Introduction
Microbes such as Chlamydia pneumoniae play an important role in development of atherosclerosis. The bacterium invades vessels walls, directly or indirectly, and by releasing endotoxins or lipopolysaccharides into the bloodstream leads to injuries to endothelial cells.
Aim
To determine the prevalence of C. pneumoniae in atherosclerotic plaques of corpses, by PCR (Polymerase Chain Reaction) and to examine the correlation between clinical status and presence of this bacterium in Iran.
Materials and Methods
In this descriptive comparative study, a total of 118 samples, including 59 from corpses with atherosclerotic plaques in arteries (44 coronary and 15 abdominal aorta samples) and 59 from corpses without atherosclerotic plaques or obstruct in arteries (44 coronary and 15 abdominal aorta samples) were refrigerated at -70°C. Then, DNA was extracted and to detect C. pneumoniae, the pstI gene was selected and after amplification, samples were electrophoresed to confirm the presence of expected PCR products. The data were analysed using Chi-square statistical test and p-value less than 0.05 was considered to be statistically significant. Also, the relation between C. pneumoniae and some variables of atherosclerotic diseases such as hypertension, hyperlipidemia, smoking and diabetes were studied.
Results
In this study, 15% (9/59) of samples from corpses with atherosclerotic plaque were positive for C. pneumoniae DNA, 11% (7/59) in coronary arteries and 4% (2/59) in aortic wall layer while, there was no evidence of C. pneumoniae in corpses with no plaque or obstruction in arteries. Variables such as hypertension, hyperlipidemia and myocardial infarction had higher values in C. pneumoniae positive samples; however, there was no statistically significant difference (p> 0.52).
Conclusion
Presence of C. pneumoniae in atherosclerotic plaques and absence in healthy vessels, confirm the possible role of C. pneumoniae in development of atherosclerosis, especially in regions with frequent infections. Nevertheless, the exact mechanism explaining the high prevalence of atherosclerotic vascular disease is completely unknown.
Introduction
Cardiovascular diseases are the most common cause of mortality in developed countries which lead to nearly one million deaths per year in USA. Multiple factors cause atherosclerosis, including smoking, hypertension, diabetes, obesity, hyperlipidemia, stress, depression, decreased physical activity, infection, etc., [1].
Despite the importance of blood lipids, nearly half of myocardial infarctions occur among people with no evident hyperlipidemia. Recently, there has been a lot of evidence on the role of infection in development of atherosclerosis, although it has not been confirmed yet [1]. Bacteria like C. pneumoniae and viruses such as cytomegalovirus, have been mentioned as factors that have a role in development of atherosclerosis [1].
C. pneumoniae (subspecies Taiwan Acute respiratory agent, TWAR), with human being as its sole known host, causes respiratory disease and just one serologic type of it is identified. Its infection is common and between 30 to 50 percent of world population have antibodies against it [2].
Serologic studies have revealed evidences of the relation between C. pneumoniae and atherosclerosis of coronary, cerebral and peripheral vessels [2].
It should be mentioned that in most cases C. pneumoniae was not considered as the cause of respiratory infection in most cases [2], and since common treatments of other respiratory infections are not effective against these bacteria, they can remain in patients body and act as a risk factor of atherogenesis [3,4].
Systemic responses to infection such as cytokines release, may change lipids profile and predispose the vascular condition to coagulation and lead to formation of thrombus or atherosclerotic plaques [4].
Given the fact that C. pneumoniae has direct effects on vessels wall and grows within the endothelial cell of the vessels, in addition to its direct effect on preparation of macrophages to absorb the oxidized Low-Density Lipoprotein Cholesterol (LDL-C) as the first stage of atherogenesis, detecting atherogenesis in patient with no common risk factor along with presence of C. pneumoniae can be assumed to be the result of the above-mentioned effects of C. pneumoniae. Hence, it is possible that presence of C. pneumoniae along with oxidizing agents and oxidation, is more important than increased cholesterol level [3].
The aim of the present study was to detect the genomic DNA of C. pneumoniae in atherosclerotic plaques of the corpses referred to Legal Medicine Center of Tehran, and studying other important risk factors in both groups of corpses.
Materials and Methods
This descriptive comparative study included 59 corpses with atherosclerotic plaques (44 coronary arteries and 15 abdominal aortas) referred to Iranian Legal Medicine Organization, Tehran between March 2016 to May 2016 as the case group and 59 corpses with no atherosclerotic plaques (44 coronary arteries and 15 abdominal aortas) as the control group. A simple random sampling method was used and each corpse was chosen entirely by chance. The number of samples (118 samples) was calculated according to other similar study as the maximum possible number [4]. To calculate the sample size for each control and patient group, the following formula was calculated.
