Primary Ewings Sarcoma of Kidney: A Case Report
Krishnendu Maiti1, Akash Agrawal2, Chhanda Datta3, Dilip Kumar Pal4
1 Assistant Professor, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
2 Post Doctrol Trainee, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
3 Professor and Head, Department of Pathology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
4 Professor and Head, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dilip Kumar Pal, 244, AJC, Bose Road, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata-700020, West Bengal, India.
E-mail: urologyipgmer@gmail.com
Primary Ewings Sarcoma (EWS) of the kidney is a very rare tumour and very few cases have been reported till date. We present a case of a 36-year-old lady presenting to us with flank pain and haematuria, with a huge renal mass. Following left radical nephrectomy, histopathology was reported as ewings sarcoma. Hence, while dealing with renal masses in young patients, this entity should always be kept in mind.
Genitourinary mesenchymal tumour, Renal mesenchymal tumour, Renal tumour
Case Report
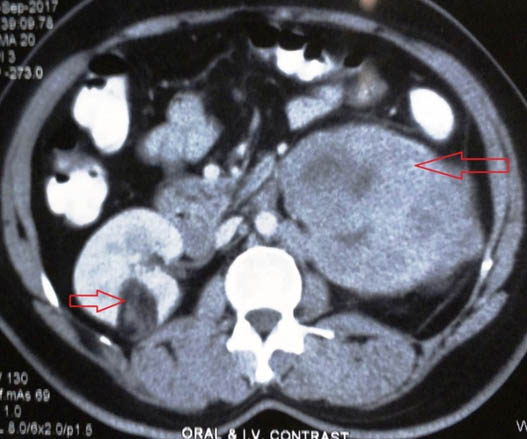
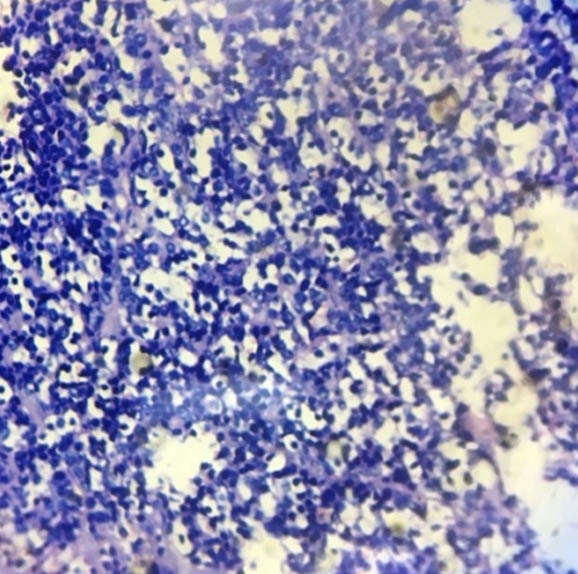
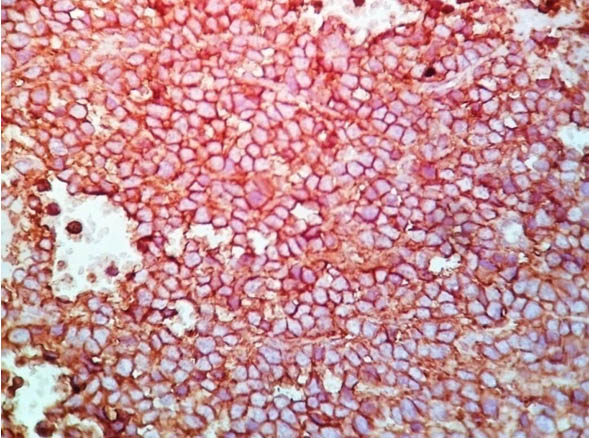
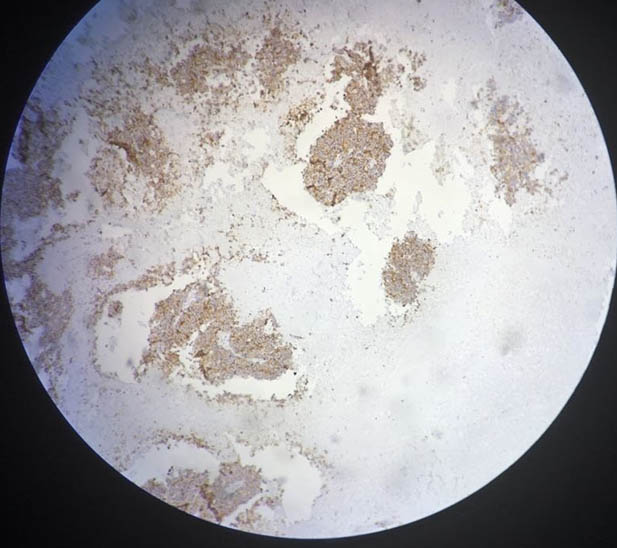
A 36-year-old women housewife by occupation presented to us with colicky pain in the left flank since two month duration which was relieved with use of analgesics. She had intermittent haematuria for the same duration. Her medical history was unremarkable except that the patient was known hypertensive which was controlled with the use of regular medication. On physical examination, there was a mass occupying the left hypochondriac and lumbar region moving with respiration, bimanually palpable and ballotable. All the routine blood investigations including serum creatinine were normal. Chest X-ray was non-contributory. On ultrasonography there was an Ill defined mixed echogenic space occupying lesion, 79×71 mm in lower aspect of left kidney. There was another well defined hyperechoic space occupying lesion, about 33 mm in diameter near mid part of Right kidney probably an Angiomyolipoma (AML). On contrast enhanced CT, there was a large heterogenously enhancing soft tissue mass of size 82×70×68 mm (H.U. Enhancement from 39 to 56) seen involving left kidney. Thrombus was noted in the proximal part of left renal vein. Fascial planes were lost at places with thickening of renal capsule. Also, there was a mixed density space occupying lesion in right kidney having fat and soft tissue component probably an AML [Table/Fig-1]. Left radical nephrectomy along with hilar lymph nodes were undertaken with an uneventful recovery. On gross pathologic examination there was a tumour of 10x10x8 cm, mostly involving lower pole of left kidney, with variegated cut surface. Macroscopic extension was limited to the renal parenchyma. Histological features of tumour composed of small round cells with rounded nuclei and scanty cytoplasm. The cells were arranged in sheets and cohesive lobules and shows rosettes and perivascular pseudorosettes [Table/Fig-2]. Histologic type was confirmed to be as Ewings sarcoma of the kidney. All the margins were uninvolved including gerotas fascia and renal vein lymphovascular invasion was present. Immunohistochemistry was done which showed that CD99 was strongly positive in tumour cells [Table/Fig-3]. Synaptophysin was also positive [Table/Fig-4] and leukocyte common antigen was negative in tumour cells. She was on adjuvant etoposide-based chemotherapy. Presently, she is doing well till 6 months after surgery.
