Benzodiazepine Induced Acute Pancreatitis
Poornima Sangmeshwar Tadkal1, Nithin Bhat2, Manjunatha Hande3
1 Junior Resident, Department of General Medicine, Kasturba Medical College, Manipal, Udupi, Karnataka, India.
2 Assistant Professor, Department of General Medicine, Kasturba Medical College, Manipal, Udupi, Karnataka, India.
3 Professor, Department of General Medicine, Kasturba Medical College, Manipal, Udupi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Poornima Sangmeshwar Tadkal, Medicine OPD, 2nd floor, OPD building, Kasturba Hospital, Manipal-576104, Udupi, Karnataka, India.
E-mail: tadkalpoornima29@gmail.com
Acute pancreatitis is acute inflammation of pancreas, caused mainly due to alcohol and gall stones. Drug induced pancreatitis is rare and benzodiazepine induced pancreatitis is still rare. Drug induced pancreatitis is a diagnosis of exclusion. We present a case of 64-year-old female, taking benzodiazepines for her disturbed sleep, admitted to the hospital with pain abdomen. Evaluation showed that she was suffering from acute pancreatitis, which was most likely secondary to her benzodiazepine intake. A high index of clinical suspicion and good drug history helped in diagnosing the cause of pancreatitis.
Abdomen, Drug induced pancreatitis, Pain
Case Report
A 64-year-old female with no history of premorbidities, complained of upper abdominal pain since one day, dull aching in nature with radiation to the back. Next day when her family members tried to wake her up, she was drowsy and complained of pain in the abdomen. She was brought to the emergency room of our hospital.
On examination, pulse rate was 78 beats/min, Blood Pressure (BP)-110/80 mmHg, SpO2-98% on room air. Central Nervous System examination- Glasgow Coma Scale (GCS) was E3 V4 M5. No obvious motor or sensory deficit was noted. Per abdomen examination showed presence of tenderness in umbilical region, no free fluid, bowel sounds present. Other systems were normal on examination.
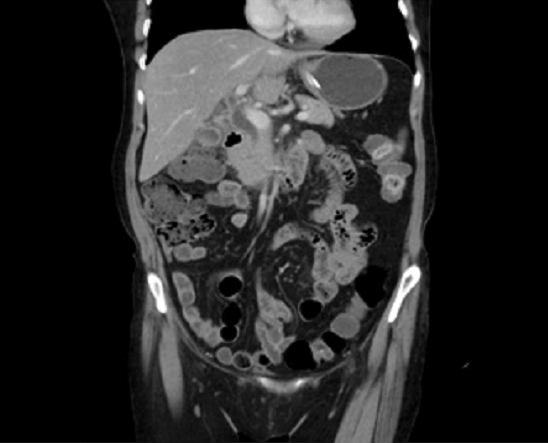
In view of her altered sensorium, cerebrovascular accident or electrolyte imbalance was suspected. To rule out cerebrovascular accident, Computrised Tomography (CT) brain was done which was normal. Later Magnetic Resonance Imaging (MRI) brain was done that was also normal. Renal function test and serum electrolytes were also normal [Table/Fig-1]. In view of pain abdomen, ultrasound abdomen was done, which showed bulky pancreas with heterogenous echotexture suggestive of acute pancreatitis, normal gall bladder. Serum amylase and lipase done were elevated. Contrast Enhanced Computerised Tomography (CECT) Abdomen done was suggestive of acute pancreatitis [Table/Fig-2,3].
Laboratory parameters at admission and after 5 days of hospital stay.
| Lab Parameters | At Admission | After 5 Days |
|---|
| Serum Urea | 18 mg/dL | 17 mg/dL |
| Serum Creatinine | 0.6 mg/dL | 0.7 mg/dL |
| Serum Sodium | 135 mmol/L | 138 mmol/L |
| Serum Potassium | 4.4 mmol/L | 4.2 mmol/L |
| Serum Amylase | 560 U/L | 62 U/L |
| Serum Lipase | 1060 U/L | 68 U/L |
| Serum Triglyceride | 59 mg/dL | - |
| Fasting Blood Sugar | 81mg/dL | |
| HbA1c | 5.7% | - |
| Haemoglobin | 12.5 gm/dL | 12.6 gm/dL |
| WBC count | 7.4 *103/microltr | 8.4*103/ microltr |
| Platelet count | 2.21 lac/dL | 2.65 lac/dL |
| Blood culture | Sterile | Sterile after 5 days |
| Serum calcium | 8.6 mg/dL | |
| HIV/Hep C/Hep B | negative | |
CECT abdomen axial plane showing enlarged head of pancreas.

CECT abdomen sagittal section showing enlarged and bulky pancreas suggestive of pancreatitis.
Patient was evaluated to know the cause of pancreatitis. She had no history of alcohol consumption or smoking, steroid intake, history of trauma, instrumentation or surgery. Presently her blood glucose levels were normal. Infective cause was ruled out as total white blood cell count was normal, blood culture was sterile and no foci of infection were found. Fasting lipid profile was also normal [Table/Fig-1].
