Conus Medullaris Dermoid Rupture into Central Canal: A Case Report
Kanumukul Lakshminarayana Surendra1, Sriram Patwari2, Harsha Chadaga3, Anita Nagadi4, Rekha Priya5
1 Resident, Department of Radiology, Columbia Asia Referral Hospital, Bengaluru, Karnataka, India.
2 Consultant, Department of Radiology, Columbia Asia Referral Hospital, Bengaluru, Karnataka, India.
3 Head, Department of Radiology, Columbia Asia Referral Hospital, Bengaluru, Karnataka, India.
4 Senior Consultant, Department of Radiology, Columbia Asia Referral Hospital, Bengaluru, Karnataka, India.
5 Resident, Department of Radiology, Columbia Asia Referral Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sriram Patwari, Columbia Asia Referral Hospital, 26/4, Brigade Gateway, Beside Metro Cash and Carry West, Malleshwaram-560055, Bengaluru, Karnataka, India.
E-mail: sramdoc@gmail.com
Intramedullary spinal dermoids are benign, uncommon, mostly congenital and slow growing tumours. Here, we present a rare case of ruptured intramedullary dermoid in a 45-year-old male who presented with lower back ache and both lower limb weakness. Magnetic Resonance Imaging (MRI) demonstrated an elongated mass expanding the conus medullaris and displacing the cauda equina with extension into lower thoracic spinal cord and ruptured fat droplets within the central canal of lower thoracic spinal cord. Correlative CT imaging confirmed the presence of fat within the lesion.
Benign tumour, DIXON technique, Intramedullary, Intraspinal
Case Report
A 45-year-old male presented with chronic mild lower back pain and bilateral lower limb weakness since two months, more pronounced on the left side. Pain was dull and intermittent in nature aggravated on moderate degree of physical activity and relieved with rest and analgesics. Power was 4/5 in the both lower limbs and 5/5 in upper limbs. The patient had no sensory or urinary symptoms or gait abnormality. There was no previous history of trauma, infection or surgery.
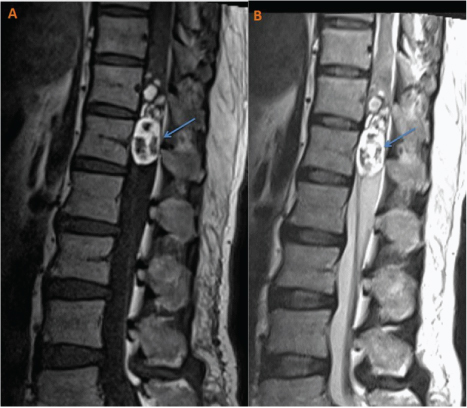
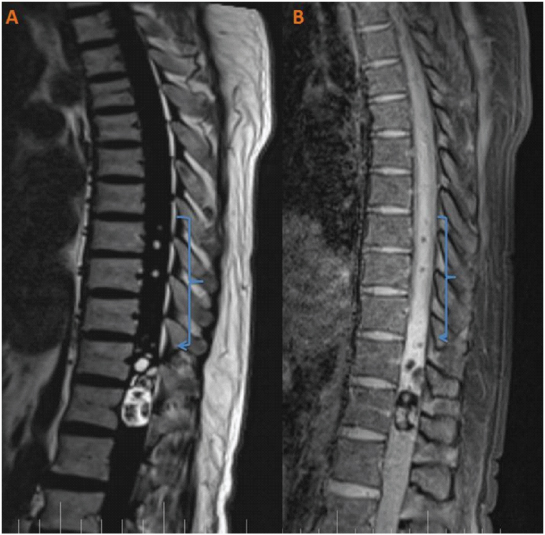
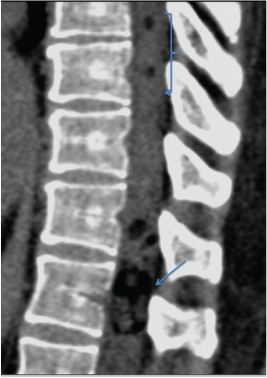
MRI whole spine with IV contrast was performed, which demonstrated an elongated heterogeneous complex cystic mass expanding the conus medullaris measuring 5.5×1.8×2 cm Craniocaudal, Anteroposterior and Transverse (CC×AP×TR) and filling the spinal canal at the level of D11-D12 vertebra. Superiorly the lesion demonstrated extension into the lower thoracic spinal cord and inferiorly causing anterior displacement of the cauda equina nerve roots. The upper margin of the lesion was irregularly marginated. The lesion was heterogeneous in signal characteristics with predominant T1W and T2W hyperintensity. Multiple T1W/T2W hypointense to isointense soft tissue foci were noted within the mid and lower portions of the lesion and a few small loculations were present in the upper portion [Table/Fig-1a,b]. The hyperintense areas of the lesion (on T1W/T2W images) were completely suppressed on fat saturation T1W sequences. The “fat only” images of chemical shift based MRI images (DIXON) showed pronounced bright fatty component within most of the lesion [Table/Fig-2a,b]. Overall these characteristics were consistent with the presence of fat. No post contrast enhancement was seen. No blooming foci were seen on Gradient Recalled Echo images. Apart from this main lesion, few small free