CECT showing Angiomyolipoma in right kidney and heterogeneously enhancing mass in left kidney.
H&E low magnification (10X).
CD99 strongly positive in tumour cells (40X).
Synaptophysin positive in tumour cells (4X).
Discussion
EWS of the kidney is a rare tumour in adults. It was first described by Seemayer and colleagues [1]. Only very few cases of primary EWS have been reported in the literature till date [2-4]. Primary renal EWS diagnosis can be difficult and is based on a combination of electron microscopy, Immunohistochemistry (IHC), chromosomal analysis, Fluorescence In Situ Hybridization (FISH) and light microscopy.
Primary Ewings sarcoma of the kidney is a rare entity. Sources of renal EWS include neural cells that invaginate into the kidney during development [5]. Other authors theorize that embryonic neural cells migrate into the kidney and undergo tumourigenesis. Hakky et al., in their case report and meta-analysis have described acute flank pain mimicking renal colic as the most common presentation of EWS of the kidney [6]. Our patient also presented with flank pain of short duration which support their finding. Renal EWS is found in young adults. Median age of diagnosis of peripheral PNET is 24 years with a range of 10-39 years [7]. Our patient in above case is also 36 years of age. The most diagnostically useful histologic feature of these tumours is the arrangement of the tumour cells into pseudorosettes, clusters of cells with a neurofibrillary stromal core, which serve to indicate neural differentiation. Bing et al., concluded that under microscopy EWS forms spherical grouping of dark tumour cells around a central area that contains neurofibrils called Homer–Wright rosettes, as we also found in our case [4]. According to Alava et al., Cell surface expression of the glycoprotein CD99 (MIC2) is detected in 95% of cases of ESFT, making this a highly sensitive, albeit nonspecific, marker for these tumours. The cytogenetics play an important role in confirming the diagnosis, by localizing the translocation t (11:22) (q24; q12) resulting in the production of the EWS/FLI-1 fusion [8]. Le Deley et al., stated that, in contrast to retrospective studies, the prospective evaluation did not confirm a prognostic benefit for type 1 EWS-FLI1 fusions [9]. There is no consensus regarding the treatment of renal EWS. Most cases have been treated with surgical resection with adjuvant chemotherapy. The effective chemotherapy agents are vincristine, doxorubicin, ifosfamide, etoposide, actinomycin D and cyclophosphamide. Addition of ifosfamide and etoposide to doxorubicin containing regimens confers survival advantage in patients with non-metastatic disease [10]. Postoperative radiotherapy must be added in the case of inadequate surgical margins [7]. In a retrospective study, 31% patients had metastasis. The most common site of metastasis was the lung, followed by the liver and bone. Despite aggressive treatment, prognosis remains poor and the median survival was reported at 15 months [11]. Five year survival rate was found to be 45% to 55% for peripheral PNET tumours localized to the kidney [7].
