Cancer is the main cause of death in young people between 0 to 19-year-old. This well-known disease has a strong impact on the quality of life of patients and their families and treated as a complex public health problem in the private and public services [1,2]. Although mortality rate improvements are observed in developed countries [3], just a small progress has been achieved in undeveloped countries in the past years [2,4].
Childhood cancer is not fully understood, and prevention is not yet widespread. Early diagnosis and appropriate treatments are essential to increase patient cure and survival rates. When the population is unfamiliar with the predisposing factors and causes of childhood cancer, the opportunity to increase prevention rates remains small [1].
It has already been demonstrated through studies that there is a concern for understanding cancer in children in a more comprehensive way regarding etiological factors, the quality of life of patients, and their caregivers [5-7]. On the other hand, investigations that describe the profile of people with cancer and how this disease presents itself in the population, are important to support strategies related to the prevention of cancer [5].
Investigations that take information from a Hospital Records of Cancer (HRC) of a specific location provide information about the impact of cancer in its population [3,8]. In addition, registration is an important and necessary tool for the planning and evaluation of cancer prevention and control programs. The National Cancer Institute of Brazil (INCA) is responsible for the countrywide policy for cancer control and updating data in Brazil.
Childhood mortality is one of the socioeconomic indicators used to evaluate the life conditions of a specific population. Brazil, China, and Argentina has a higher childhood cancer mortality rate [9,10] when compared to developed countries, as the United States, Spain and Italy [1,3,8]. Thus, it is important to broadly understand the cancer profile in Brazil, and this study aimed to describe the epidemiological profile of childhood cancer in a 15-year period from the National Cancer Institute of Brazil data.
Materials and Methods
An epidemiological, ecological, sectional, and descriptive study with quantitative data approach was carried out in time series. The data collected came from the HRC, which is available for the public on the official website of the National Cancer Institute of Brazil (INCA). The population comprised the records of new cases of childhood cancer in the group age of 0 to 19 years. The HRC database has approximately 25 information sites covering about 260 hospitals in Brazil.
This study includes the data recorded during the period of 2000 to 2014, excluding the years of 2015 and 2016 because there is no complete information related to all states in the country in these years. The variables selected were: age, gender, previous history of cancer, most relevant base for diagnosis, primary tumour site and histological type of cancer. The registries without information about these interest variables were excluded. The age was the first variable considered, ranging from 0 to 19-year-old, in order to select only childhood cancer cases. In order to identify the primary diagnosis of cancer and the histological type, the International Classification of Diseases (ICD) was considered, containing nomenclature and the code of pathologies that were taken into account.
The selection of these independent variables was based on previous studies, which have emphasized the importance of primary diagnosis, tumour involvement site, and histological type of cancer as well as the genetic factors that directly influence the incidence of malignant tumours in childhood [1-3].
Ethical Issues: For the accomplishment of this study it was not necessary to obtain approval from the Ethics Committee, since it is secondary data, available for public consultation on the National Cancer Institute website.
Statistical Analysis
The descriptive (absolute and relative frequency) and inferential statistical analysis was performed using the SPSS software (20.0), using Chi-square test, Kolmogorov-Smirnov to test the data’s normal distribution, Kruskal-Wallis Test, and Mann-Whitney (5% significance level).
Results
During the period from 2000 to 2014, 57,006 cases of cancer were diagnosed and registered in children in Brazil, and males were more affected (n=30,851; 54.1%) than females (n=26,155; 45.9%). The mean age for the cases recorded was 9.48 (±6.08) years for males and 9.39 (±6.20) for females. The overall mean age was 9.64 years, the median was 10 years, and the mode was 19 years.
The variables of interest and their categories are described in [Table/Fig-1] according to the HRC database, where the variable “previous diagnosis” of cancer, shows a greater number of cases related to people without previous diagnosis (n=32,124, 56.4%). Previous diagnosis reflects on the medical history of the patients, if they were aware of any diagnosis of cancer and treatment before the current diagnosis recorded in the database. The most relevant basis for diagnosis was primary tumour histology (n=28,125; 49.3%) and clinical research (n=21,343; 37.4%).
