic significance [1]. The precise location of the impacted teeth is determined eliminating the super impositions evident in plane film radiography [2]. The choice of CBCT facilitated the surgical procedures for enabling the minimally traumatic exposure and guided movement of the impacted teeth. This in turn will enhance the favourable outcome for vital tooth eruption and future stabilisation. Additionally, CBCT also enabled orthodontists in appropriate measurements of space discrepancies and appropriate auxiliary appliance design.
A key aspect in the orthodontic mechanical management is the application of palatal root torque. The combination of force application in palatal direction with palatal corticotomies has facilitated the correction of the root position of impacted tooth #11. The effect of performing corticotomies prior to orthodontic movement was shown to enhance and accelerate tooth movement [10]. Early detection of the bony defect can ensure proper prognosis assessment and suitable interdisciplinary management. Also, the literature shows that CBCT was an accurate vital tool in the continuous evaluation of alveolar bone remodeling during orthodontic periodontal treatment [11].
The periodontal management of bony defect site with anteriorly displaced incisors, similar to the present case, was shown to improve with conducive periodontal conditions [12]. In the present case, thin bony housing was a major challenge with significant impact on the prognosis of tooth #11. Tooth movement in compromised periodontal conditions was unfavourable with concurrent reduction in bone volume and density [13]. In present case, we managed to overcome any potential loss by performing alveolar decortication combined with bone and tissue augmentation to accelerate teeth movement while maintaining the health of teeth supporting tissues. The impact of this procedure also influences the treatment time, differential tooth movement, increased traction of impacted teeth and post-orthodontic stability [14]. Additionally, patient’s compliance in oral hygiene maintenance may be reduced and this can increase the biofilm formation, especially in fixed metal appliances [15]. This shortcoming could be overcome by accelerating tooth movement and thus reducing the time period of treatment and possible patient’s negligence.
Conclusion
Patients with impacted anterior teeth and compromised initial bony position benefit from early orthodontic/periodontal collaboration. Biomechanical and orthodontic force orientation assessment should complement periodontal intervention aimed toward improving the surrounding supporting structure.
[1]. Xue JJ, Ye NS, Li JY, Lai WL, Management of an impacted maxillary central incisor with dilacerated rootSaudi Med J 2013 34(10):1073-79. [Google Scholar]
[2]. Crawford LB, Impacted maxillary central incisor in mixed dentition treatmentAm J Orthod Dentofacial Orthop 1997 112(1):1-7.10.1016/S0889-5406(97)70266-X [Google Scholar] [CrossRef]
[3]. Gkantidis N, Christou P, Topouzelis N, The orthodontic-periodontic interrelationship in integrated treatment challenges: a systematic reviewJ Oral Rehabil 2010 37(5):377-90.10.1111/j.1365-2842.2010.02068.x20202098 [Google Scholar] [CrossRef] [PubMed]
[4]. Zachrisson BU, Clinical implications of recent orthodontic-periodontic research findingsSemin Orthod 1996 2(1):4-12.10.1016/S1073-8746(96)80034-X [Google Scholar] [CrossRef]
[5]. Zhang J, Zhang AM, Zhang ZM, Jia JL, Sui XX, Yu LR, Efficacy of combined orthodontic-periodontic treatment for patients with periodontitis and its effect on inflammatory cytokines: A comparative studyAm J Orthod Dentofacial Orthop 2017 152(4):494-500.10.1016/j.ajodo.2017.01.02828962734 [Google Scholar] [CrossRef] [PubMed]
[6]. Panchal AH, Patel VG, Bhavsar NV, Mehta HV, Orthodontic-periodont icintervention of pathological migration of maxillary anterior teeth in advanced periodontal diseaseJ Indian Soc Periodontol 2013 17(3):378-82.10.4103/0972-124X.11564624049341 [Google Scholar] [CrossRef] [PubMed]
[7]. Kokich VG, Esthetics: the orthodontic-periodontic restorative connectionSemin Orthod 1996 2(1):21-30.10.1016/S1073-8746(96)80036-3 [Google Scholar] [CrossRef]
[8]. Salama H, Salama M, Kelly J, The orthodontic-periodontal connection in implant site developmentPract Periodontics Aesthet Dent 1996 8(9):923-32. [Google Scholar]
[9]. Kazandjian G, Scopp IW, Stahl S, Combined orthodontic-periodontal treatment of an infrabony defect. A case reportJ Periodontol 1979 50(9):479-82.10.1902/jop.1979.50.9.479385827 [Google Scholar] [CrossRef] [PubMed]
[10]. Hassan AH, Al-Saeed SH, Al-Maghlouth BA, Bahammam MA, Linjawi AI, El-Bialy TH, Corticotomy-assisted orthodontic treatment. A systematic review of the biological basis and clinical effectivenessSaudi Med J 2015 36(7):794-801.10.15537/smj.2015.7.1243726108582 [Google Scholar] [CrossRef] [PubMed]
[11]. Ma ZG, Fan LF, Fang B, The role of CBCT in evaluation of alveolar bone state during orthodontic-periodontal treatmentShanghai Kou Qiang Yi Xue 2010 19(2):113-17. [Google Scholar]
[12]. Cao T, Xu L, Shi J, Zhou Y, Combined orthodontic-periodontal treatment in periodontal patients with anteriorly displaced incisorsAm J Orthod Dentofacial Orthop 2015 148(5):805-13.10.1016/j.ajodo.2015.05.02626522041 [Google Scholar] [CrossRef] [PubMed]
[13]. Machibya FM, Zhuang Y, Guo W, You D, Lin S, Wu D, Effects of bone regeneration materials and tooth movement timing on canine experimental orthodontic treatmentThe Angle orthodontist 2017 10.2319/062017-40729154676 [Google Scholar] [CrossRef] [PubMed]
[14]. Amit G, Jps K, Pankaj B, Suchinder S, Parul B, Periodontally accelerated osteogenic orthodontics (PAOO) - a reviewJournal of clinical and experimentaldentistry 2012 4(5):e292-96.10.4317/jced.5082224455038 [Google Scholar] [CrossRef] [PubMed]
[15]. Lindel ID, Elter C, Heuer W, Heidenblut T, Stiesch M, Schwestka-Polly R, Comparative analysis of long-term biofilm formation on metal and ceramic bracketsThe Angle orthodontist 2011 81(5):907-14.10.2319/102210-616.121542722 [Google Scholar] [CrossRef] [PubMed]