According to previous studies, the frequency of C. pneumoniae bacteria in atherosclerotic plaques is 12% and it is 0% in healthy individuals [4-6]. With a confidence level of 95% and an 80% probability test, the sample size was calculated to be 61 in each group. Based on the bias in the implementation section of the project, a total of 59 people were sampled in each group.
All coronary arteries and abdominal aortas were kept in -70°C to be studied later. The diameter of the abdominal aorta was measured and demographic data, lipid profile, history of smoking and hospital record of each person was documented. The study was approved by the research ethics committee of the Iranian Legal Medicine Organization (LMO).
Inclusion criteria for the case group, included patients more than 30-year-old, at least one atherosclerotic plaque in cardiac vessels.
Exclusion criteria for the case group, were patients affected with hepatic, gastric renal and autoimmune diseases, as well as cancer. Inclusion criteria for the control group consisted of more than 30-year-old and absence of atherosclerotic plaques in cardiac vessels. Tissue sample (Coronary arteries and abdominal aortas) were taken under sterile conditions in the autopsy at the Legal Medicine Center of Tehran. A 4-5 millimeter section of the vessel was longitudinally incised and then put in a microtube containing Tris EDTA buffer (buffer containing 10 mM Tris and 1 mM EDTA (TE buffer; Sigma). Following the transfer of microtubes from the autopsy to the microbiology lab, the samples were taken out under a hood with clean air stream to extract DNA.
DNA was extracted using the DNA purification Kit QiAamp DNA mini Kit (Qiagen, Hilden, Germany). Purity of the extracted DNA was measured using a NanoDrop™ spectrophotometer (NanoDrop ND-1000; Thermo Fisher Scientific, Waltham, MA). DNA samples with an OD260/OD280 ratio of ≥1.8 were used for further analysis. Moreover, the quality of extracted DNA was examined by 1% agarose gel electrophoresis (Sigma Chemical Co.).
In order to avoid contamination of samples, all stages of the procedure (preparation, PCR and analysis) were carried out in a separate room and under sterile conditions. To detect C. pneumoniae the pstI gene with 437 bp was selected and primers were taken according to the description in the study by Dabiri H et al., HL1 as Forward (5-GTTGTTCATGAAGGCCTACT-3) and HR1 as Revers (5-TGCATAACCTACGGTGTGTT-3) primers were used for amplification [4].
Amplification reactions were carried out in a total volume of 25 μL, containing 1 μL of DNA template, 2.5 μL of 10x reaction buffer, 1 μL of dNTPs (10mM), 1μL of MgCl2 (50mM), 1μL of each primer (10pmol) and 1U Taq DNA polymerase (Fermentas, Lithuania). The PCR conditions were as follows: an initial denaturation at 94°C for 5 minute, followed by 30 cycles, each consisting of denaturation at 94°C for one minute; annealing at specific 61°C for one minute; and elongation at 72°C for one minute and a final extension step at 72°C for five minute.
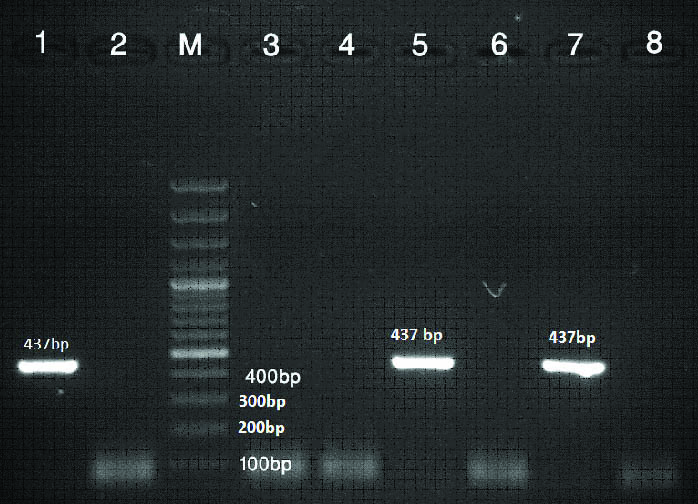
After amplification, 5 μL sample of each reaction was electrophoresed on a 1.5% agarose gel to confirm the presence of expected PCR products. Moreover, staining with Ethidium bromide was done and banding patterns were visualized and photographed using a GelDoc system (UVP, Upland, Calif.) under UV fluorescence. A 100-bp and 1kb DNA ladders (Fermentas, Lithuania), as a size standard, were used for band-size comparison of the PCR products [Table/Fig-1]. All amplification procedures were performed in duplicate.