Absolute and relative frequency of interest variables for childhood cancer according to gender in Brazil, between 2000 and 2014.
| Interest variables | n (%) | Male | Female | p-value |
|---|
| Previous diagnosis |
| Without diagnosis | 32,124 (56.4%) | 17,408 (54.2%) | 14,716 (45.8%) | 0.068 |
| With diagnosis, without treatment | 13,803 (24.2%) | 7,368 (53.4%) | 6,435 (46.6%) |
| With diagnosis and treatment | 11,079 (19.4%) | 6,075 (54.8%) | 5,004 (45.2%) |
| Most relevant base for diagnosis |
| Clinical | 694 (12.0%) | 387 (55.8%) | 307 (44.2%) | <0.0001 |
| Clinical Research | 21,343 (37.4%) | 11,491 (53.8%) | 9,852 (46.2%) |
| Imaging | 1,478 (2.6%) | 740 (50.1%) | 738 (49.9%) |
| Based on Tumour Markers | 285 (0.5%) | 162 (56.8%) | 123 (43.2%) |
| Cytology Test | 4,765 (8.4%) | 2,697 (56.6%) | 2,068 (43.4%) |
| Metastasis Histology | 316 (0.6%) | 180 (57.0%) | 136 (43.0%) |
| Primary Tumour Histology | 28,125 (49.3%) | 15,194 (54.0%) | 12,931 (46.0%) |
Chi-Square Test, (α=5%);
Considering the number of patients without previous diagnosis, the majority were male (n=17,408; 54.2%). For those cases with previous diagnosis but no established treatment, the majority was also represented by males (n=7,368; 53.4%). In cases where cancer recurrence was detected (with diagnosis and treatment), men were the most affected group (n=6075; 54.8%).
For the association between “most relevant basis for diagnosis” and gender, the greatest proportion indentified for males was metastasis histology (57.0%), for relative frequency. For females, diagnostic imaging was the main proportion (49.9%), with a significance level of p<0.0001[Table/Fig-1].
The most prevalent histological types and primary tumour sites for childhood cancer in Brazil are shown in [Table/Fig-2,3]. During the period of investigation, acute lymphoblastic leukaemia was the most frequent histological type of cancer (n=7,149; 12.6%). Regarding tumour localization, the most frequent site was the bone marrow (n=15,936; 28.0%).
Prevalence and mean age of histological type of childhood cancer in Brazil in the period 2000-2014.
| Histological Type | n | % | Mean Age (±SD) |
|---|
| Acute Lymphoblastic leukaemia | 7,149 | 12.6 | 7.58 (±5.21)a |
| Acute Myeloid leukaemia | 2,609 | 4.6 | 9.49 (±5.93)b |
| Nephroblastoma (Wilms’ tumour) | 2,295 | 4.0 | 3.69 (±3.18)c |
| Osteosarcoma | 2,244 | 3.9 | 13.65 (±3.60)d |
| Neuroblastoma | 1,820 | 3.2 | 2.93 (±3.34)c |
| Hodgkin lymphoma | 1,680 | 2.9 | 13.43 (±4.48)d |
| Retinoblastoma | 1,450 | 2.5 | 1.90 (±1.94)f |
| Medulloblastoma | 1,443 | 2.5 | 8.03 (±4.77)a |
| Nodular sclerosis Hodgkin lymphoma | 1,352 | 2.4 | 13.85(±4.30)d |
| Burkitt lymphoma | 1,342 | 2.4 | 7.83 (±4.88)a |
| B-cell acute lymphoblastic leukaemia | 1,314 | 2.3 | 6.99 (±5.15)a |
| Ewing sarcoma | 1,282 | 2.2 | 12.30 (±4.60)d |
| Non-Hodgkin lymphoma | 1,202 | 2.1 | 11.44 (±5.48)e |
| Lymphoid leukaemia | 1,066 | 1.9 | 7.45 (±5.15)a |
| Embryonal rhabdomyosarcoma | 875 | 1.5 | 8.62 (±5.76)b |
| Malignant glioma | 760 | 1.3 | 7.57(±4.37)a |
| Astrocytoma | 680 | 1.2 | 9.47 (±5.31)b |
| Acute promyelocytic leukaemia | 611 | 1.1 | 11.79 (±5.06)e |
| Ependymoma | 543 | 1.0 | 7.63 (±5.57)a |
n: Number of cases; SD: Standard deviation
Kruskal-Wallis and Mann-Whitney test. Significance Level of 5%. Different lowercase letters indicate a statistically significant difference between the groups.
