Nasolabial Extraosseous Benign CD68+ Giant Cell Neoplasm with Low Malignant Potential
Ashok kumar Kapoor1, Surbhi Rajauria2, Akanksha Singh3, Anil Kumar Verma4
1 Pathologist, Department of Pathology, RML Mehrotra Pathology Ltd., Nirala Nagar, Lucknow, Uttar Pradesh, India.
2 Pathologist, Department of Pathology, RML Mehrotra Pathology Ltd., Nirala Nagar, Lucknow, Uttar Pradesh, India.
3 Senior Technician, Department of Pathology, RML Mehrotra Pathology Ltd., Nirala Nagar, Lucknow, Uttar Pradesh, India.
4 Assistant Professor, Department of Pathology, School of Medical Sciences and Research, Sharda University, Greater Noida, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashok Kumar Kapoor, B-171, Nirala Nagar, Lucknow-226020, Uttar Pradesh, India. E-Mail: drashokkapoor2016@gmail.com
The present case report highlights the histopathological features of a small nasolabial tumour in a 22-year-old female. The tumour was adequately excised. It consisted of proliferated Mononuclear Spindle (MNS) cells admixed with numerous giant cells. Tumour was located in superficial subcutaneous tissue. Immunohistochemical (IHC) examination showed strong positivity of giant cells for anti-CD68+ antibody, suggesting their origin from Monocyte-macrophage (MØ) cells. Both MNS cells and giant cells showed strong positive staining with anti-vimentin antibody. In addition, MNS cells did not show nuclear atypia and mitoses. It was finally diagnosed as a Giant Cell Tumour of Soft Tissue (GCT-ST). It is a highly cellular neoplasm. Receptor Activator of Nuclear Factor Kappa-B Ligand (RANKL) expression by MNS cells stimulates osteoclast formation, resorption and osteolysis associated with this tumour. A benign course is expected after complete excision of this tumour.
Mononuclear spindle cells, Spindle cell tumour, Subcutaneous
Case Report
A 22-year-old female presented with a left nasolabial tumour. The tumour was slowly increasing in size for the last several months. It presently measured about 2.5×2×2 cm. Oedema, redness and pain suggesting local inflammation of overlying skin or bleeding were not observed. The tumour was well-circumscribed and had variable consistency. Local invasion of maxilla was not seen. There was no history of trauma and giant cell tumour elsewhere in the body.
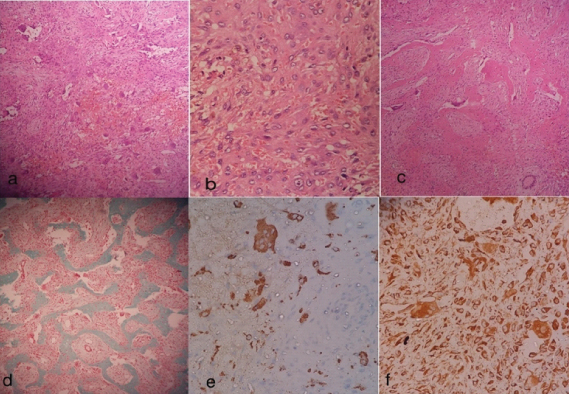
The tumour was surgically excised. Microscopically, it revealed highly cellular neoplasm showing a mixture of MNS cells and multinucleated giant cells. Tumour cells had oval bland nuclei. Number of nuclei varied from 3 to 17 nuclei/giant cell. Nuclei of tumour cells had prominent nucleoli. Nuclear pleomorphism, hyperchromasia and mitoses were not seen in MNS cells. Nuclei of MNS cells and giant cells were identical. Fibrocytic areas and osteoid formation were seen both in the periphery and in the substance of tumour tissue [Table/Fig-1a-c]. Haemorrhagic necrosis and haemorrhagic cyst formation were also seen. Masson-Goldner trichrome stain showed collagen in osteoid tissue [Table/Fig-1d]. IHC examination showed strong positivity of giant cells with anti-CD68+ antibody, suggesting their origin from MØ [Table/Fig-1e]. In addition, anti-vimentin antibody stained both MNS cells and giant cells, suggesting mesenchymal origin of both types of cells [Table/Fig-1f]. Other IHC markers, i.e., S100, HMB45 and pancytokeratin were not tried. The patient was followed for two weeks without any post-operative complication.
a) Tumour showed large number of mononuclear spindle (MNS) cells (H&E 100X); b) MNS cells were admixed with many multinucleated giant cells (H&E 450X); c) Osteoid formation was also seen (H&E 100X); d) Masson-Goldner Trichrome stain showed positive reaction with collagen of osteoid matrix; e) Anti-CD68+ antibody showed strong positivity with giant cells, suggesting their origin from monocytes; f) Anti-vimentin antibody stained both giant cells as well as MNS cells of tumour tissue.