PCR of C. pneumoniae in atherosclerotic plaques. 5 and 7 lanes: Positive samples. 3, 4, 6 and 8 lanes: Negative samples. M: 100 bp DNA Ladder (MW). Lane 1: Positive control (437bp), lane 2: Negative control.
Positive control (Chlamydophila pneumoniae ATCC® VR-1360™) was taken from the microbial collection bank, Pasteur Institute of Iran and Double-distilled water (DDW) samples were also used as a negative control for all reactions.
Statistical Analysis
Statistical analysis was performed using SPSS software version 19.0 for windows (IBM, Chicago, USA). Chi-square was used to compare proportions. The p-values less than 0.05 were considered to be statistically significant. Also, the relation between this bacteria and a number of risk factors of atherosclerotic disease, such as blood hypertension, hyperlipidemia and diabetes was studied. These risk factors were extracted from hospital files corpses referred to Iranian Legal Medicine Organisation.
Results
In the present study by PCR method 15% (9/59) of samples taken from plaques were positive for C. pneumoniae DNA, 11% (7/59) of which were in coronary arteries and 4% (2/59) in aortic samples.
Demographic data: The case group members consisted of 42 (71.2%) men and 17 (28.8%) women with the age range of 43-75 years and the mean age of 64.5±15 years. The mean anterior-posterior diameter of the abdominal aorta in the first group was 7.25±1 cm. The control group members (with no atherosclerotic plaque) included 45 (76.2%) men and 17 (23.8%) women with the age range of 41-78 years and mean age of 66.5±10 years. The mean anterior-posterior diameter of the abdominal aorta was 7.95±1 cm in this group. There was no significant difference in altering factors of age, sex and the maximum diameter of the abdominal aorta between the two groups (p-value=0.11).
There was no statistically significant difference between the two groups in terms of history of specific diseases such as blood hypertension, hyperlipidemia, smoking and diabetes (p-value=0.52) [Table/Fig-2]. The samples were examined to detect C. pneumoniae by PCR and the results of calculating significant difference between the two groups are shown in [Table/Fig-3] (p-value <0.001).
The relationship between the risk factors and atherosclerotic plaques in the two studied groups.
| Risk Factor | corpses with atherosclerotic plaques | corpses without atherosclerotic plaques | p-value |
|---|
| Blood Hypertension | 21 (35%) | 17 (28%) | 0.58 |
| Hyperlipidemia | 23 (38%) | 21 (35%) | 0.72 |
| Smoking | 20 (33%) | 18 (30%) | 0.36 |
| Diabetes | 12 (20%) | 10 (16%) | 0.37 |
p-value by Two-tailed Fisher’s exact test is significant at p<0.05
The results of the calculated significant difference between the two groups.
| Groups | PCR Positive (%) | PCR Negative (%) |
|---|
| Case | 15.5 | 84.5 |
| Control | 0 | 100 |
| Chi-square (df=1) | p-value <0.001 | |
Significant level: p<0.05
Discussion
The relationship between C. pneumoniae and atherosclerosis plaques was first reported by Saikku P et al., [7]. While these studies could not find any association between C. pneumoniae and atherosclerosis and not isolate C. pneumoniae DNA from atherosclerotic specimens by PCR [5,6,8] A majority of studies have confirmed a high incidence of this microorganism in plaques and there are various reports of its incidence in different parts of the world for instance 14.3% in Turkey [9], 56% in South Africa [10], 71% in Canada [11], 33% to 61% in United States [12,13] and 17% to 29.4% in Iran [4,14,15]. Disparity in the prevalence of C. pneumoniae could be due to selection of samples, differences in the size of tested samples and using various methods such as serology, PCR, Immunocytochemistry, electron microscopy and culture at diverse periods.
