Among eight HPV genes, two early genes i.e., E6 and E7 plays key role in tumor formation [5] i.e., both E6 and E7 genes interacts with the tumor suppressor genes i.e., p53 and hypophosphorylated Rb respectively [6]. These early oncogenes are invariably expressed in human cervical cancer, and their continued expression is required for maintenance of the cancerous state [7].
According to literature the sexual activity plays most important role in the acquisition of HPV infection therefore higher number of sexual partners increases the risk of HPV infection. Other risk factors includes infection with Herpes simplex virus and Chlamydia, impaired immune response, persistence of virus (HPV), smoking, extensive use of oral contraceptives and administration of steroid hormones [8,9]. The thorough understanding of the risk factors of this infection is required because this information will be helpful in implementation of future prevention strategies [8].
Cervical cancer can be prevented by early detection of abnormalities and subsequent treatment, it is important to establish cost-effective, sensitive, and accurate screening protocols within routine clinical practice [10]. Pap test is the standard method used for the screening of cervical cancer in India; however, organized screening programs are rare. Despite the availability of Pap testing, the incidence of invasive cervical cancer remains high, especially in rural India [11]. Though HPV vaccines have been launched recently; they prevent infection by the major types of HPV only. However, cervical cancer may be caused by other genotypes of this virus as well. Hence we still need to rely on early detection of infection by screening methods and moreover there is no literature available regarding the circulating genotypes of HPV among women of our locality. Therefore, the present study has been planned to screen the women attending OBG OPD in our tertiary care hospital, with any gynaecological problem, for the presence of HPV- DNA, so as to understand the circulating genotypes of HPV among these patients.
Materials and Methods
For this prospective study total 90 subjects were enrolled after obtaining ethical clearance from institutional ethics committee. The sample size was calculated using the “G-Power Software, version 3.1.9.2” with the effective size of 10%. This study was conducted for a period of 11 months i.e., from November 2016 to September 2017. Data and sample collection were done at the Department of OBG and sample processing was done at the Department of Microbiology, Yenepoya Medical College, Mangalore. Informed consent was obtained from all the enrolled participants.
Inclusion criteria: All subjects who were married, non pregnant and had not undergone hysterectomy were included.
Exclusion criteria: Women who were pregnant, unmarried and refused to sign the consent were excluded.
Data collection: Cervical biopsies were collected from 50 subjects those who were admitted in OBG ward with cervical abnormalities and cytobrush samples were collected from 40 subjects who came to OBG OPD and suspected to have HPV infection. Cytobrush samples were taken from the patients before Pap smear sampling during the routine examination.
Following the cervical punch biopsy, a small piece of tissue was sent for histopathology and another piece was stored in phosphate buffer saline at 2-4°C until DNA extraction for PCR. Cytobrush samples were collected using a Qiagen, Digene HC2 DNA collection device, Germany; which was after collection placed into Qiagen STM collection medium provided with the same collection kit and stored at - 20°C until DNA extraction, not more than four weeks.
Questionnaire based assessment of risk factors and awareness regarding HPV and HPV mediated malignancy: To evaluate different aspects of knowledge and awareness of HPV and HPV mediated malignancy, all the subjects were offered a structured questionnaire from an existing interview guide from a previous study [Table/Fig-1] [12]. All subjects answered the questionnaire voluntarily and independently. Descriptive analysis was performed on the information collected using Microsoft Excel.