Prevalence of primary tumour site and mean age of childhood cancer in Brazil in the period 2000-2014.
| Primary tumour site | n | % | Mean Age (±SD) |
|---|
| Bone marrow | 15,936 | 28.0 | 8.38 (±5.66)a |
| Lymph node | 6,134 | 10.8 | 12.19 (±5.19)b |
| Bone | 3,953 | 6.9 | 13.17 (±4.29)b |
| Kidney | 2,766 | 4.9 | 4.25 (±4.08)c |
| Gland | 2,644 | 4.6 | 11.07 (±6.57)b |
| Cerebellum | 1,613 | 2.8 | 8.15 (±4.91)a |
| Encephalon | 1,611 | 2.8 | 16.11 (±5.52)d |
| Retina | 1,510 | 2.6 | 1.90 (±1.99)e |
| Brain | 1,417 | 2.5 | 9.11 (±5.48)f |
| Testicle | 1,160 | 2.0 | 3.49 (±6.51)c |
| Ovary | 1,157 | 2.0 | 13.37 (±4.66)b |
| Skin | 1,011 | 1.8 | 11.71 (±6.26)b |
n: number of cases; SD: Standard deviation
Kruskal-Wallis and Mann-Whitney test. Significance Level of 5%. Different lowercase letters indicate a statistically significant difference between the groups.
Age distribution varied considerably between histological type and primary tumour sites. Among the most prevalent tumour sites, the mean age of 1.90 (±1.94) was registered for lesions located in the retina. On the other hand, central nervous system neoplasms affected patients with a mean age of 16.11 (±5.22). Regarding the histological variation types, the mean age (2.93±3.34) was observed for neuroblastoma, and the maximum mean was observed for Hodgkin Lymphoma (13.43±4.48). These data are described in [Table/Fig-2,3].
The distribution over 15 years showed that 2010 was the year with the highest number of childhood cancer registries (n=6,062; 10.6%). For the other years, the following distribution was observed in the years: 2000 (n= n=3,002; 5.3% ;) 2001 (n=3,462; 6.1), 2002 (n= 3,522; 6.2%), 2003 (n= 3504; 6.1%;); 2004 (n= 3,787; 6.6%), 2005 (n= 8,872; 6.8%), 2006 (n= 4,254; 7.5%), 2007 (n=4,363; 7.7%), 2008 (n= 4,671; 8.2%), 2009 (n= 4,208; 7.4%), 2011 ( n= 5,417; 9.5%), 2012 (n= 3,333; 5.8%), 2013 (n= 2,542; 4.5%), 2014 (n= 1,007; 1.8 %).
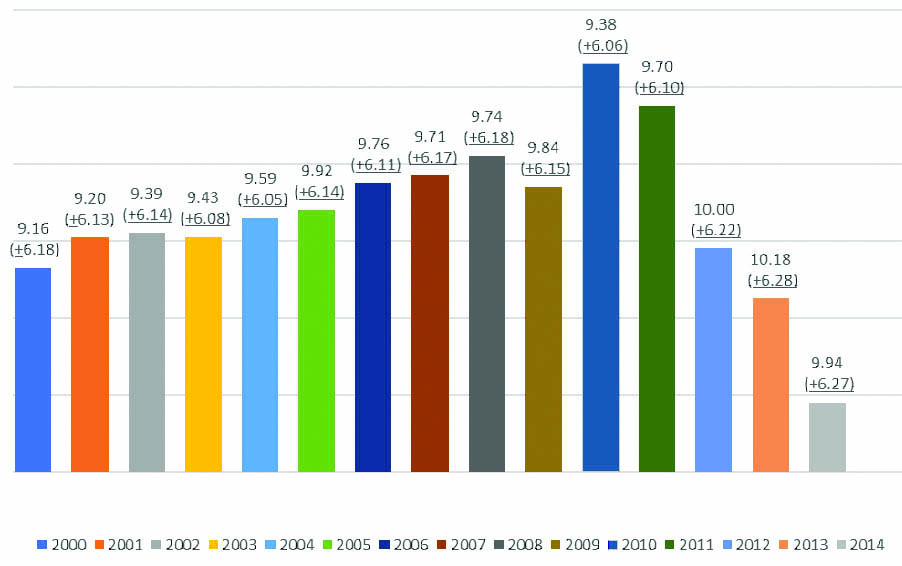
The mean age recorded for each year from 2000 to 2014 is shown in [Table/Fig-4].
