Atypical Intra-Bronchial Carcinoid -A Rare Case Report
Malgere R Ramitha1, Gajanan S Gaude2
1 Senior Resident, Department of Pulmonary Medicine, J. N. Medical College, Belgaum, Karnataka, India.
2 Professor and Head, Department of Pulmonary Medicine, J. N. Medical College, Belgaum, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gajanan S Gaude Nehrunagar, Belgaum, Karnataka, India.
E-mail: gsgaude922@gmail.com
Bronchial carcinoids are uncommon, slow growing; low-grade malignant neoplasms of the lungs, which rarely metastasize outside the thoracic cavity. We hereby report a case of atypical intra-bronchial carcinoid tumour of the lung in a young female which was treated successfully with surgery and chemotherapy.
Atypical carcinoids, Carcinoid tumour, Lungs, Neuroendocrine tumours, Typical carcinoids
Case Report
A 29-year-old female patient presented with breathlessness of six months duration which was gradually progressive and aggravated on exertion. There was no history of orthopnoea, and no diurnal variation or seasonal variation in breathlessness. There was also history of continuous dull aching chest pain since for six months, which was on right side, with no radiation of pain. There was no history of fever, cough, expectoration, haemoptysis, vomiting, sweating or joint pain. There was no history of diabetes, hypertension, thyroid disorders, tuberculosis or bronchial asthma in the past.