Questionnaire used for the assessment of Knowledge about HPV and HPV mediated malignancy.
| Major issue | Topic Question |
|---|
| Awareness and knowledge of Cervical Cancer | What do you know about cervical cancer? |
| What causes cervical cancer? |
| Who can have cervical cancer? |
| Do you think there is a possibility your daughter may have cervical cancer in the future? Why? Why not? |
| Do you know the risk factors of cervical cancer? |
| Have you ever had cervical Pap smear test done? |
| Awareness and knowledge of HPV and HPV vaccine | Have you heard about the human papillomavirus (HPV)? |
| Where did you hear about it? |
| Who could get HPV? |
| Have you heard about the HPV vaccine? |
| Have you ever had an HPV test before? |
DNA Extraction: The tissues were cut into approximately 25 mg pieces (not more than 25 mg) and chopped into fine pieces before starting the procedure for DNA extraction. DNA was extracted from cervical tissues and from the material collected by the cytobrushes using Qiagen DNA Mini kit (Qiagen GmbH, Hilden/Germany) according to kit literature and stored at -70°C until performing PCR for HPV DNA detection. In addition, DNA was extracted from a HPV negative endometrial tissue (negative control) and from a cervical cancer tissue sample which was positive for HPV (positive control) for this study. Both the samples were obtained from the patients who were admitted in our hospital during standardisation of the PCR.
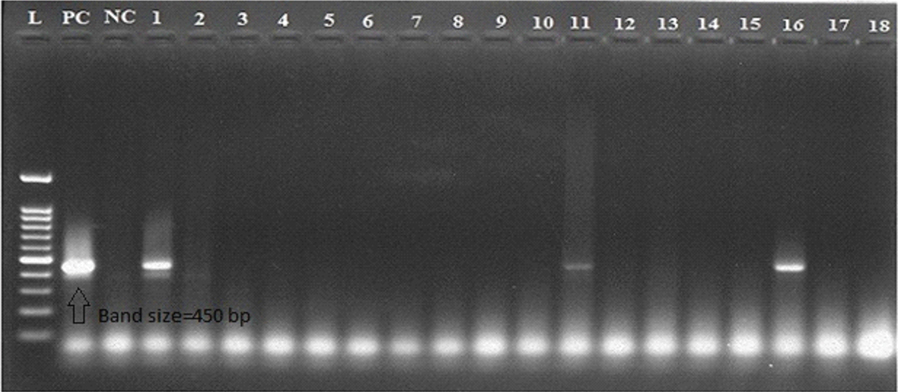
HPV detection by Polymerase Chain Reaction (PCR): DNA from each sample was amplified by PCR with the primer sets as given in [Table/Fig-2]. The oligonucleotide primers were procured from the EUROFINS Genomics Private India Limited, Bangalore. PCR was performed using the in-house PCR protocol in thermal cycler (applied biosystems, USA) that is routinely followed in our laboratory. A 25 μL reaction was assembled that contained 3 μL sample DNA, 12.5 μL Ampliqon Red 2X Mastermix (Tris-HCL pH 8.5, Ammonium sulphate (NH4)2SO4, 0.2 unit/ μL ampliqon Taq DNA polymerase, 0.4 mM deoxynucleotide triphosphate (dNTPs), 3 mM MgCl2, 0.2% Tween 20), 1 μL of 10 pmol of each primers (forward and reverse) and 7.5 μL molecular grade water. The PCR condition [13] for each primer set is given in [Table/Fig-3]. The amplified products were analyzed on a 2% agarose gel, stained with ethidium bromide (0.5 μL/ ml) and visualized on a UV transilluminator and photos of the bands were recorded using gel documentation system (Major science, USA) as shown [Table/Fig-4]. The amplification was carried out in the presence of negative and positive controls; DNA from cervical cancer tissue sample positive for HPV was used as a positive control and a HPV negative endometrial tissue used as a negative control.
Primers used for detection of common Human papillomavirus (6, 11, 16, 18, 31 and 33).
| Primer | Sequence | Target | Band size (bp) |
|---|
| MY09MY11 | F5’-CGTCCMARRGGAWACTGATC-3’R5’-GCMCAGGGWCATAAYAATGG-3’ | L1 | 450 |
F-Forward, R-Rverse, bp-Base pair
Polymerase chain reaction (PCR) conditions for primer sets.
| Primer Name | Hot Start | Denaturation | Annealing | Extension | Final Extension |
|---|
| 40 cycles |
|---|
| MY09/MY11 | 95 °C, 5 min | 94 °C, 1 min | 55 °C, 1 min | 72 °C, 30 s | 72 °C, 5 min |
Agarose gel showing polymerase chain reaction on amplified product of HPV (6, 11, 16, 18, 31 and 33) common gene.
