A Giant Hepatic Cyst Mimicking Echinococcosis
Leszek Sułkowski1, Maciej Matyja2, Artur Pasternak3
1 Doctor, Department of General and Vascular Surgery, Regional Specialist Hospital, Czestochowa, Silesia, Poland.
2 Doctor, Department of Endsocopic, Metabolic and Soft Tissue Tumour Surger, Jagiellonian University Medical College, Kraków, Malopolska, Poland.
3 Professor, Department of Anatomy, Jagiellonian University Medical College, Kraków, Malopolska, Poland.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Leszek Sułkowski, Bialska 104/118, Czestochowa, Silesia, Poland.
E-mail: leszeksulkowski@icloud.com
Echinococcosis is a life-threatening disease for humans. It occurs all over the world. We report a case of large and complicated hepatic cyst mimicking the Echinococcosis. A 68-year-old female was referred with epigastric pain. Physical examination did not reveal any abnormality. A giant hepatic cyst with a non-homogeneous content was revealed in ultrasound and Computed Tomography (CT). Due to suspicion of Echinococcosis, she underwent surgery with cystectomy. A non-parasitic cyst localised in the liver may mimic the parasitic ones, especially when they are complicated with septa and non-homogenous content.
Cystectomy, Parasite, Surgery, Zoonosis
Case Report
A 68-year-old female complained of epigastric pain since several weeks. She had no relevant medical or surgical history. Physical examination of her head, neck, thorax, abdomen and limbs revealed no abnormality.
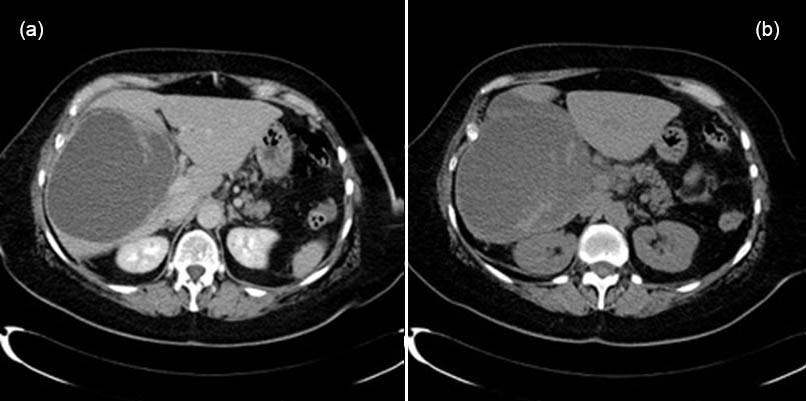
Ultrasound (USG) revealed a giant hepatic cyst with a non-homogeneous content, localised in the right lobe. CT confirmed presence of a cyst with single septa and non-homogenous content in the right lobe of liver [Table/Fig-1a,b].
CT scan of a giant liver cyst with septa, localised in the right lobe.
Due to suspicion of Echinococcosis, the patient underwent surgery. The approach to the abdominal cavity was achieved with an oblique incision in right epigastrium. The examination of abdomen confirmed the presence of a large cyst with a thin wall in the right liver lobe [Table/Fig-2].
Giant liver cyst localised in the right lobe.

The cyst content was aspirated for parasitological examination. Then the cyst was irrigated with ethanol and re-aspirated. Finally, the cyst was excised. The postoperative course was uneventful and the patient was discharged on the seventh postoperative day, in good condition with healing postoperative wound. Pathological examination of resected cyst revealed signs of suppuration in the cystic wall. The cyst content was a hematoma. Parasitological examination was negative, confirming the Echinococcal origin of the cyst.
Discussion
Echinococcosis is a life-threatening disease for humans. It occurs all over the world, not only in developing, but also in developed countries [1]. It is a zoonosis caused by Echinococcus granulosus [2,3]. Dogs and other canids are definitive hosts for this parasite, while sheep and other herbivores are intermediate hosts [1]. Humans are incidentally infected and are accidental intermediate hosts [1,4]. Slowly growing cysts are predominantly located in liver and lungs where parasites are distributed [2,3]. Liver is the most frequently affected organ in majority of cases of echinococcal cysts, with a 4:1 liver:lung distribution [2,3,5-7]. Echinococcosis is usually associated with slow growth, although rapid growth does not exclude Echinococcosis [2].