According to a study by Bishara J et al., in punch biopsy samples of aortas of 61 patients with coronary artery bypass and 32 patients with carotid atheroma who underwent endarterectomy, there was evidence of C. pneumoniae infection [6]. Another study by Fong IW et al., revealed that in New Zealand white mice, respiratory infection with C. pneumoniae may cause atherosclerotic changes in aorta which are not caused by Mycoplasma pneumoniae infection (with similar pathologic changes in the lung). These findings may support the idea of C. pneumoniae’s role in atherosclerosis but cannot prove it [16]. In a study by Jackson LA et al., it was revealed that C. pneumoniae has a specific affinity towards cardiovascular tissues, so that autopsy samples of coronary arteries contained C. pneumoniae in 34% of cases, while this percentage was 13% in lung, 10% in liver, 5% in spleen,10% in bone marrow and 5% in lymph nodes [17]. However, C. pneumoniae was found in 11% of autopsy samples of coronary arteries in our study and the difference may be due to different geographical positions of the studies. Although, study was conducted by Muhlestein JB et al., showed that intranasal C. pneumoniae infection of rabbit model fed with chow supplemented with a small amount (0.25%) of cholesterol would result in significant acceleration of atherosclerosis, our study has shown that, there was no statistically significant difference between hyperlipidemia and acceleration of atherosclerosis [18]. The reviewed studies are carried out in various countries to verify this relationship from a seroepidemiological or histopathological point of view [12-15,19]. Our results are in agreement with 9 studies which were conducted in different countries and revealed a positive relation between C. pneumoniae and atherosclerosis [4,9-16].
The study by Paterson DL et al., on 17 autopsy samples of carotid atherectomy and 16 coronary arteries was done by PCR test to detect C. pneumoniae, which showed nothing in any of the samples. Therefore, they finally declared that although it is an interesting theory but no proof has been found for it in Australian patients [8]. The results are inconsistent with present study, may be due to difference in methods of testing. A study by Dabiri H et al., on 64 samples (33 from patients with atherosclerotic plague and 31 from healthy subjects) indicated that the DNA of C. pneumoniae was observed in 21% of patients while no such DNA was found in healthy individuals [4].
Various epidemiological studies determining prevalence of C. pneumoniae infection in different geographical areas could be effective to clarify the type of disease and the therapeutic approaches [9,12,14]. Accordingly, we performed our study on the corpses referred to the Iranian Legal Medicine Organisation as a center which is scarcely studied in this regard. In consistent with previous reports, our finding revealed that 15 percent of autopsy samples had been infected with C. pneumoniae [4,10].
The present study showed the incidence of C. pneumoniae in atherosclerotic plaque of coronary artery autopsy samples was 15.5%. Also, an incidence of 17% was reported in another study in Iran on 26 atherosclerotic plaques which is consistent with our results [4]. Presence of C. pneumoniae in more than 15% of atherosclerotic plaques and its absence in healthy vessels confirms its possible role in atherogenesis. However, its absence in more than 75% of atherosclerotic plaques reveals the fact that C. pneumoniae is not a necessary part of the process of atherogenesis and may only play a role in its initiation or progress. It was also indicated that myocardial infarction was higher but with no statistically significant difference which is consistent with the results of the present study [4].
Limitation
Methodological limitation of this study was small sample size.
Conclusion
Since, atherosclerosis is progressive disease, there are surely other factors involved in development of atherosclerotic plaques and presence of C. pneumoniae in plaques per se does not confirm its role in development of atherosclerosis. However, it seems necessary to study on presence of C. pneumoniae and its relation with other risk factors involved in atherogenesis and providing a proof of the role of infections in atherogenesis in order to help in diagnosis and treatment of the disease.
p-value by Two-tailed Fisher’s exact test is significant at p<0.05
Significant level: p<0.05
[1]. Libby P, Ridker PM, Maseri A, Inflammation and atherosclerosisCirculation 2002 105(9):1135-43.10.1161/hc0902.10435311877368 [Google Scholar] [CrossRef] [PubMed]