L - 100 base pair (bp) DNA ladder (NEX-GEN, GENETICS), PC - Positive control (band size=450 bp), NC - Negative control, 1 and 16 - Strong positive, 11 - Weekly positive and 2-10, 12-15, 17, 18 – Negative for HPV
Statistical Analysis
The statistical analysis was performed using the Windows program; SPSS (version 22.0). Chi square test was used and variables were compared between HPV positivity and histopathological/cytological status of the patients. p-value less than 0.05 was considered significant. Positive predictive value and negative predictive value was calculated wherever appropriate with the help of EPR-Val Test Pack 2 Web browser version.
Results
Total 90 subjects were enrolled in the present study. A complete demographic data were collected from all the participants as shown in [Table/Fig-5]. Out of 90 cervical samples, 50 were tissue biopsies and 40 were cytobrushes.
Socio-demographic details of the participants.
| Socio-demographic factors | n = 90 | % | H PV DNA + |
|---|
| Age group (Years)20-3030-4040-5050-60> 60 | 92536146 | 1027.84015.56.7 | 0202050503 |
| ReligionHinduMuslimChristian | 58302 | 64.533.32.2 | 100700 |
| Socioeconomic statusBelow poverty lineAbove poverty line | 6624 | 73.326.7 | 1304 |
| LiteracyEducatedUneducated | 5931 | 65.634.4 | 1106 |
Among 50 tissue biopsies, 15 had different types of cervical carcinoma (seven Non Keratinizing Squamous Cell Carcinoma, three Keratinizing Squamous Cell Carcinoma, two Adenocarcinoma and three Moderately Differentiating Squamous Cell Carcinoma) whereas two had Cervical Intraepithelial Neoplasia-II and 33 had chronic cervicitis. Among 40 cytobrush samples, PAP smear cytology shows 32 were Negative for Intraepithelial Lesions/Malignancy, two had ASCUS, three had Inflammatory Smear with Reactive Atypia and three had Inflammatory smear as shown in [Table/Fig-6].
HPV-DNA prevalence in women with different cervical abnormalities.
| Histology/Cytology of samples | Number of sample (n=90) | HPV DNA positive |
|---|
| Invasive Cervical CancersNKSCCKSCCAdenocarcinomaMDSCC | 7323 | 3421- |
| CIN – II | 2 | 2 |
| Chronic Cervicitis | 33 | 2 |
| NILM | 32 | 3 |
| ASCUS | 2 | 1 |
| IS-RA | 3 | 1 |
| Inflammatory smear | 3 | 1 |
| TOTAL | 90 | 17 (18.8 %) |
NKSCC-Non Keratinizing Squamous Cell Carcinoma, KSCC-Keratinizing Squamous Cell Carcinoma, MDSCC-Moderately Differentiating Squamous Cell Carcinoma, CIN-II-Cervical Intraepithelial Neoplasia-II, NILM-Negative for Intraepithelial Lesion/Malignancy, ASCUS- Atypical Squamous Cells of Undetermined Significance, IS-RA-Inflammatory Smear with Reactive Atypia
PCR results confirmed 11/50 (22%; p-value = 0.0004) HPV positives among tissue biopsies whereas only 6/40 (15%; p-value = 0.08) HPV positives among cytobrush sample. The distribution of HPV DNA positive samples among study participants is shown in [Table/Fig-5,6]. The occurrence of HPV in present study among invasive carcinomas was high i.e., 7/15 as compared to women with chronic cervicitis (2/33), NILM (3/32), ASCUS (1/2), IS-RA (1/3) and Inflammatory smear (1/3) (χ2 = 16.1173; p-value = 0.002866). The prevalence of HPV infection in the present study is low i.e., only 18.8%.
