“Electrocardiogram Changes with Elevated Troponins Mimicking MI: All that Glitters is not Gold”
Monika Bhandari1, Pravesh Vishwakarma2, Akshyaya Pradhan3, Rishi Sethi4
1 Assistant Professor, Department of Cardiology, King George’s Medial University, Lucknow, Uttar Pradesh, India.
2 Assistant Professor, Department of Cardiology, King George’s Medial University, Lucknow, Uttar Pradesh, India.
3 Assistant Professor, Department of Cardiology, King George’s Medial University, Lucknow, Uttar Pradesh, India.
4 Professor, Department of Cardiology, King George’s Medial University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Akshyaya Pradhan, Assistant Professor, Department of Cardiology, King George’s Medial University, Lucknow-226003, Uttar Pradesh, India.
E-mail: akshyaya33@gmail.com
Temporary transvenous pacing is often required as life saving measure in conditions such as Stokes Adams attack and symptomatic bradyarrhythmias. Bradyarrhythmias are also known complications of acute Myocardial Infarction (MI), which can be transient or persistent and often demand temporary pacing too. It is difficult to diagnose underlying MI in the setting of paced rhythm due to secondary ST-T changes. Elevated cardiac enzymes are essential in the scenario of paced rhythm to diagnose underlying acute MI. Remarkable T wave inversion and ST depression {similar to Left Bundle Branch Block (LBBB)} do occur in right ventricular paced ECG and some changes may persist following withdrawal of pacing (cardiac memory T waves) simulating ischaemia. Very rarely arrhythmias can also lead to troponin rise causing diagnostic dilemma in such a setting. Here, we report a case of an elderly female who presented with symptomatic Complete Heart Block (CHB) and developed T wave inversion with Q wave formation in anterior leads in sinus rhythm following temporary pacing. She also demonstrated a dynamic rise in serial cardiac troponin values mimicking an acute coronary syndrome. Ultimately, an invasive coronary angiogram was performed to rule of significant coronary artery disease.
Bradyarrhythmia, Cardiac memory, Coronary angiogram, ST-T changes, Transvenous pacing
Case Report
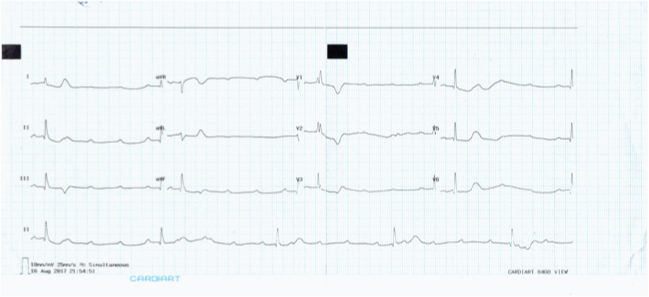
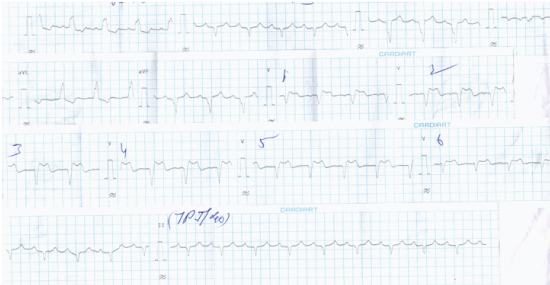
A 69-year-old female was admitted in the Emergency Department with complaints of recurrent episodes of syncope for past three days. There was no history of associated chest pain and dyspnea. On examination, she had a pulse rate of 32 beats per minute and blood pressure of 140/96 mmHg. Her Electrocardiogram (ECG) demonstrated complete dissociation of P wave and QRS wave suggesting CHB with a Right Bundle Branch Block (RBBB) type escape rhythm [Table/Fig-1]. Patient was immediately shifted to catheterisation laboratory and temporary transvenous pacemaker was implanted with pacing lead positioned at right ventricular apex under fluoroscopic guidance. The procedure was uneventful and all her blood investigations including renal functions and electrolytes were within normal range. Her cardiac troponin T (high sensitive assay) at admission; however, was 0.021 ng/mL (Normal <0.014 ng/mL, Elecsys assay, Roche diagnostics, Indianapolis, USA). The patient regained sinus rhythm on third day of admission but ECG showed T wave inversion in anterior leads with LBBB along with Q waves which persisted on repeated recordings [Table/Fig-2]. At admission because her troponin was elevated, a repeat assay was ordered to rule out ischaemia. Her second troponin value rose from 0.021 ng/mL to 0.047 ng/mL (almost doubled). However, the echocardiography did not show any Regional Wall Motion Abnormality (RWMA) and left ventricular systolic function was normal. However, in view of patient’s advance age, ECG changes and rising cardiac enzymes Coronary Angiography (CAG) was done which revealed normal coronary arteries [Table/Fig-3]. Finally taking into account all the above findings, patient was considered to be a case of degenerative disease of conduction system of heart and ECG changes were likely to be depolarisation abnormality secondary to pacing. A permanent pacemaker was implanted and patient was discharged in stable condition. At her one month follow-up in pacemaker clinic, her pacing parameters were in range.
