Introduction
PCOS is a condition in which women experiences various physiological, genetic as well as environmental changes. It is a hormonal disorder causing enlarged ovaries with many small cysts. Globally, PCOS is affecting many women in their reproductive age in an inconstant manner and this variable prevalence of PCOS is been observed as 2-25% [1]. The wide range of ubiquity of PCOS is might be due to disparate presentation of symptoms, diagnostic standards. Onset of PCOS occurs at the early age in girls when they start menstruating [1]. PCOS includes wide spectrum of clinical symptoms which are mainly caused by androgens resulting in increased BMI in women. It is known to have a multi factorial origin like infertility, menstrual disorder, elevated insulin level, hyperandrogenemia associated with obesity, increased BMI, type 2 diabetes, heart disease, mood disorder, obstructed sleep apnoea, endometrial cancer, hypothyroidism, hyperprolactinemia, hyperlipidemia, anovulation, altered cognitive functions of the brain etc., [2].
The patients of PCOS are generally obese with Body Mass Index ranging from 25 to 29.9 kg/m2 which has direct effect on estradiol metabolism due to which there is a disturbance in the female reproductive cycle. Though estradiol is primarily a reproductive hormone but it has been shown to alter the neuronal excitability. The excitatory and inhibitory effect of neurons due to hormonal variation in PCOS patients possibly results in alteration in responses to various reactions [3].
Reaction to any stimulus is a voluntary response which is measures the speed of response of a person. Process of responding tostimuli involves stimulus processing, decision making, attention span and response programming [4].
From previous studies, it is apparent that reaction time is the depiction of the neural integrity. It has also been seen that visual reaction time is increased in luteal phase (due to progesterone) as compared to follicular phase (due to estradiol) where increased neuronal conduction was attributed to oestrogenic influence and thereby decreasing the reaction time [5].
Hence, these findings triggered this study, i.e., to find out the effect of the deranged hormone profile in PCOS, on the neuronal activity of women, which could be measured indirectly through the reaction time assessment, for which the auditory and visual reaction times were chosen. Thus, the present study was designed with an aim to evaluate the neuronal activity through auditory and visual reaction time in patients with Polycystic ovarian syndrome.
Materials and Methods
The present study was designed as a comparative case-control study, which was started only after obtaining ethical clearance from institutional ethical committee. The written consent was taken from the study participants. The cases were recruited from the fertility centre of Geetanjali Medical College and Hospital, Udaipur, Rajasthan, India, by random sampling. The data collection for the study took four months to get completed i.e., from March 2016 to July 2016.
The study was conducted on 80 women who were divided equally into two groups; PCOS and NPCOS. The sample size was calculated from the formula:
n=4pq/L2
where, p=10.32; (prevalence of PCOS calculated from a previous study), q=100-p=89.8; (with 10% permissible error, L); n=4×10.32×89.8/100=37.06, rounded off to 40, in each group [1,2].
The patients in Group PCOS included 40 healthy women with PCOS; Group NPCOS included 40 healthy women without PCOS, attending the infertility OPD and consented to participate in study. Both the groups were compared for various anthropometric and vital parameters and were matched for age, height, Body Mass Index (BMI), heart rate, blood pressure.
Patients were diagnosed according to AES criteria (2010); [1,6] which states that a woman is diagnosed as PCOS when all three of the following criteria are present:
Hyperandrogenism (clinical or biochemical)
Ovarian dysfunction (oligomenorrhoea or anovulation and/or polycystic ovarian morphology)
Exclusion of other androgen excess or related disorders
However, the subjects with any other systemic disease except PCOS were excluded from the study.
After a detailed physical examination, the anthropometric measurements were obtained of all the participants, viz. height, weight and BMI.
The blood samples (5 mL) was taken, from all the subjects for various biochemical parameters, viz., Random Blood Sugar (RBS), hormonal status (serum estradiol, serum prolactin, serum Anti Mullerian Hormone (AMH) and serum Thyroid Stimulating Hormone (TSH) and were measured using fully automated COBAS-6000 analyser based on principle of chemiluminiscence.
The audio-visual reaction time, of the participants from both the groups was measured using audio visual reaction time machine (RTM-608 and supplied by Medicaid Chandigarh). This instrument is equipped with a sensitive quartz clock which measured upto 1/10th of a msec with an accuracy of +1 and -1 digit. The audio-visual reaction time was measured in a quiet room of Fertility department of our hospital. Each session lasted for about 15 minutes. A practice session was given to the subjects before starting the test.