The histopathological/cytological positive/negative results were compared with the PCR positive/negative results of both the biopsy and cytobrush samples. The positive and negative predictive values for HPV DNA from 17/50 histopathologically positive and 33/50 histopathologically negative tissue biopsies were evaluated. Similarly, the positive and negative predictive values for HPV DNA from 8/40 cytologically (PAP smear) positive and 32/40 cytologically negative cytobrush samples were evaluated as given in [Table/Fig-7].
Comparison of histopathological/cytological findings of tissue biopsies and cytobrush samples with PCR findings.
| Total samples (n=90) | PCR positive samples | PCR negative samples | Positive predictive value | Negative predictive value | p-value |
|---|
| Histological positive biopsy samples (n=17) | 09 | 08 | 53% | 94% | 0.0004 |
| Histological negative biopsy samples (n=33) | 02 | 31 |
| Cytological positive cytobrush samples (n=08) | 03 | 05 | 37.5% | 90.6% | 0.08 |
| Cytological negative cytobrush samples (n=32) | 03 | 29 |
Assessment of Risk Factors for the Acquision of HPV Infection: Patient information sheet; approved by the institutional ethics committee was provided to all the participants at the beginning of the study. With regard to age at marriage 58/90 (64.4%) had sexual debut before or at the age of 20 years however, 32/90 (35.6%) got married after the age of 21 or above. 48/90 (53.3%) women had more than three children in which some of them had even 8-10 children. Only 2/90 (2.2 %) subjects had been using oral contraceptive during last two years before participating in the present study. With regard of sexual partner, 87/90 (96.7%) were monogamous and only 3/90 (3.3%) had two or more than two partners. Upon assessment of questionnaire, it was observed in this study that even though literacy rate being 65.5%, 84/90 (93.3%) women are not aware of PAP smear screening for cervical cancer and therefore never had gone for PAP testing. Majority of women 62/90 (68.9%) used cotton cloth during menstruation whereas 28/90 (31.1%) women used sanitary pads. A 75/90 (83.3%) participants were free from any underlying conditions however, 15/90 (16.7%) participants had some underlying conditions like hypertension, diabetes etc.
Discussion
In India, annually the incidence of cervical cancer is quite high [2] therefore, early screening of HPV and cervical cancer can be a better solution for this question. The major obstacles in India and in other developing countries for the low screening prevalence are either educational barriers or behavioral barriers [14]. Persistent high risk HPV infection increases the risk of cervical intraepithelial neoplasia or invasive cervical cancers. The distribution of HPV varies geographically however, HPV 16 found to be the commonest type followed by HPV 18 [15].
In the present study, 36/90 (40%) of the participants belonged to the 40-50 years age group followed by 25/90 (27.8%) in 30-40 years age group whereas, a study from China had maximum number of participants in the age group of 31-40 years [16]. However, study done by Vince A et al., reported maximum number of subjects from the age group (20-40 years) which was not in accordance to the present study [4]. Age specific prevalence was increased from 2.2% to 5.5% from age group 20-40 to 40-60 years, then again decreases to 3.3% from age group >60 years onwards. However, a population based survey from Bangladesh reported that the age specific prevalence was first decreased for 25-34 age group then increased for 35-44 age group and again decreased for age group above 45 years [17].