Mean age (years) of childhood cancer, 57,006 cases in Brazil, between 2000 and 2014.
Discussion
The aim of this study was to establish the profile of Paediatric patients with cancer over a 15-year period in Brazil, from the main HRC in the country, in order to have a full comprehension of these patients and provide subsidies for the elaboration of public health policies. It was verified that young men with no previous history of cancer and a mean age of 9.64 years are more affected by cancer. This disparity by gender is observed in other studies, with the highest rates among males [5,8].
The most relevant basis for diagnosis was represented by primary tumour histology (49.3%) and clinical research (37.4%). Clinical research comprises not only clinical examination (visual), but consists in a deep research, involving laboratory analysis (e.g., blood tests), family history findings, and full examination for signs and symptons. Conforming to this data, a continued and detailed clinical practice and complete anamnesis are important to improve detection of the signs and symptoms affecting childhood cancer. Most of the time, they show similar clinical history that guides the diagnosis, as long as there is a careful investigation to identify predisposing and determinant factors, along with complementary exams: such as primary tumour histology, imaging and cytology. The previous identification of the type of cancer through biopsy has led to an accurate diagnosis and a reduction in complications during surgeries [9]. The diagnosis of cancer should be performed as early as possible to ensure a safer prognosis. Thus, the importance of meticulous clinical research and complementary exams is justified.
The most frequent sites for primary tumours in Paediatric patients in Brazil are represented by the bone marrow, lymph nodes, bones, and kidney, which are the same location of the most prevalent histological types of cancer such as acute lymphoblastic leukaemia, acute lymphocytic leukaemia, Wilms’ tumour, and osteosarcoma. Lymphocytic leukaemia was also one of the most prevalent types in other countries, such as Spain, Italy, Argentina and United States, recognized as the most common histological childhood cancer pattern in the literature [1,3,10,11].
It was verified through our study that cancers that affect children in early childhood are Retinoblastoma (1.90±1.949) and Wilms’ tumour (3.69±3.181). The diagnosis of embryonal tumours in early life occurs through medical monitoring from birth in public or private health services [3].
In late childhood, Osteosarcoma (13.65±3.60), Hodgkin lymphoma (13.43±4.48) and Ewing Sarcoma (12.30±4.60), were the most observed cancers. The results obtained from our study differ from epidemiological studies conducted in other countries, such as Italy and the United States [3,11,12], where Osteosarcoma was not the most frequent type in adolescents. In Italy, it was observed that Lymphoma and Lymphoid leukaemia were the most prevalent in this age group; and in the USA, the most common type of cancer is Lymphoma (21%), Brain and nervous system (17%), and Leukaemia (14.0%). Osteosarcoma is an aggressive malignant neoplasm that arises from primitive transformed cells of mesenchymal origin with the capacity to produce immature bone, and it is commonly found in youngers until the third decade of life [13], as found in the present study.
Genetic and epigenetic factors might be related to the onset and type of childhood cancer. Despite the difference between genetic standards, leukaemia is the most prevalent type of childhood cancer [8,12-14]. As also observed in this study, the most prevalent histological types of cancer are: Acute Lymphoblastic Leukaemia and Acute Myeloid Leukaemia. The mean age for the these two types of leukaemia was 9.14 (±1.5) years, which is in agreement with other studies [3,10,15], where Leukaemia (Lymphoblastic and Myeloid) is the most frequent type of childhood cancer.