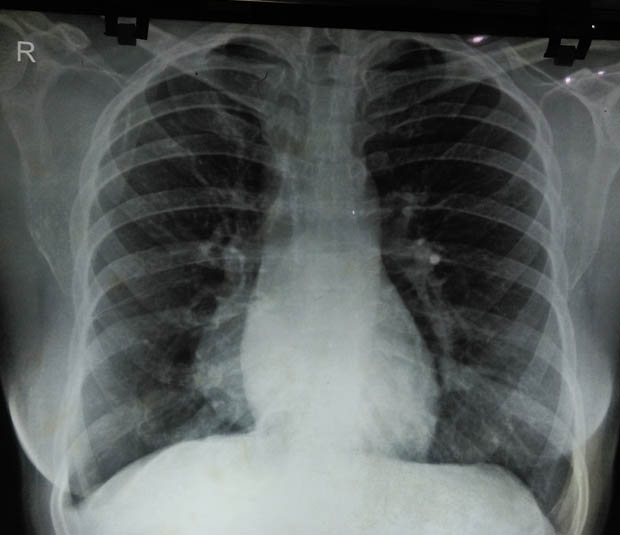
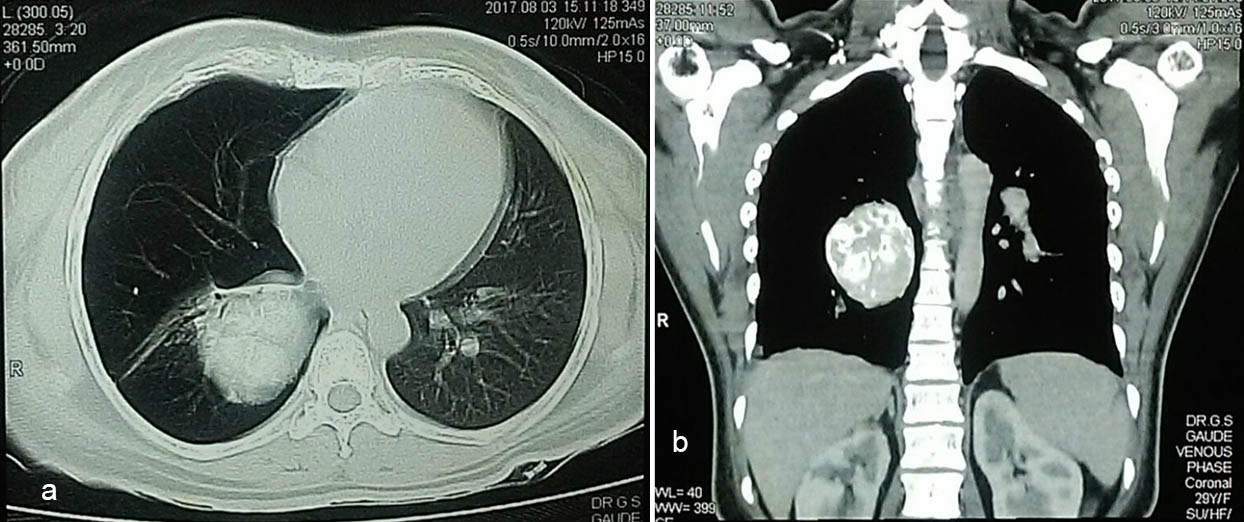
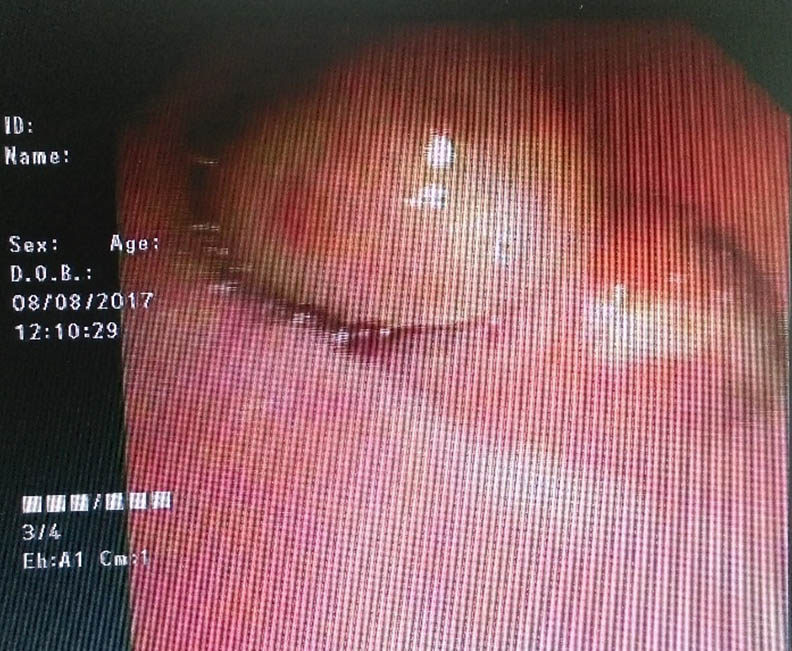
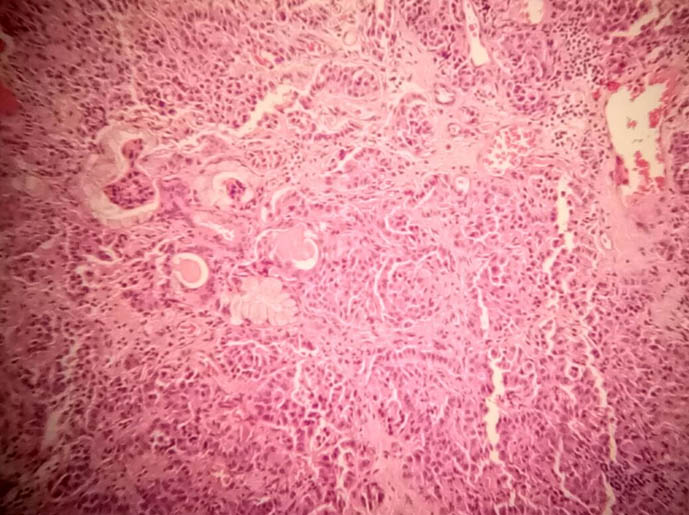
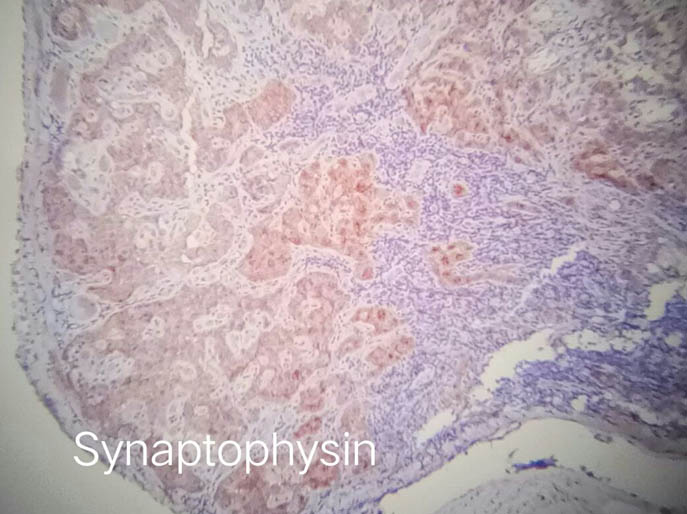
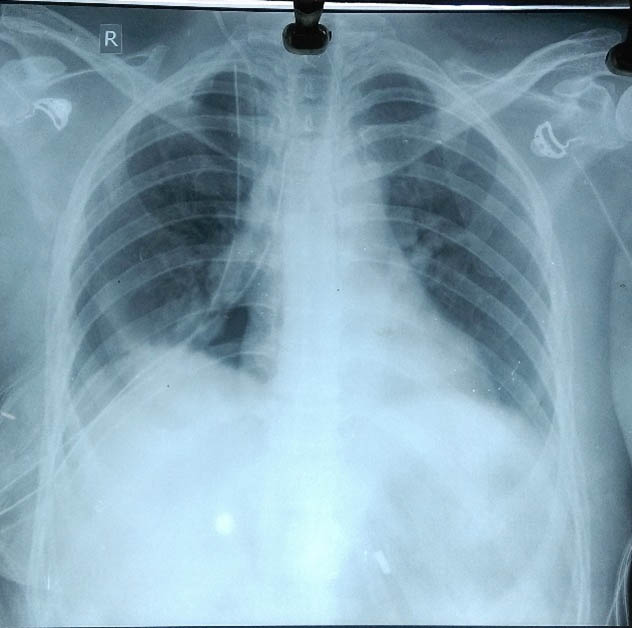
On examination, vitals were stable with pulse rate of 82/min, respiratory rate of 20/min, blood pressure-110/70 mmHg and the patient was afebrile. There were no signs of pallor, icterus, clubbing, cyanosis, lymphadenopathy or oedema. Respiratory system examination revealed dull note in right inframammary area with reduced vocal resonance. There were tubular breath sounds in mammary and inframammary areas on the right side. Blood examination were within normal limits. Chest radiograph revealed homogenous opacity in right lower zone in paracardiac region [Table/Fig-1]. Computed Tomography (CT) Thorax revealed a well-defined soft tissue density involving right bronchus intermedius with extension into right lower lobe and sub-carinal lymphnodes [Table/Fig-2a,b]. Video bronchoscopy revealed a large mass completely obstructing bronchus intermedius which appeared glossy with smooth margins. There were some specks of calcification visible [Table/Fig-3]. Biopsy of the mass showed tumour cells showing scanty to moderate cytoplasm and round monomorphic nuclei with stripped chromatin which was consistent with neuroendocrine tumour (WHO Grade 1) [Table/Fig-4]. Immunohistochemistry of the biopsy specimen revealed synaptophysin, and chromogranin positive and Ki 67 negative [Table/Fig-5,6]. The diagnosis was confirmed as bronchial carcinoid. The patient was subjected for surgical resection of the tumour. On thoracotomy, it was observed that the tumour was adherent to the mediastinum and dissection was done with excision of mediastinal adhered lymph nodes and right middle lobe and right lower lobe lobectomy en block [Table/Fig-7]. Histopathology of the resected tumour confirmed the diagnosis of the central carcinoid tumour with intermediate malignant potential and mediastinal lymph node involvement. Postoperatively her lung expanded completely [Table/Fig-8]. The patient was advised for chemotherapy in the view of malignant deposits in the mediastinal lymph nodes. The patient received chemotherapy with cisplatin-100mg/m2 on day 1and etoposide-35 mg/m2 for four days as one cycle. She received four cycles of this chemotherapy and she is doing well.