Conclusion
Primary ewing’s sarcoma is a rare entity in kidney presenting only in <1% of solid tumours. Primary EWS should be considered as a differential diagnosis in young individuals presenting with a renal mass. Diagnosis requires histopathology, IHC and cytogenetics. Diagnosis of sarcoma should be kept in mind as prognosis is overall poor and resection of other viscera may be required if it is extending. Surgical resection with adjuvant chemotherapy is the treatment of choice.
[1]. Seemayer TA, Thelmo WL, Bolande RP, Wiglesworth FW, Peripheral neuroectodermal tumoursPerspect Pediatr Pathol 1975 2:151-72. [Google Scholar]
[2]. Saxena R, Sait S, Mhawech-Fauceglia P, Ewing sarcoma/ primitive neuroectodermal tumour of the kidney: a case report. Diagnosed by immunohistochemistry and molecular analysisAnn Diagn Pathol 2006 10:363-66.10.1016/j.anndiagpath.2005.11.00117126256 [Google Scholar] [CrossRef] [PubMed]
[3]. Kang SH, Perle MA, Nonaka D, Zhu H, Chan W, Yang GC, Primary Ewing sarcoma/PNET of the kidney: fine needle aspiration, histology, and dual color break apart FISH AssayDiagn Cytopatholy 2007 35:353-57.10.1002/dc.2064217497665 [Google Scholar] [CrossRef] [PubMed]
[4]. Bing Z, Zhang P, Tomaszewski J, MacLennan G, Primary ewing sarcoma/primitive neuroectodermal tumour of the kidneyThe Journal of Urology 2009 181(3):1341-42.10.1016/j.juro.2008.12.02919157457 [Google Scholar] [CrossRef] [PubMed]
[5]. Parham DM, Roloson GJ, Feely M, Green DM, Bridge JA, Beckwith JB, Primary malignant neuroepithelial tumours of the kidney: a clinicopathologic analysis of 146 adult and pediatric cases from the National Wilms’ Tumour Study Group Pathology CenterAm J Surg Pathol 2001 25:133-46.10.1097/00000478-200102000-0000111176062 [Google Scholar] [CrossRef] [PubMed]
[6]. Hakky TS, Gonzalvo AA, Lockhart JL, Rodriguez AR, Primary Ewing sarcoma of the kidney: a symptomatic presentation and review of the literatureTher Adv Urol 2013 5(1):153-59.10.1177/175628721247109523730330 [Google Scholar] [CrossRef] [PubMed]
[7]. Ellinger J, Bastian P, Hauser S, Biermann K, Müller S, Primitive neuroectodermal tumour: Rare, highly aggressive differential diagnosis in urologic malignanciesUrology 2006 68(2):257-62.10.1016/j.urology.2006.02.03716904430 [Google Scholar] [CrossRef] [PubMed]
[8]. De Alava E, Gerald WL, Molecular biology of the Ewing’s sarcoma/primitive neuroectodermal tumour familyJ Clin Oncol 2000 18(1):204-13.10.1200/JCO.2000.18.1.20410623711 [Google Scholar] [CrossRef] [PubMed]
[9]. Le Deley M, Delattre O, Schaefer K, Burchill S, Koehler G, Hogendoorn P, Impact of EWS-ETS fusion type on disease progression in ewing’s sarcoma/peripheral primitive neuroectodermal tumour: prospective results from the cooperative euro-E.W.I.N.G. 99 trialJournal of Clinical Oncology 2010 28(12):1982-88.10.1200/JCO.2009.23.358520308673 [Google Scholar] [CrossRef] [PubMed]
[10]. Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumour of boneN Engl J Med 2003 348:694-701.10.1056/NEJMoa02089012594313 [Google Scholar] [CrossRef] [PubMed]
[11]. Thyavihally YB, Tongaonkar HB, Gupta S, Kurkure PA, Amare P, Muckaden MA, Primitive neuroectodermal tumour of the kidney: a single institute series of 16 patientsUrology 2008 71:292-96.10.1016/j.urology.2007.09.05118308106 [Google Scholar] [CrossRef] [PubMed]