12 Lead electrocardiogram at admission demonstrating complete heart block with RBBB type ventricular escape rhythm at rate of <40/min.
12 lead electrocardiogram depicting return of spontaneous rhythm with ST elevation and T wave inversion with QS in anterior leads suggestive of LBBB (arrows).
Coronary angiogram showing normal left coronary artery (left panel) and right coronary artery (right panel). The temporary transvenous pacing lead can also seen in-situ.

Discussion
Temporary intravenous pacing is often required as life saving measure in conditions such as Stokes Adams syndrome and symptomatic bradyarrhythmia [1]. Bradyarrhythmias are also known complications of acute MI, which can be transient or persistent and often demand temporary pacing too [2]. It is difficult to diagnose underlying MI in the setting of paced rhythm due to secondary ST-T changes. Elevated cardiac enzymes (preferably high sensitive troponins) help in diagnosing infarction in these settings.
It is known that secondary ST-T changes that develop following pacemaker implantation can persist even after pacing is discontinued (cardiac memory). Although, not common, such ST-T changes often induce the suspicion of coronary ischaemia and often mandate further evaluation. Initially, it was described by Chatterjee K et al., (hence, also called also as Chatterjee phenomenon) in 29 of 31 of their patients paced primarily for conduction blocks [3]. These changes were primarily influenced by duration of pacing and pacing output but not by atrial pacing or baseline QRS. The ECG changes could appear as early as 10 minutes of pacing when pacing was done with higher voltage with faster rates. In the present patient, ST segment elevation and T wave inversions along with Q waves developed on day three of temporary pacemaker implantation. Gautschi O et al., and more recently Behera S et al., have described similar memory ST-T changes in intrinsic rhythm following pacing [4,5]. Apart from cardiac pacing, other conditions producing such memory ST-T changes include intermittent LBBB, conduction over accessory pathway and episodes of tachycardia [6,7]. Although, the exact cause of such memory changes are not known, some studies have attributed it to potassium channel and cAMP responsive element binding protein [8].
It is advisable and we routinely estimate cardiac troponin at admission to rule out underlying acute MI in bradyarrhythmia’s presenting with an acute onset because bradyarrhythmia can be the first manifestation of acute MI and chest pain may not be a prominent feature in select subgroups (elderly, female, diabetic and dementia). High sensitive cardiac troponins are pivotal to diagnosis of acute MI and more so in cases with baseline ECG changes like bundle branch block, ventricular hypertrophy and paced rhythm [9]. Their advent has led to early diagnosis of MI and short waiting times in Emergency Department. Serial assessment of troponins correctly identifies MI and avoids misdiagnosis of other non coronary causes of troponin elevation [10]. However, uncommonly there can be rise in cardiac troponins following ventricular pacing in absence of acute MI as reported by Martignani C et al., and Nikolaou NI et al., [11,12]. The significance of such rise in troponin following pacing is unknown at present and needs further research.