Simple hepatic cysts are benign, common and typically revealed incidentally [8]. They are usually asymptomatic, do not impair liver function and despite very rare neoplastic degeneration, do not require surgical intervention [8-10].
The diagnostic methods in the evaluation of hepatic cysts include abdominal USG examination, CT and MRI scans [3,11]. Gold standard and the first line imaging modality in screening remains the ultrasound. The CT and MRI are the second line imaging dedicated for disseminated, complicated or extra abdominal cases, especially in preoperative evaluation [2,3,12]. For patients who claim non-specific epigastric pain or discomfort, the ultrasound examination may reveal simple, benign hepatic cyst [2]. When the detached endocysts are not present, it is difficult to distinguish non-parasitis from echinococcal cyst [12]. In presented case, the giant cyst with non-homogenous content was found during ultrasound examination. To evaluate the cyst and other abdominal organs, present patient underwent CT examination. The CT scans confirmed a giant cyst localised in the right lobe of the liver and revealed a single septa and non-homogenous content [Table/Fig-1a,b] . These findings as well as epigastric pain and a nonsignificant medical history led to suspicion of Echinococcosis and offering the patient a surgical management.
There are several treatment options for uncomplicated echinococcal hepatic cyst including wait-and-watch approach, chemotherapy with albendazole or mebendazole and various interventional management modalities [13,14]. The interventional modalities include percutaneous drainage or percutaneous ethanol sclerotherapy, endoscopic, laparoscopic or surgical approach [3,6,7,15,16]. Although, total pericystectomy has lower recurrence rate, the most frequent operative method remains capsectomy, drainage and epiploplasty [6]. For patient with giant hydatid cyst cysto-jejunostomy is considered to be a safer approach than partial cystectomy [11]. For the most serious cases with no other surgical or medical treatment option, the liver transplantation is also an acceptable treatment [4]. In the presented case, the patient who was referred with an epigastric pain had a giant, non-homogenous hepatic cyst with septa. Due to suspicion of Echinococcosis, the patient was offered surgery [Table/Fig-2]. The surgery was performed with a legitimate suspicion of parasitic origin of the giant cyst, yet the procedure included aspiration of the cyst content for the parasitological examination, irrigation with ethanol and subscapular cyst resection. The specimen was examined histopathologically, what revealed that the non-homogenous cyst content was caused by internal hemorrhage. The wall of the cyst was locally suppurated, what could be a reason of mentioned above intra-cystic hemorrhage, the increase of intra-cystic pressure and finally the pain in the epigastrium.
The cyst-related complications which may occur are rupture, intracystic hemorrhage or infection [5,9,15]. In presented case, a pathological examination revealed signs of suppuration in the cystic wall and a hematoma in a cyst’s content. The hepatic cyst may rupture into peritoneum, biliary tract, digestive tract, thorax, viscera or skin [8]. When the complications appear, the patient condition becomes serious [5,9,15]. Surgery should be done before the complications appear and remains the only and definitive treatment for symptomatic, complicated or large cysts exceeding 5 cm in diameter [3,8]. The epigastrial pain in presented case was suspected to be a sign of infection of cystic wall and intra-cystic hemorrhage, which are one of mentioned above cyst-related complications. Thus, referring the patient for surgery was the appropriate management option.
Conclusion
Although, benign liver cysts are common, rare Echinococcal cysts may also be revealed. The non-parasitic cysts localised in the liver may mimic the parasitic ones, especially when they are complicated with septa and non-homogenous content.