Possibility of drug induced pancreatitis was considered after ruling out other causes. So patient was interviewed for any history of drug intake and she revealed that due to some quarrel in the house and disturbed sleep, she has been taking sleeping pills (name of the drug she does not know) since last one month and since last 3-4 days she has been taking 4-5 tablets per day. Her urine was sent to toxicology centre for drug testing and was found positive for benzodiazepine. NARANJO causality score calculated in our patient was 7 suggestive of pancreatitis as a probable adverse drug effect of benzodiazepines. WHO-UMC causality assessment done for this patient was suggestive of a probable/likely relationship between the drug.
The patients was treated conservatively for acute pancreatitis. Repeat serum amylase and lipase done after five days were decreased, compared to her initial enzyme levels [Table/Fig-1]. Patient improved and she was discharged from hospital after seven days of hospital stay.
The patients was referred to Psychiatry in view of her dependence on sleeping pills, psychological counselling done and she was put on fluoxetine for her psychotic symptoms.
Discussion
Drug induced acute pancreatitis is rare, amounting to only 0.1-2% of cases. Drugs commonly known to cause are azathioprine, 6 mercaptopurine, sulphonamides etc. [1].
Benzodiazepines causing pancreatitis is rare. In the present case, patient was diagnosed with acute pancreatitis secondary to unknown benzodiazepine drug intake.
Benzodiazepines are used as sedatives and to treat anxiety, disturbances of sleep, seizures and withdrawal disorders. Benzodiazepines act by binding to GABA receptors. This binding increases the flow of chloride ions through the GABA ion channel, causing postsynaptic hyperpolarization and a decreased ability to initiate an action potential [2].
Till date, only one cohort study has been done on benzodiazepine induced acute pancreatitis in Taiwan from 2010 to 2011 involving 12,893 patients where the results showed that the patients with benzodiazepine poisoning had a 5.33-fold increased risk of acute pancreatitis compared with the controls without benzodiazepine poisoning [3]. The exact mechanism of benzodiazepine induced pancreatitis is not known. However, zolpidem a non benzodiazepine hypnotic is reported to cause pancreatitis [4]. Zolpidem acts similar to benzodiazepines, by acting selectively on alpha1 subunit-containing GABA benzodiazepine receptors. In contrast to zolpidem, benzodiazepines have greater affinity for GABA subunits, so may be benzodiazepine overdose also increases the risk of acute pancreatitis in the same way. Olanzapine, an atypical antipsychotic belonging to thienobenzodiazepine class, is known to cause pancreatitis, though the mechanism is unclear. Olanzapine induced impaired glucose tolerance, direct pancreatic injury and hypertriglyceridemia are believed to have caused pancreatitis [5,6]. There are no specific or distinguishing clinical features to diagnose drug induced pancreatitis. The diagnosis is based on high index of suspicion and careful drug history.
Conclusion
Benzodiazepine induced pancreatitis is rare. It is a diagnosis of exclusion. A high index of suspicion and good clinical history taking is needed. Through this case report, we emphasize on importance of good history taking, which had directed us towards the diagnosis.
[1]. Jones MR, Hall OM, Kaye AM, Kaye AD, Drug-induced acute pancreatitis: a reviewThe Ochsner Journal 2015 15(1):45-51. [Google Scholar]
[2]. Hevers W, Lüddens H, The diversity of GABAA receptors. Pharmacological and electrophysiological properties of GABAA channel subtypesMolecular Neurobiology 1998 18(1):35-86.10.1007/BF027414599824848 [Google Scholar] [CrossRef] [PubMed]
[3]. Liaw GW, Hung DZ, Chen WK, Lin CL, Lin IC, Kao CH, Relationship between acute benzodiazepine poisoning and acute pancreatitis risk: a population-based cohort studyMedicine 2015 94(52):e237610.1097/MD.000000000000237626717383 [Google Scholar] [CrossRef] [PubMed]
[4]. Lai SW, Lin CL, Liao KF, Increased relative risk of acute pancreatitis in zolpidem usersPsychopharmacology 2015 232(12):2043-48.10.1007/s00213-014-3833-625491930 [Google Scholar] [CrossRef] [PubMed]
[5]. Kerr TA, Jonnalagadda S, Prakash C, Azar R, Pancreatitis following olanzapine therapy: a report of three casesCase Reports in Gastroenterology 2007 1(1):15-20.10.1159/00010422221487466 [Google Scholar] [CrossRef] [PubMed]
[6]. Samantha M, Roy-Chaudhury P, Yadlapalli G, Olanzapine-induced hypertriglyceridemia resulting in necrotizing pancreatitisACG Case Reports Journal 2016 3(4):e10410.14309/crj.2016.7727807566 [Google Scholar] [CrossRef] [PubMed]