[2]. Damodar DM, Bhat Kishore G, Aruneshwari D, Detection of multiple microbial DNA in atheromatous plaques by polymerase chain reactionInt Res J Pharm 2011 2(5):214-19. [Google Scholar]
[3]. Wagenseil JE, Mecham RP, Vascular extracellular matrix and arterial mechanicsPhysiological reviews 2009 89(3):957-89.10.1152/physrev.00041.200819584318 [Google Scholar] [CrossRef] [PubMed]
[4]. Dabiri H, Rezadehbashi M, Badami N, Aghanouri R, Ahmadi H, Khoramizadeh MR, Detection of Chlamydia pneumoniae in atherosclerotic plaques of patients in Tehran, IranJpn J Infect Dis 2009 62(3):195-97. [Google Scholar]
[5]. Holland SM, Gaydos CA, Quinn TC, Detection and differentiation of Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae by DNA amplificationJ Infect Dis 1990 162(4):984-87.10.1093/infdis/162.4.9842401796 [Google Scholar] [CrossRef] [PubMed]
[6]. Bishara J, Pitlik S, Kazakov A, Sahar G, Haddad M, Vojdani A, Failure to detect Chlamydia pneumoniae by cell culture and polymerase chain reaction in major arteries of 93 patients with atherosclerosisEur J Clin Microbiol Infect Dis 2003 22(5):300-02. [Google Scholar]
[7]. Saikku P, Mattila K, Nieminen M, Huttunen J, Leinonen M, Ekman MR, Serological evidence of an association of a novel Chlamydia, TWAR, with chronic coronary heart disease and acute myocardial infarctionThe Lancet 1988 332(8618):983-86.10.1016/S0140-6736(88)90741-6 [Google Scholar] [CrossRef]
[8]. Paterson DL, Hall J, Rasmussen SJ, Timms P, Failure to detect Chlamydia pneumoniae in atherosclerotic plaques of Australian patientsPathol 1998 30(2):169-72.10.1080/003130298001691669643499 [Google Scholar] [CrossRef] [PubMed]
[9]. Adiloglu AK, Ocal A, Can R, Duver H, Yavuz T, Aridogan BC, Detection of Helicobacter pylori and Chlamydia pneumoniae DNA in human coronary arteries and evaluation of the results with serologic evidence of inflammationSaudi med J 2005 26(7):1068-74. [Google Scholar]
[10]. Kuo CC, Shor A, Campbell LA, Fukushi H, Patton DL, Grayston JT, Demonstration of Chlamydia pneumoniae in atherosclerotic lesions of coronary arteriesJ Infec Dis 1993 167(4):841-49.10.1093/infdis/167.4.8418450249 [Google Scholar] [CrossRef] [PubMed]
[11]. Chiu B, Viira E, Tucker W, Fong I, Chlamydia pneumoniae, cytomegalovirus, and herpes simplex virus in atherosclerosis of the carotid arteryCirculation 1997 96(7):2144-48.10.1161/01.CIR.96.7.21449337182 [Google Scholar] [CrossRef] [PubMed]
[12]. Campbell LA, O’Brien ER, Cappuccio AL, Kuo CC, Wang SP, Stewart D, Detection of Chlamydia pneumoniae TWAR in human coronary atherectomy tissuesJ Infec Dis 1995 172(2):585-88.10.1093/infdis/172.2.5857622912 [Google Scholar] [CrossRef] [PubMed]
[13]. Muhlestein JB, Hammond EH, Carlquist JF, Radicke E, Thomson MJ, Karagounis LA, Increased incidence of Chlamydiaspecies within the coronary arteries of patients with symptomatic atherosclerotic versus other forms of cardiovascular diseaseJ Am Coll Cardiol 1996 27(7):1555-61.10.1016/0735-1097(96)00055-1 [Google Scholar] [CrossRef]
[14]. Rostami Nejad M, Lahmi F, Nazemalhosseini H, Mojarad E, Godarzi H, Ahmadi H, Chlamydia pneumoniae infection in patients with atherosclerotic plaquesJ Army Univ Med Sci 2013 11:175-79. [Google Scholar]
[15]. Assar O, Nejatizadeh A, Dehghan F, Kargar M, Zolghadri N, Association of Chlamydia pneumoniae infection with atherosclerotic plaque formationGlob J Health Sci 2016 8(4):26010.5539/gjhs.v8n4p26026573036 [Google Scholar] [CrossRef] [PubMed]
[16]. Fong IW, Antibiotics Effects in a Rabbit Model of Chlamydia pneumoniae-Induced AtherosclerosisJ Infect Dis 2000 181(Supplement_3):S514-S9.10.1086/31560710839750 [Google Scholar] [CrossRef] [PubMed]
[17]. Jackson LA, Campbell LA, Schmidt RA, Kuo CC, Cappuccio AL, Lee MJ, Specificity of detection of Chlamydia pneumoniae in cardiovascular atheroma: evaluation of the innocent bystander hypothesisAm J Pathol 1997 150(5):1785 [Google Scholar]
[18]. Muhlestein JB, Anderson JL, Hammond EH, Zhao L, Trehan S, Schwobe EP, Infection with Chlamydia pneumoniae accelerates the development of atherosclerosis and treatment with azithromycin prevents it in a rabbit modelCirculation 1998 97(7):633-36.10.1161/01.CIR.97.7.6339495296 [Google Scholar] [CrossRef] [PubMed]
[19]. O’connor CM, Dunne MW, Pfeffer MA, Muhlestein JB, Yao L, Gupta S, Azithromycin for the secondary prevention of coronary heart disease events: the WIZARD study: a randomised controlled trialJ Am Med Assoc 2003 290(11):1459-66.10.1001/jama.290.11.145913129985 [Google Scholar] [CrossRef] [PubMed]