Radical cystoprostatectomy represents the most effective treatment for muscle-invasive non-metastatic bladder cancer [1]. The high incidence of sexual complications has been one of the reasons for development of alternative procedures like cystectomy with partial prostatectomy [2] cystectomy with adenoma enucleation [3] and cystectomy preceded by transurethral resection of prostatic tissue with preservation of the prostatic capsule. These potency-preserving techniques raise concern because of two essential risks: (a) involvement of the prostate by the urothelial cancer; (b) a possible association with incidental prostate cancer [1-3].
The frequency of incidentally detected prostate cancer is nearly 42% in men older than 50 years of age, and higher than 80% in men older than 80 years [4]. A large proportion of prostate cancer remains undiagnosed or clinically insignificant resulting in high frequency of autopsy detected cases. Cystoprostatectomy specimen obtained from patients with bladder cancer provides a unique opportunity to estimate the prevalence and to define the morphological features of silent (incidental) adenocarcinoma of prostate. The aim of this study was to determine prevalence and histopathological features of incidental prostate carcinoma detected in radical cystoprostatectomy specimens for muscle invasive bladder cancer.
Materials and Methods
A retrospective chart review of patients who underwent radical cystoprostatectomy for infiltrating bladder tumors during the period between 2003 and April 2014 was done in our Department. A total of 123 patients underwent radical cystectomy for invasive bladder cancer at our Institute. Of these, 113 patients were males. Patients who underwent PSA screening, desired prostate sparing surgery or had any surgical procedure for benign prostate disease were excluded from the study.
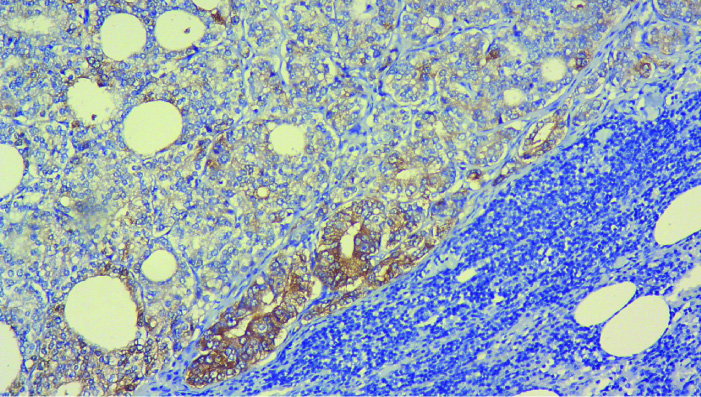
The histopathology slides of these patients were reviewed. Gleason Score (GS), seminal vesicle invasion, extracapsular extension, type of tumour (ductal/acinar) and lymph nodal involvement by adenocarcinoma prostate, confirmed by Immunohistochemistry (IHC) staining for PSA [Table/Fig-1] was determined. Associated or isolated Atypical Small Acinar Proliferation (ASAP) and High Grade Prostatic Intraepithelial Neoplasia (HGPIN) were also noted. Specimens with adenocarcinoma prostate fulfilling all the following criteria were defined as insignificant: (a) GS<=6 without Gleason pattern 4 or 5; (b) Organ confined disease; (c) tumour volume <0.5cc (dominant nodule) [5,6].
Photomicrograph showing tumour cells positive for Prostate Specific Antigen (PSA) staining on Immunohistochemistry (IHC) in a background of lymphoid tissue.
Statistical Analysis
Continuous variables were expressed as mean±standard deviation, whereas categorical variables were expressed as frequency and percentage.
Results
Adenocarcinoma prostate was detected in 14 out of 113 specimens with an overall prevalence of 12.4%. Eight of these patients had received neoadjuvant chemotherapy with Gemcitabine and Carboplatin for bladder cancer. The mean patient’s age was 65 years (range 48-75 years). The median Gleason Score was 3+3 (3+3, 4+3); (64%) had GS of 3+3, three patients (22%) had a GS of 3+4 and two (14%) had GS 4+3. As per Tumour (T) stage, seven patients (50%) had T2c and four patients (29%) had T2a disease. Three patients had locally advanced disease, one with seminal vesical invasion (GS 3+3) and two patients with extra prostatic extension [Table/Fig-2].