The occurrence of HPV in present study among invasive carcinomas was found to be high, being 46.7% as compared to women with chronic cervicitis and NILM being only 6.3% and 9.4%, respectively which is in accordance with a study from Pakistan [10]. In present study, the results of histopathological positive/negative and PCR positive/negative tissue biopsy samples were significantly correlated (p-value 0.0004) whereas; results of cytological positive/negative and PCR positive/negative for cytobrush samples were not significantly correlated (p-value 0.08). However, the overall prevalence of HPV in present study was low (18.8%), which is in accordance with a study from Bangladesh [17] in which the reported overall prevalence was 7.7% only. However, a study by Chakravarty J et al., from East India reported the overall prevalence of HPV among HIV positive subjects was 26.85% which according to the author was the high prevalence as compared to the general population [18]. However, results from western countries were contradictory to the present study where HPV prevalence was found to be high [19,20].
Results of the present study showed that 66/90 (73.3%) of the study participants belonged to the below poverty line status (which was considered on the basis of having a ration card), yet most of them were educated whereas, education rate among population from the North India was found to be low [21]. After the assessment of the questionnaire given to the study participants it was analysed that even though being educated (literate and illiterate subjects were classified according to the Arora CD et al., [22]) more than 90% of the women in Mangalore region are not aware of HPV infection or HPV mediated malignancies. However, according to Ganju SA et al. the awareness regarding cervical cancer from India, Nepal and Sri Lanka was found to be 66%, 58.8% and 57.7%, respectively [14].
PAP smear is a simple, cost-effective and sensitive tool for the detection of premalignant and malignant changes in the cervix. The efficiency, sensitivity and specificity of the Pap smear depends on frequency of cervical cancer screening programs for women, adequate sample collection, and the quality of laboratory analysis [23].
A study published from north India in accordance with the present study which reported that the PAP smear had sensitivity of 80% with the positive predictive value of 48.98% and negative predictive value of 88.24% [24]. As it is well known that infection with HPV in cervix is reversible so this could be the reason for the discordance between cytology and molecular detection may also be influenced by self-clearance of the virus during the interval between PAP test and molecular assay [10].
Although vaccines are available for two major high risk oncogenic HPVs and two low risk oncogenic HPVs i.e., type 16/18 and type 6/11 respectively, the major problem in vaccinating women in developing countries is the lack of knowledge or awareness and the high cost of vaccination [25]. However, a study from North India by Hussain S et al., on the willingness of HPV vaccination after educating students about the risks of HPV infection and consequences related to this virus, it was found that the willingness was 70% among females compared to males and 64% among urban populations compared to rural populations [26].
Limitation
Present study mainly focused on those HPV types which are most commonly considered as highly oncogenic, however in the recent past years some low risk oncogenic types have been emerged as a causative agent of cervical cancers. Additionally, the major drawback is that as this is a cross-sectional study and no longitudinal data is available, therefore, major conclusions cannot be drawn about causality as mere presence of HPV does not mean that patient will die of cervical cancer because in many cases the abnormal cervical cell may returns to the normal state by the auto clearance of HPV from the body as a result of immune response.
Conclusion
In Mangalore region, the prevalence of HPV is very low and there is absolute no awareness regarding HPV infection. Many epidemiological studies suggest that regular cervical screening in adult females is important in the reduction of HPV associated cervical malignancy. Though HPV vaccines have been launched recently; they prevent infection by the major types of HPV only. However, cervical cancer may be caused by other genotypes of this virus as well. Hence, we still need to rely on early detection methods. Therefore, molecular testing for HPV infection should additionally be used in order to identify patients who are at high risk for the development of premalignant lesions. Combination of cytology and molecular testing may help to avoid unnecessary stress and intensive follow-ups. Overall, these findings could have important implications for the preventions of cervical cancer.
F-Forward, R-Rverse, bp-Base pair
NKSCC-Non Keratinizing Squamous Cell Carcinoma, KSCC-Keratinizing Squamous Cell Carcinoma, MDSCC-Moderately Differentiating Squamous Cell Carcinoma, CIN-II-Cervical Intraepithelial Neoplasia-II, NILM-Negative for Intraepithelial Lesion/Malignancy, ASCUS- Atypical Squamous Cells of Undetermined Significance, IS-RA-Inflammatory Smear with Reactive Atypia