All the subjects used their dominant hand to press the switch to stop the quartz clock of the apparatus. Before measuring the visual reaction time, each subject was asked to respond to the alternating flashing of the red, green and yellow light. They were instructed to press the corresponding switch as soon as they see the light. This process was repeated for about nine times.
For measuring auditory reaction time, they were asked to respond a total of nine auditory stimuli of varied frequencies (250 Hz, 500 Hz and 750 Hz) by pressing the corresponding switch immediately to stop the sound.
All the readings for Auditory Reaction Time-Visual Reaction Time (ART-VRT) were recorded for the respective groups. Each auditory and visual stimulus was given thrice and the average of all these stimuli was recorded as mean ART/VRT.
Statistical Analysis
The data collected were analysed using unpaired t-test; and p-value <0.05 was considered as significant.
Results
[Table/Fig-1] shows that there is no significant difference in mean age, mean height, weight and BMI in both the groups. Also, the heart rate, blood pressure and random blood sugar level were comparable and showed no significant difference among both the groups.
Comparative values of various anthropometric and vital parameters in both the groups.
| Parameters | Group PCOS | Group NPCOS |
|---|
| Mean Age (years) | 27±5.24NS | 30.5±6.2 |
| Mean Height (cm) | 2.3±0.15NS | 2.4±0.16 |
| Mean Weight (kg) | 52.9±10.9NS | 55.2±10.4 |
| Mean Body Mass Index (kg/m2) | 22.2±5NS | 22.6±4.4 |
| Mean Heart Rate (beats/minute) | 82.5±15.7NS | 80.3±10.9 |
| Mean Systolic Blood Pressure (mm/Hg) | 109.1±14.8NS | 118±13.4 |
| Mean Dystolic Blood Pressure (mm/Hg) | 72.3±12.6NS | 78.5±10.10 |
| Mean Random Blood sugar (mmol/L) | 5.8±5.5NS | 5.5±1.3 |
NS-not significant as assessed by unpaired t-test
On the other hand, the hormone levels (mean serum AMH, mean serum prolactin, mean serum AMH and mean serum estradiol) were significantly (p<0.01) elevated in Group PCOS as compared to Group NPCOS. However, serum TSH was non-significantly lower in the test group [Table/Fig-2].
Mean values of AMH, Prolactin and TSH; mean value of Estradiol in both the groups.
| Parameters | Group PCOS | Group NPCOS |
|---|
| Serum AMH (ng/mL) | 5.20±1.36* | 1.54±1.19 |
| Serum Estradiol (pg/mL) | 21.09* | 5 |
| Serum Prolactin (ng/mL) | 19.23±9.9* | 14.15±6.57 |
| Serum TSH (μL/mL) | 3.03±2.3NS | 3.3±3.15 |
*p<0.01, highly significant; NS: Non Significant as assessed by unpaired t-test
These hormonal tests were done by collecting blood samples of the volunteers and were measured using COBAS-6000 analyser.
The ART for group PCOS was significantly lower (p=0.012) as compared to the other group whereas VRT was non-significantly lower in PCOS group [Table/Fig-3].
Mean ART and VRT in both the groups.
| Parameters | Group PCOS | Group NPCOS |
|---|
| ART (msec) | 1.18±0.4* | 1.38±0.36 |
| VRT (msec) | 0.86±0.26NS | 0.91±0.2 |
Discussion
The present study documents a significant decrease in auditory reaction time whereas non significant decrease in visual reaction time in patients with PCOS as compared to non PCOS. It was also observed that the decrease in ART was 14.49% and 5.49 % in VRT, for group PCOS when compared to group NPCOS. The decreased reaction time in group PCOS could be attributed to altered hormonal profile in the patients with PCOS.
As observed in [Table/Fig-2], the various hormones viz., serum estradiol, serum prolactin and serum AMH were significantly high in the study group (Group PCOS) indicating the interplay of these hormones in modulating the neuronal activity, hence affecting the reaction time. These hormones are documented to have varied effects on neuronal activity of brain [7].