Characteristics of carcinoma prostate diagnosed incidentally in radical cystoprostatectomy specimen.
| Age (yrs) | T Staging (UB) | Operative Procedure | GS | T Staging (CaP) | Nodal Status | Significant Tumour | Diffuse HGPIN | Peri-op CT | Total Nodes | PSA** (ng/ml) | Bone scan |
|---|
| 63 | T2a | RC+IC | 3+3 | T2a | N0 | N | Y | N | 15 | 0.03 | NA |
| 71 | T2b | RC+ONB | 3+4 | T2c | N1(PSA) | Y | Y | N | 16 | 0.2 | Negative |
| 67 | T1 | RC+IC | 3+3 | T3b | N1(PSA) | Y | Y | N | 15 | 0.1 | Negative |
| 75 | yT0 | RC+IC | 3+4 | T3a | N1(PSA) | Y | Y | Y | 16 | 0.01 | Negative |
| 58 | T1G3 | RC+IC | 3+3 | T3a | N0 | Y | Y | Y | 14 | 0.05 | NA |
| 70 | yT0 | RC+IC | 3+4 | T2c | N0 | Y | N | Y | 11 | 0.001 | NA |
| 48 | T4a | RC+IC | 3+3 | T2a | N0 | N | N | Y | 15 | 0.035 | NA |
| 49 | T2a | RC+NB | 3+3 | T2a | N0 | N | N | N | 17 | 0.004 | NA |
| 73 | T2b | RC+IC | 3+3 | T2a | N0 | Y | Y | Y | 13 | 0.1 | NA |
| 73 | T4a | RC+IC | 3+3 | T2a | N0 | N | Y | N | 11 | 0.02 | NA |
| 71 | T4a | RC+CU | 3+3 | T2c | N0 | Y | Y | Y | 7 | 0.1 | NA |
| 72 | T1 | RC+IC | 3+3 | T2c | N0 | N | Y | N | 12 | 0.008 | NA |
| 64 | T3a | RC+CU | 4+3 | T2c | N0 | Y | Y | Y | 16 | 0.12 | NA |
| 58 | T1 | RC+ONB | 4+3 | T2c | N1(PSA) | Y | Y | Y | 15 | 0.1 | Negative |
UB: Urinary bladder; GS: Gleason score; CaP: Carcinoma prostate; HGPIN: High grade prostate intraepithelial neoplasm; RC: Radical cystectomy; ONB: Orthotopic neobladder; IC: Ileal conduit; CU: Cutaneous ureterostomy; CT: Chemotherapy; PSA: Prostate specific antigen; NA: Non applicable
**After surgery
Pelvic lymph node metastasis from adenocarcinoma prostate was detected in four patients, which was confirmed with PSA staining of the nodes [Table/Fig-1]. None of these patients had evidence of metastatic lymph nodes on Computerized Tomography of abdomen and pelvis (CT). Two of these patients had GS 3+4, with T2b and T3a disease respectively. One patient had GS 4+3 and T2c disease. One patient with LN metastasis had GS 3+3 with SV invasion on one side. Two of these patients had received neo-adjuvant chemotherapy with gemcitabine and carboplatin [Table/Fig-2]. Four patients had ASAP and 1 had diffuse high grade PIN with no evidence of carcinoma prostate. 10 out of 14 patients with Carcinoma prostate (CaP) had associated diffuse high grade PIN on HPE. As per the definition of significant tumour given by Ohori and Epstein et al., 64% of all incidental CaP were significant in our study [Table/Fig-3] [5,6].
Isolated ASAP/HGPIN patient details.
| Age (years) | T staging (UB) | Operative procedure | HGPIN/ASAP | Nodal status | Total nodes dissected | Peri-op CT |
|---|
| 70 | T3a | RC+IC | ASAP | N0 | 13 | Y |
| 60 | T3a | RC+ONB | ASAP | N0 | 19 | Y |
| 72 | T1 | RC+IC | ASAP | N0 | 12 | N |
| 62 | T3a | RC+IC | HGPIN | N0 | 14 | N |
| 62 | T1 | RC+IC+ URETHRECTOMY | ASAP | N0 | 18 | Y |
HGPIN: High grade prostate intraepithelial neoplasm; ASAP: Atypical small acinar proliferation; RC: Radical cystectomy; ONB: Orthotopic neobladder; IC: Ileal conduit, CT: Chemotherapy
One patient expired in the post-operative period due to ureteric anastomotic leak leading to sepsis and Multi Organ Dysfunction (MODS). 3 out of 4 patients with Lymph Node (LN) positive CaP underwent medical or surgical castration (as per patient preference) and followed up 6 monthly with PSA. On a mean follow-up of 2.5±1.2 years, these patients had no evidence of disease progression (clinical or biochemical). One patient with LN positive CaP was followed up with serial PSA (patient refused therapy) and underwent castration after one year when there was PSA rise. Two patients lost to follow up. Of the remaining seven patients, one developed adenocarcinoma stomach after 2 years. He underwent surgery and adjuvant chemotherapy for stomach cancer. On a mean follow-up of 3.5±1.5 years, the other six patients had no evidence of disease progression (clinical or biochemical) [Table/Fig-4].