In the present case, patient had complete heart block at hospitalisation, but ST-T changes developed after cessation of ventricular pacing. Concurrently, the cardiac troponins were also elevated leading to false alarm of acute MI. Highly sensitive cardiac troponin too can infrequently give rise to false positive results and despite doubling of cardiac troponin values on serial estimation in the present case no significant underlying disease in coronary arteries was detectable on CAG. Although, the pacemaker induced ECG changes usually do not confer any clinical significance, but they can simulate MI and lead to unnecessary prolonged hospital stay and unwarranted interventions.
The noteworthy combination of spurious ECG changes (pacing induced) and spurious troponin rise in the same individual-the two golden tenets essential for diagnosing acute MI in contemporary medicine makes us remember the wise idiom-All that glitters (ECG and troponin) may not be gold (ischaemia).
Conclusion
Pacing induced ST-T changes are uncommon but can occur. Diagnosis of MI in presence of paced rhythm is challenging and cardiac enzymes usually help in diagnosing underlying MI. However, cardiac enzymes too can rise falsely in many clinical scenarios and infrequently after pacing too. Coronary angiogram sometimes will be needed ultimately to rule out coronary artery disease is such cases. ECG changes and cardiac enzyme alterations should not be viewed in isolation and entire clinical scenario should be taken into account.
[1]. Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American college of cardiology/American Heart Association task force on practice guidelines (writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmic devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic SurgeonsJ Am Coll Cardiol 2008 51:e1-62. [Google Scholar]
[2]. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, ESC Guidelines on cardiac pacing and cardiac resynchronization therapyEur Heart J 2013 34:2281-329.10.1093/eurheartj/eht15023801822 [Google Scholar] [CrossRef] [PubMed]
[3]. Chatterjee K, Harris A, Davies G, Leatham A, Electrocardiographic changes subsequent to artificial ventricular depolarizationBr Heart J 1969 31:770-79.10.1136/hrt.31.6.7705358161 [Google Scholar] [CrossRef] [PubMed]
[4]. Behera SK, Samal AK, Pradhan AK, Temporary cardiac pacing-induced electrocardiographic changes simulating myocardial infarctionInt J Res Med Sci 2017 5:4172-74.10.18203/2320-6012.ijrms20174006 [Google Scholar] [CrossRef]
[5]. Gautschi O, Naegeli B, Cardiac memory mimicking Myocardial ischemiaJ R Soc Med 2003 96(3):131-32.10.1177/014107680309600309 [Google Scholar] [CrossRef]
[6]. Byrne R, Filippone L, Benign persistent T wave inversion mimicking ischemia after left bundle branch block-cardiac memoryAm J Emerg Med 2010 28(6):747.e5-6.10.1016/j.ajem.2009.10.00320637400 [Google Scholar] [CrossRef] [PubMed]
[7]. Sucu MM, Davutoglu V, Cardiac memory T-wave changes after ventricular tachycardia in pregnancyAm J Emerg Med 2008 26(8):968.e1-3.10.1016/j.ajem.2008.02.01118926372 [Google Scholar] [CrossRef] [PubMed]
[8]. Patberg KW, Plotnikow A, Giannulin R, Quamina A, Samaniengo L, Danilo P, Cardiac memory is associated with alterations in the cAMP responsive element binding protein and its phosphorylation formPACE 2001 24:645 [Google Scholar]
[9]. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC)Eur Heart J 2016 37:267-315.10.1093/eurheartj/ehv32026320110 [Google Scholar] [CrossRef] [PubMed]
[10]. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Third universal definition of myocardial infarctionEur Heart J 2012 33:2551-67.10.1093/eurheartj/ehs18422922414 [Google Scholar] [CrossRef] [PubMed]
[11]. Nikolaou NI, Christou AH, Spanodimos SG, Antonatos DG, Marked troponin elevation after implantation of a permanent antibradycardia pacemakerHellenic J Cardiol 2011 52(6):489-92. [Google Scholar]
[12]. Matignani C, Diemberger I, Biffi M, Ziacchi M, Saporito D, Valzania C, Troponin I rise after pacemaker implantation at the time of “universal definition of myocardial infarction”Am J cardiol 2009 103(8):1061-65.10.1016/j.amjcard.2009.01.00419361590 [Google Scholar] [CrossRef] [PubMed]