Various environmental and genetic factors along with physical inactivity results in obesity and insulin resistance in PCOS, prevalently seen nowadays, hence stimulates the ovaries causing an increase in release of AMH. The AMH has been reported to have a stimulatory effect on Gonadotrophin releasing hormone neurons, located in hypothalamus, which secrete high amount of gonadal hormones (Luteinizing hormone and Follicle Stimulating Hormone) causing an increase in follicular growth and ovarian hyperandrogenemia resulting in PCOS [7,8]. As a result, PCOS causes hyperestrogenemia and hyperprolactinemia. The literature has clearly indicated the neuroexcitatory role of estradiol through ERα receptors [5]. The hyperprolactinemia, seen in PCOS may occur directly through hyper ovaries or indirectly through raised estradiol levels [9]. The studies have also reported that a high level of prolactin stimulates Tubero Infundibular Dopamine (TIDA) neurons through ultra short loop feedback mechanisms. Stimulation of TIDA neurons results in high Dopamine levels, which is also a neuromodulatory neurotransmitter [Table/Fig-4] [9]. Hyperprolactinemia has also been reported to result in natriuresis, diuresis and kaliuresis thus altering the fluid and electrolyte balance of the body [10]. This electrolyte imbalance may affect the membrane potential and hence neuronal activity [Table/Fig-5].
Excitatory effect of prolactin on TIDA neurons.
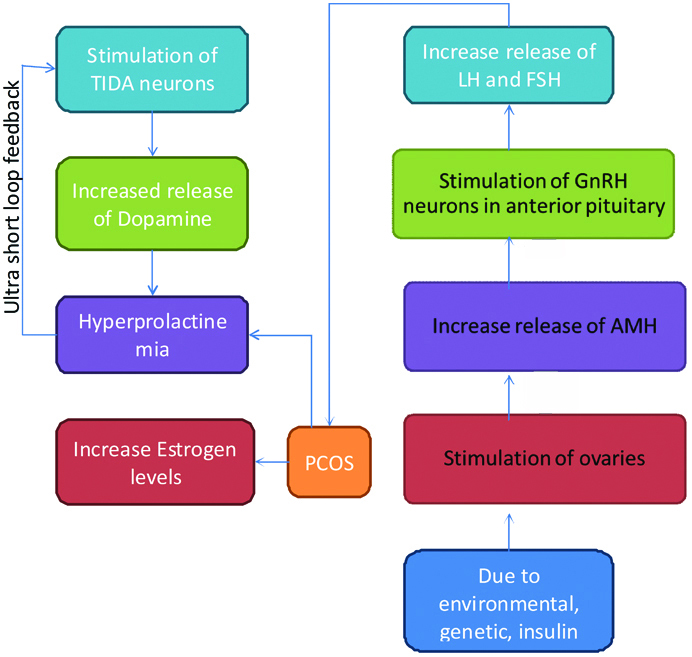
Hormonal variation in PCOS.
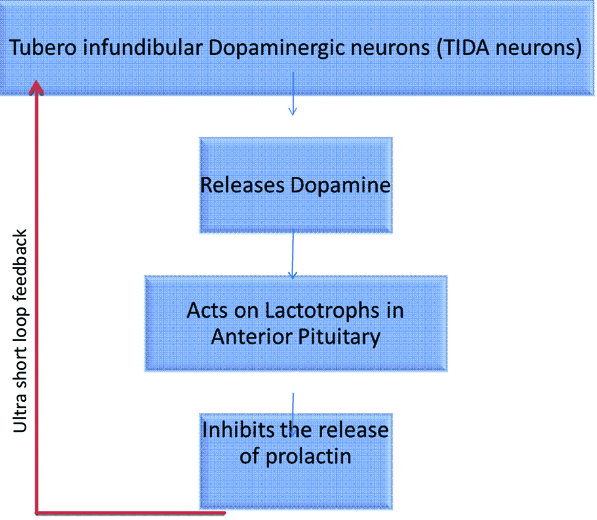
The altered hormonal profile, during pregnancy has also documented the increased reaction time, mainly attributed to progesterone [11]. The present study has also reported the significant hyperprolactinemia in Group PCOS, which might mediate its effects through Dopaminergic neurons on anterior pituitary gland. Levels of dopamine are found to influence various neuronal responses such as auditory responses, integration, attention, physiological state and neuronal disorders [12].
Another insignificant finding in both the groups was the normal levels of TSH, though the levels were in high normal range. The literature has documented a close association of sub clinical hypothyroidism with PCOS, which was not seen in this study [13]. As documented raised TSH level could prolong the reaction time but in this study the levels of TSH were normal. Hence, any effect of TSH on neurons could be ruled out.
Hence, the present study highlights the effect of altered hormonal profile (estradiol, prolactin and AMH) in patients of POS on the neuronal activity by increasing their excitability and lowering their reaction time.
Limitation
The present study came across a wide variation in the serum estradiol levels with the range of (2 pg/mL-3000 pg/mL), which resulted in the skewed data and hence we calculated the mode for serum estradiol rather than the mean, which showed us wide fluctuations in the serum estradiol levels.