Follow-up of patients stratified as per pathological nodal status.
| Node Positive (PSA positive) patients |
|---|
| Total | Hormone Therapy | Mean BCR free survival (n=4) |
|---|
| 4 | 3 (one patient refused) | 2.5 years |
| Node negative patients |
|---|
| Total | Lost to follow up | Mortality | Mean BCR free survival (n=6) |
|---|
| 10 | 2 | 2 (One non prostate cancer specific mortality) | 3.5 years |
Discussion
The frequency of incidentally discovered CaP in radical cystoprostatectomy specimens is extremely variable among the most relevant published series. In our study we noted the prevalence to be 12.4%. This is much lower than overall mean frequency in other series (range 23-68%) [7,8]. This variability can be explained by different pathological sampling protocols used. Ruffion et al., found a 51.0% rate of incidentally detected CaP, advocating the use of 2.5 mm prostate slices [8]. Similar results were seen in the study by Abbas et al., who examined prostatic tissue from 40 radical cystoprostatectomy specimens with serial step slices taken at 2 to 3-mm intervals [9]. On the other hand, variability can also be noted when considering those using a different pathologic examination protocol with 5-mm sections. Yang et al., reported rate of incidentally detected CaP as 21%. At our center, we routinely sample the prostate taking 5 mm cut [10].
In our study majority of patients (64%) had low-grade disease with GS 3+3. On basis of the criteria to define significant tumour by Ohori et al., and Epstein et al., 64% of all tumours were significant in our study. Revelo et al., reported a 41% rate of unsuspected CaP, with 48% being considered clinically significant [11]. In a series of 141 cystoprostatectomies by Delongchamps et al., 30% were considered insignificant [12] Montironi et al., concluded that incidentally detected CaP is less aggressive than CaP clinically detected with regard to stage, Gleason score, and surgical margin status. The same group investigated the expression of some of the markers of aggressiveness i.e., nuclear and nucleolar size, proliferation activity assessed as Ki- 67 index, HER2 gene amplification, HER2 protein expression, endothelin-1 in incidental cancer. They pointed out that incidental cancers are different from clinical ones in terms of marker expression, having cell features of less aggressiveness [13]. The proportion of clinically significant cancers in various series published previously varies from 10% to 70% [12]. Such wide variability could be related to different criteria adopted to define clinically significant cancer, different pathological techniques and the population under investigation. In conclusion, there is no consensus in defining clinically insignificant prostate cancer.
Total four cases of node positive disease (28%) were confirmed to be of prostatic origin using PSA staining. Nodal involvement by incidental carcinoma prostate has not been reported by most of the other series in the past. These CaP patients had Gleason pattern 4 on HPE or seminal vesicle invasion/extra capsular spread. Abdelhady et al., in their review of 58 radical cystoprostatectomy specimen reported a relatively higher rate of extra capsular extension (20%) and Gleason grade 4 (21%) than previously noted (3-11%) [14]. We found evidence of diffuse HGPIN in 10 out of 14 patients (71%) with incidental carcinoma prostate. There was only one radical cystoprostatectomy specimen with diffuse HGPIN without any evidence of incidental CaP. In the study by Wiley et al., incidental PC was found in 22 of 48 cystoprostatectomy cases and HGPIN was found in 21 (95%) of these 22 cases. Conversely, there was only one incidental PC in the eight prostates without HGPIN (13%). They concluded that HGPIN is a marker for concurrent PC, and that the risk depends more on the volume of HGPIN than on its absolute presence [15].
The present results indicate that the percentage of incidentally detected prostate cancer in cystoprostatectomy specimens at our clinical center is much lower (12.5%) than reported rates in the world until now (25-68%). We assumed that the varying methods of histopathological examination of the prostate could be the main cause of these frequency differences. Also, regional differences in prostate cancer incidence rates can be related to environmental and racial factors. The clinical significance of these incidentally discovered cancers remain questionable because the outcome of the patients with both malignancies depends on the prognosis of the bladder tumor. None of the patients in our study showed evidence of progression on follow up. Node positive incidental CaP remained in remission following hormone therapy.
Limitation
The retrospective nature and small sample size are the main drawbacks of our study. A longer follow up period of patients with incidental carcinoma prostate would have given a better understanding of the natural history of these tumours.
Conclusion
The percentage of incidentally detected prostate cancer in cystoprostatectomies varies in different studies. This can be attributed to sampling techniques and possibly environmental and racial factors. The clinical significance of incidental prostate cancer is doubtful and prognosis depends on the aggressiveness of bladder tumour. It would be prudent to do digital rectal examination (for clinical prostate evaluation) and prostate-specific antigen (PSA) testing along with bladder cancer work.
UB: Urinary bladder; GS: Gleason score; CaP: Carcinoma prostate; HGPIN: High grade prostate intraepithelial neoplasm; RC: Radical cystectomy; ONB: Orthotopic neobladder; IC: Ileal conduit; CU: Cutaneous ureterostomy; CT: Chemotherapy; PSA: Prostate specific antigen; NA: Non applicable**After surgery
HGPIN: High grade prostate intraepithelial neoplasm; ASAP: Atypical small acinar proliferation; RC: Radical cystectomy; ONB: Orthotopic neobladder; IC: Ileal conduit, CT: Chemotherapy