[1]. Mandal S, Mandal MD, Human cystic echinococcosis: epidemiologic, zoonotic, clinical, diagnostic and therapeutic aspectsAsian Pac J Trop Med 2012 5(4):253-60.10.1016/S1995-7645(12)60035-2 [Google Scholar] [CrossRef]
[2]. Valour F, Khenifer S, Della-Schiava F, Cotte E, Guibert B, Wallon M, Unusualgrowth rate during cystic echinococcosisParasitol Int 2014 63(2):275-77.10.1016/j.parint.2013.11.00624275211 [Google Scholar] [CrossRef] [PubMed]
[3]. Keong B, Wilkie B, Sutherland T, Fox A, Hepatic cystic echinococcosis inAustralia: an update on diagnosis and managementANZ J Surg 2018 88(1-2):26-31.10.1111/ans.1411729024292 [Google Scholar] [CrossRef] [PubMed]
[4]. Moray G, Shahbazov R, Sevmis S, Karakayali H, Torgay A, Arslan G, Livertransplantation in management of alveolar echinococcosis: two case reportsTransplant Proc 2009 41(7):2936-38.10.1016/j.transproceed.2009.07.02219765480 [Google Scholar] [CrossRef] [PubMed]
[5]. Stamatakos M, Kontzoglou K, Tsaknaki S, Sargeti C, Iannescu R, Safioleas C, Intrahepatic bile duct rupture of hydatid cyst: a severe complication for thepatientChirurgia (Bucur) 2007 102(3):257-62. [Google Scholar]
[6]. Voros D, Katsarelias D, Polymeneas G, Polydorou A, Pistiolis L, Kalovidouris A, Treatment of hydatid liver diseaseSurg Infect (Larchmt) 2007 8(6):621-27.10.1089/sur.2006.007018171123 [Google Scholar] [CrossRef] [PubMed]
[7]. Michalopoulos N, Laskou S, Papavramidis TS, Pliakos I, Kotidis E, Kesisoglou I, Rupture of right hepatic duct into hydatid cystJ Korean Med Sci 2012 27(8):953-56.10.3346/jkms.2012.27.8.95322876065 [Google Scholar] [CrossRef] [PubMed]
[8]. de Reuver P, van der Walt I, Albania M, Samra JS, Hugh TJ, Long-term outcomes and quality of life after surgical or conservative treatment of benign simple liver cystsSurg Endosc 2018 32(1):105-13.10.1007/s00464-017-5645-328639041 [Google Scholar] [CrossRef] [PubMed]
[9]. Mori E, Akai Y, Matsumoto T, Kawaratani H, Horii M, Iwano M, Hepatic cyst infection in a healthy older maleBMJ Case Rep 2012 :bcr042011413610.1136/bcr.04.2011.413622605693 [Google Scholar] [CrossRef] [PubMed]
[10]. Monteagudo M, Vidal G, Moreno M, Bella R, Díaz MJ, Colomer O, Squamous cell carcinoma and infection in a solitary hepatic cystEur J GastroenterolHepatol 1998 10(12):1051-53.10.1097/00042737-199812000-000129895053 [Google Scholar] [CrossRef] [PubMed]
[11]. Acar F, Sahin M, Alptekin H, Yılmaz H, Kafalı ME, Surgical treatment of giant liver hydatid cysts: comparison of cystojejunostomy and partial cystectomySurg Today 2014 44(11):2065-71.10.1007/s00595-014-0887-324664490 [Google Scholar] [CrossRef] [PubMed]
[12]. Grisolia A, Troìa G, Mariani G, Brunetti E, Filice C, A simple sonographic scoring system combined with routine serology is useful in differentiating parasitic from non-parasitic cysts of the liverJ Ultrasound 2009 12(2):75-79.10.1016/j.jus.2009.02.00423396670 [Google Scholar] [CrossRef] [PubMed]
[13]. Rinaldi F, De Silvestri A, Tamarozzi F, Cattaneo F, Lissandrin R, Brunetti E, Medical treatment versus "Watch and Wait" in the clinical management of CE3 bechinococcal cysts of the liverBMC Infect Dis 2014 14:49210.1186/1471-2334-14-49225204575 [Google Scholar] [CrossRef] [PubMed]
[14]. Benzimra J, Ronot M, Fuks D, Abdel-Rehim M, Sibert A, Farges O, Vilgrain V, Hepatic cysts treated with percutaneous ethanol sclerotherapy: time to extend the indications to haemorrhagic cysts and polycystic liver diseaseEur Radiol 2014 24(5):1030-38.10.1007/s00330-014-3117-x24563160 [Google Scholar] [CrossRef] [PubMed]
[15]. Zanen AL, van Tilburg AJ, Bleeding into a liver cyst can be treated conservativelyEur J Gastroenterol Hepatol 1995 7(1):91-93. [Google Scholar]
[16]. Pang Q, Jin H, Man Z, Wang Y, Yang S, Li Z, Radical versus conservative surgical treatment of liver hydatid cysts: a meta-analysisFront Med 2017 10.1007/s11684-017-0559-y29170917 [Google Scholar] [CrossRef] [PubMed]