fatty foci seen within the central canal of thoracic spinal cord at D8 and D9 levels, suggestive of ruptured fat droplets possibly extruded from the lesion [Table/Fig-3a,b]. No evidence of sinus tract, meningeal herniation, extradural extension, tethered spinal cord, spinal dysraphism or vertebral anomalies seen. Rest of the spinal cord was unremarkable [Table/Fig-4]. Correlative non contrast CT study of spine demonstrated fat attenuating material (–80 to –100 HU) within the lesion [Table/Fig-5]. Considering these typical imaging characteristics, a diagnosis of ruptured intramedullary dermoid into central canal was made. Patient was advised surgery, however lost to further follow up.
T1W and T2W sagittal image showing predominantly hyperintense fat containing intramedullary lesion (arrow) with scattered hypointense to isointense foci within and at conus medullaris.
a) DIXON fat only sagittal image showing predominantly hyperintense intramedullary conus medullaris lesion with scattered fat droplets seen within the central canal; b) DIXON water only sagittal image showing suppression of fatty areas of the lesion and scattered fat droplets in central canal..
T1W sagittal and STIR coronal images showing ruptured fat droplets (arrows) within the central canal in thoracic spinal cord.
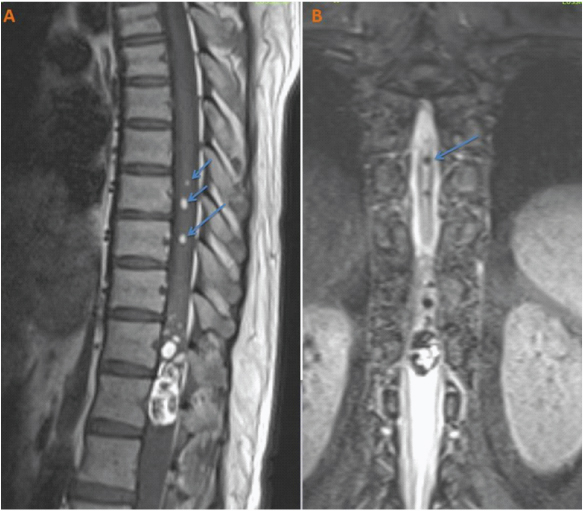
T2W sagittal image of whole spine showing the extent of the fat droplets in central canal (arrows). Rest of the spinal cord is normal.

Correlative sagittal CT image at the level of D12 vertebra demonstrating fat attenuating material (–80 to –100 HU) within the lesion and also showing small fat droplets superior in the central canal in thoracic cord.
Discussion
Spinal dermoids are uncommon, slow growing, benign tumours that can occur anywhere along the neural axis. They constitute only 0.8-1.1% of primary intraspinal tumours and 0.7-0.8% of CNS tumours [1-3]. They are frequently encountered in the paediatric population with prevalence of 5-17% [2]. The vast majority occur in the lumbosacral region, usually in the cauda equina and are extra medullary in location [2,3]. There is slight male predominance.
The aetiology of their origin is debatable. It is proposed that they arise from congenital or acquired ectodermal inclusions [3]. The most widely accepted theory is that between the third and fourth weeks of foetal development, the cells fated for cutaneous ectoderm are abnormally trapped within the neural ectoderm during neural tube closure and eventually tumours arise from these cells [2].
In majority of the cases spinal dermoids are associated with varying degrees of spinal dysraphism, more so particular when presenting in an early age group [3], when presenting in adulthood these are unlikely to be associated with other spinal abnormalities.
Inspite of a slow growing and benign nature they can be associated with significant morbidity, particularly if ruptured or secondarily infected [3]. Once ruptured the fat droplets can travel along the Cerebrospinal Fluid (CSF) pathways and can disseminate within the spinal cord, which was demonstrated in this case [1,3]. Symptoms after acute rupture include headache, paresis, vertigo, visual disturbances, hemiplegia and sometimes coma [1,3,4]. Dissemination into the CSF pathways can result in arachnoiditis, meningitis and even psychiatric disturbances in the long run [1,5].