Conclusion
The neuronal activity is slightly increased in the patients with Polycystic Ovarian disease which is quite evident due to decreased reaction time.
This increased neuronal activity could be attributed to hyperestrogenemia which acts through ERα receptors and is a documented neuroexcitatory hormone along with the stimulation of Tubero infundibular neurons in hypothalamus due to hyperprolactinemia resulting in increased dopamine levels in these patients, further adding to neuro-modulatory effect of oestrogen.
NS-not significant as assessed by unpaired t-test
*p<0.01, highly significant; NS: Non Significant as assessed by unpaired t-testThese hormonal tests were done by collecting blood samples of the volunteers and were measured using COBAS-6000 analyser.
[1]. Joshi B, Mukherjee S, Patil A, Purandare A, Purandare A, Chauhan S, A cross-sectional study of polycystic ovarian syndrome among adolescent and young girls in Mumbai, IndiaIndian J Endocrinal Metab 2014 18(3):317-24.10.4103/2230-8210.13116224944925 [Google Scholar] [CrossRef] [PubMed]
[2]. Malik S, Jain K, Talwar P, Prasad S, Dhorepatil B, Devi G, Management of Polycystic Ovarian Syndrome in IndiaFertility Science and Research 2014 1(1):23-43. [Google Scholar]
[3]. Reese ME, Casey E, Musculoskeletal health in pregnancy and postpartum. Switzerland, Musculoskeletal Health in Pregnancy system in Pregnancy Springer International Publishing 2015 :19-39.10.1007/978-3-319-14319-4_2 [Google Scholar] [CrossRef]
[4]. Garg R, Malhotra V, Dhar U, Tripathi Y, Study of visual reaction time in different phases of menstrual cycleInt J Cur Res Rev 2014 6(17):41-43. [Google Scholar]
[5]. Markou A, Duka T, Prelevic GM, Estrogens and brain functionHormones (Athens) 2005 4(1):09-17.10.14310/horm.2002.11138 [Google Scholar] [CrossRef]
[6]. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop GroupRevised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndromeFertil steril 2004 81:19-25.10.1016/j.fertnstert.2003.10.004 [Google Scholar] [CrossRef]
[7]. Cimino I, Casoni F, Liu X, Messina A, Parkash J, Jamin SP, Novel role for anti-Mullerian hormone in the regulation of GnRH neuron excitability and hormone secretionNat commun 2016 7:1005510.1038/ncomms1005526753790 [Google Scholar] [CrossRef] [PubMed]
[8]. Kermath BA, Gore AC, Neuroendocrine control of the transition to reproductive senescence: lessons learned from the female rodent modelNeuroendocrinology 2012 96:01-12.10.1159/00033599422354218 [Google Scholar] [CrossRef] [PubMed]
[9]. Gittelman JX, Perkel DJ, Portfors CV, Dopamine modulates auditory responses in the inferior colliculus in a heterogeneous mannerJ Assc Res Otolaryngol 2013 14:719-29.10.1007/s10162-013-0405-023835945 [Google Scholar] [CrossRef] [PubMed]
[10]. Ibarra F, Crambert S, Eklof A, Lunquist A, Hansell P, Holtbäck U, Prolactin, a natriuretic hormone, interacting with the renal dopamine systemKidney Int 2005 5:1700-07.10.1111/j.1523-1755.2005.00586.x16164646 [Google Scholar] [CrossRef] [PubMed]
[11]. Mehta R, Kurmi N, Kaur M, Verma A, Effect of pregnancy on the auditory and visual reaction timeInternational Journal of Research in Medical sciences 2017 5(2):525-28.10.18203/2320-6012.ijrms20170144 [Google Scholar] [CrossRef]
[12]. Cave BJ, Wakerley JB, Luckman SM, Tortonese DJ, Hypothalamic targets for prolactin: assessment of c-Fos induction in tyrosine hydroxylase- and proopiomelanocortin-containing neurones in the rat arcuate nucleus following acute central prolactin administrationNeuroendocrinology 2001 74:386-95.10.1159/00005470511752895 [Google Scholar] [CrossRef] [PubMed]
[13]. Azziz R, Woods KS, Renya R, Key TJ, Knochenhauer ES, Yildiz BO, The prevelance and features of the polycystic ovary syndrome in an unselected populationJ Clin Endocrinol Metab 2004 89(6):2745-49.10.1210/jc.2003-03204615181052 [Google Scholar] [CrossRef] [PubMed]