Among the most prevalent histological types of cancer, it is important to note that retinoblastoma, neuroblastoma, and Wilms’ tumour are the most frequent types in children with low age, as observed in other countries [3,16]. The retinoblastoma has a high prevalence and is the most common ophthalmic tumour in our study. Studies carried out in Argentina and the United States also observed a high prevalence of this type of cancer in early childhood, mainly in the age group between 1-3 years [10,13,16]. Brain tumours, such as neuroblastoma, are considered cancers with worse prognosis in general and are found in corresponding prevalence compared to a study carried out in the United States [13], which differs from the study carried out in Italy [3]. Wilms’ tumour is the most common genitourinary tumour detected in children. The maximum incidence occurs between 2 to 3 years of life [17,18]. The incidence variation and/or prevalence support the investigation of the spatial distribution of genetic profiles presented in distinct populations. Brazil is considered a developing country, but the high number of malignant tumours detected in children in their first few years reflects the improvement in public health and primary care in recent years, thus resulting in early treatment and increasing the chances of a cure.
[Table/Fig-2] shows the statistical differences between the age of detection and the histological type of cancer. Regarding the site of the tumour, it was verified that the cancers in the cerebellum and bone marrow mainly affect children with an average age of 8 years. There is a higher prevalence of cancer in the lymph nodes of children with a mean age of 12.19 (±5.19). Cancer affecting the kidney is more observed in children with a mean age of 4.25 (±4.08), and testicles is more observed with a mean age of 3.49 (±6.51). Osteosarcoma and Burkitt lymphoma are found in children with mean age of 13 years and 7.4 years respectively. Acute lymphoblastic, acute lymphocytic, and medulloblastoma are found in patients with similar ages (7-8 years). Wilms’ tumour and neuroblastoma represent the histological types of cancer that mainly affect children between 2 and 3 years. There were no study found in the literature evaluating the relationship between tumour sites and histological types of cancer with involvement at similar ages. Studies investigating the relation between the tumour site and the histological type of neoplasia, and if this relation has an effect on similar ages, should be carried out.
In this study, there was a higher frequency of Leukaemia, followed by Wilms’ tumour and Osteosarcoma. Wilms’ tumour presented a considerable prevalence in Brazil, but it is not a highly prevalent tumour in other countries, such as Argentina. China, Italy, and United States [3,10,13,19]. In relation to developing countries, a study carried out in Argentina showed that the most prevalent types were Leukaemia, Lymphoma and Tumours of the Central Nervous System [10]. In China, the most prevalent types of cancer were Leukaemina, followed by germ cell neoplasms and Neuroblastomas [19].
This temporal evaluation, for 15 years, demonstrated that the prevalence of the childhood cancer in Brazil is worrisome. This might be partially explained by the failure of prevention programs, greater population exposure to risk factors, modifications to lifestyle, and genetic alterations. According to Isaevska et al., in a similar study carried out in Italy, no satisfactory explanation has been found for this prevalence, and efforts should be made to understand and interpret this peculiar pattern, thus encouraging new studies to identify what might influence this prevalence [3].
As shown through this study results, there has been a slight increase over the years, and the highest incidence was found in 2010 (n=6062; 10.6%). However, these data might be related to the improvement of cancer registration that feeds the database used in Brazil for the year 2010, population increase, and health prevention and promotion program development, as already addressed by other researchers who used the database to study cancer [20,21]. For the subsequent years, a significant decrease is observed. No study was found to justify this reduction. This result may be a consequence of the lack of hospital records when obtaining the diagnosis.
Studies carried out through databases inserted in information systems may show limitations, since records with no complete information might not be included, and reliability of data and source must be verified. However, the importance of this method of scientific research is considered by the valorization of information systems and their databases, which is a relevant source to collect information from various locations in the world.
Conclusion
Childhood cancer affects, to a greater proportion, males without previous history of cancer, with a mean age of 9.64 years. The most relevant basis for diagnosis was primary tumour histology, followed by clinical research. The most prevalent types of neoplasms were Acute Lymphoblastic Leukaemia and Acute Myeloid Leukaemia. For younger children, retinoblastoma and Wilms’ tumour were more prevalent than other types of cancers, compared to Hodgkin lymphoma and osteosarcoma in older children. Thus, efforts should be made to understand and interpret this peculiar and misunderstood pattern of childhood cancer prevalence.
Chi-Square Test, (α=5%);
n: Number of cases; SD: Standard deviationKruskal-Wallis and Mann-Whitney test. Significance Level of 5%. Different lowercase letters indicate a statistically significant difference between the groups.
n: number of cases; SD: Standard deviationKruskal-Wallis and Mann-Whitney test. Significance Level of 5%. Different lowercase letters indicate a statistically significant difference between the groups.