Discussion
The GCT-ST is an extremely rare neoplasm [1,2]. Most important feature of this study was the positivity of multinucleated giant cells for anti-CD68+ antibody. Similar observation was made in another study [1]. CD68+ positivity of giant cells suggested their lineage from MØ cells. Fusion of recruited MØ cells in the lesion might have resulted in formation of giant cells [3]. Further, positive reaction of MNS cells and giant cells with anti-vimentin antibody suggested mesenchymal differentiation. Tumour was separate from maxilla, suggesting its derivation from one of the cells of subcutaneous tissue. GCT-ST has been reported earlier mainly from thigh and rarely from soft tissue of face [1,2]. However, a case has been reported in paravertebral region opposite D3 to D5 vertebra [4]. Moreover, osteogenesis was also discernible in the stromal tissue of tumour. Similar finding has been reported earlier [1]. In addition, the tumour in the index case neither showed nuclear atypia nor mitoses, suggesting its benign nature. Variable mitoses have been reported earlier in GCT-ST [1,3,5]. Rarely, it may metastasise to lung [6]. Clinically, in the present case it was a soft tissue tumour. There was no evidence of local osseous involvement to suggest its origin from bone. Giant Cell Reparative Granuloma (GCRG) was not considered because GCRG is an oral lesion and/or it may be intraoseous and may arise following trauma. Histologically, GCRG has a haemorrhagic background with plump bland fibroblasts, haemosiderin-laden macrophages and fewer giant cells [7]. Conversely, these features were not found in the present tumour. IHC examination of GCT cells with anti S100 reveal positive reaction of some stromal cells [8]. In addition, multinucleated giant cells in GCT are Alpha Anti-Chymo Trypsin (AACT) and M718 positive, indicating their close relationship to macrophage-like stromal cells [8].
Conclusion
The GCT-ST is an extremely rare slow-growing tumour. Complete excision of tumour appeared to cure the patient. However, it may be followed by recurrence and rarely, it may metastasize. Denosumab, a human monoclonal antibody may be useful in the treatment of GCT-ST where complete excision of tumour is not possible.
[1]. Kulkarni MM, Joshi AR, Patil V, Tabassum A, Giant cell tumour of soft tissues of low malignant potential: A rare diagnosis on fine needle aspiration cytologyJ Cytol 2016 33(2):106-08.10.4103/0970-9371.17714427279689 [Google Scholar] [CrossRef] [PubMed]
[2]. Sarita A, Sharma S, Giant cell tumour of soft tissue: Cytological diagnosis of a caseJ Cytol 2009 26(1):33-35.10.4103/0970-9371.5486621938147 [Google Scholar] [CrossRef] [PubMed]
[3]. Chand K, Bhardwaj RK, Rappai TJ, Study of 7 cases of giant cell tumour of soft tissueMed J Armed Forces India 2006 62:138-40.10.1016/S0377-1237(06)80056-0 [Google Scholar] [CrossRef]
[4]. Mazhari NJ, Dhal A, Mandal AK, Giant cell tumour of soft tissue – A case reportInd J Pathol Microbiol 2000 43(3):353-54. [Google Scholar]
[5]. Trabelsi A, Hammedi F, Slama A, Abdelkarim SB, Beizig N, Khochtali H, Giant cell tumour of soft tissue of neck: a case reportN Amer J Med Sci 2009 1(6):319-20. [Google Scholar]
[6]. Oliveira AM, Dei Tos AP, Fletcher CD, Nascimento AG, Primary giant cell tumour of soft tissues: A study of 22 casesAm J Surg Pathol 2000 24(2):248-56.10.1097/00000478-200002000-0001110680893 [Google Scholar] [CrossRef] [PubMed]
[7]. Shah UA, Shah AK, Kumar S, Giant cell reparative granuloma of the jaw: A case reportInd J Radiol Imag 2006 16(4):677-78.10.4103/0971-3026.32297 [Google Scholar] [CrossRef]
[8]. Liu TC, Ji ZM, Wang LT, Giant cell tumours of bone. An immunohistochemical studyPathol Res Pract 1989 185(4):448-53.10.1016/S0344-0338(89)80061-5 [Google Scholar] [CrossRef]