Conventional radiography and myleography are almost completely replaced with MRI preferably with advanced chemical shift based fat suppression techniques which can demonstrate the exact composition of the lesion, rarely requiring histological confirmation. CT imaging is an important adjuvant for further characterisation of the lesion particularly to demonstrate fat, calcification or haemorrhage.
The combination of fat, fluid, soft tissue, calcification and haemorrhage is diagnostic of dermoid with fat or fluid being major components. Because of varying amounts of each of these components, MRI signal characteristics of the lesion are typically heterogeneous. In the present case, fat was the major component and was demonstrated clearly on T1W, fat suppression and chemical shift sequences and was further confirmed by CT.
The differentials include lipoma, teratoma and ependymoma. Heterogeneity and confirmation of fat presence is diagnostic for dermoid in the present case.
Most of the ruptured dermoids present with fat dissemination in subarachnoid spaces with only few case reports describing isolated intramedullary rupture of dermoids. Sharma M et al., published similar case, wherein patient presented with urinary retention, low backache and no sensory or gait abnormalities [1]. On imaging there was extensive intra spinal dissemination of the ruptured fat droplets within the central canal and subarachnoid spaces upto the level of corticomedullary junction. Where as in the present case, there was limited area of dissemination of the fat droplets only in to the central canal with no evidence of dissemination in to subarachnoid spaces, which is probably the reason for absence of urinary or sensory or gait abnormalities.
Surgery with close observation and follow up for complications is the treatment of choice for ruptured dermoid [1,3,6,7]. Special precautions need to be taken to prevent the further spillage of contents during surgery. Majority of the cases show significant neurological improvement
Conclusion
Intramedullary dermoids are uncommon and usually detected in the first two decades of life. The present case is rare and relatively unique in terms of middle age presentation, intramedullary location, limited spread of ruptured fat droplets in the spinal cord, absence of CSF dissemination and absence of spinal anomalies. Meticulous study of typical signal characteristics and awareness of intramedullary rupture as a complication will aid prompt diagnosis by radiologists. Accurate diagnosis and meticulous surgery can produce positive outcome.
[1]. Sharma M, Mally R, Velho V, Ruptured conus medullaris dermoid cyst with fat droplets in the centralAsian Spine 2013 7(1):50-55.10.4184/asj.2013.7.1.5023508636 [Google Scholar] [CrossRef] [PubMed]
[2]. Falavigna A, Righesso O, Teles AR, Concomitant dermoid cysts of conus medullaris and cauda equinaArq Neuro-Psiquiatr 2009 67(2a):293-96.10.1590/S0004-282X200900020002319547826 [Google Scholar] [CrossRef] [PubMed]
[3]. De Maio PN, Mikulis DJ, Kiehl TR, Guha A, AIRP best cases in radiologic-pathologic correlation: Spinal conus dermoid cyst with lipid disseminationRadiographics 2012 32(4):1215-21.10.1148/rg.32411501822787003 [Google Scholar] [CrossRef] [PubMed]
[4]. Lunardi P, Missori P, Gagliardi FM, Fortuna A, Long-term results of the surgical treatment of spinal dermoid and epidermoid tumorsNeurosurgery 1989 25(6):860-64.10.1227/00006123-198912000-000022601815 [Google Scholar] [CrossRef] [PubMed]
[5]. Cha JG, Paik SH, Park JS, Park SJ, Kim DH, Lee HK, Ruptured spinal dermoid cyst with disseminated intracranial fat dropletsBr J Radiol 2006 79(938):167-69.10.1259/bjr/1723268516489200 [Google Scholar] [CrossRef] [PubMed]
[6]. Sharma NC, Chandra T, Sharma A, Bajaj M, Kundu R, Long-segment intramedullary spinal dermoidIndian J Radiol Imaging 2009 19(2):148-50.10.4103/0971-3026.5084019881072 [Google Scholar] [CrossRef] [PubMed]
[7]. Satyarthee GD, Kumar A, Moscote-Salazar LF, Conus medullaris dermoid tumour. Uncommon presentation of conus medullaris dermoid as an exophytic mass lesionJournal of Romanian Society of Neurosurgery 2017 31(1):97-100.10.1515/romneu-2017-0015 [Google Scholar] [CrossRef]