Chest radiograph showing right para-cardiac homogenous opacity.
Computed Tomography (CT) of the chest showing well defined mass in right paracardiac region with calcifications.
Video-bronchoscopy shows a large mass completely obstructing bronchus intermedius which was glossy with smooth margins.
Biopsy of the mass showed tumour cells showing scanty to moderate cytoplasm and round monomorphic nuclei with stipped chromatin (Haematoxylin and Eosin stain X100).
Immunohistochemistry of the biopsy specimen revealed Synaptophysin (20X Magnification).
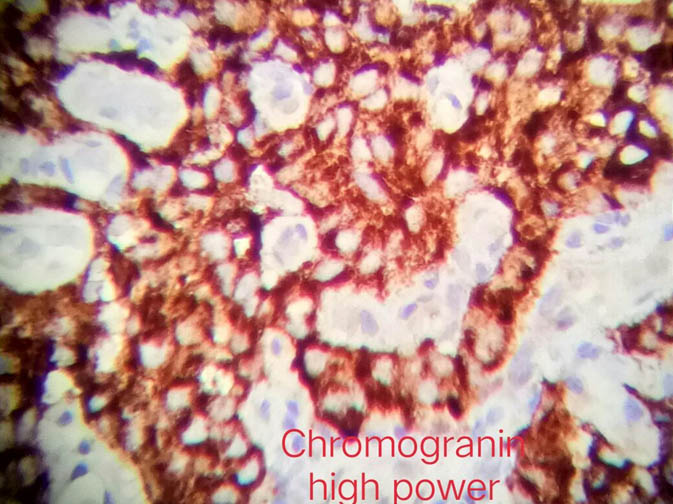
Immunohistochemistry of the biopsy specimen revealed chromogranin (40X Magnification).

Postoperative chest radiograph showing complete expansion of right lung.
Discussion
Neuroendocrine Tumours (NETs) comprise a heterogeneous group of malignancies that arise from neuroendocrine cells throughout the body, most commonly originating from the gastrointestinal tract and lungs. Lung NETs can be classified as well differentiated {low-grade Typical Carcinoids (TCs) and intermediate-grade Atypical Carcinoids (ACs)} and poorly differentiated (high-grade large cell neuroendocrine carcinoma or SCLC) [1]. Carcinoid tumours account for 0.5-2.5% of all primary lung tumours and they are slow growing and low-grade malignant tumours [2].
More than 80% of lung NETs are carcinoids [3]. They synthesise and secrete neuroendocrine peptides into the general circulation and they have the ability to synthesise serotonin from dietary tryptophan, which is suggested to be pathognomonic of carcinoids. The symptoms of bronchial carcinoids depend on the location of the tumour-central or peripheral. Central tumours are mostly located in the right lung and cause haemoptysis or recurrent bronchial obstruction as noted in the present case. In symptomatic patients, the most common clinical findings are those associated with bronchial obstruction, such as persistent cough, haemoptysis, and recurrent or obstructive pneumonitis. Wheezing, chest pain, and dyspnoea also may be noted [4]. Although, uncommon, various endocrine or neuroendocrine syndromes can be initial clinical manifestations of either typical or atypical pulmonary carcinoid tumours. Carcinoid syndrome, hypercortisolism and Cushing syndrome, inappropriate secretion of Antidiuretic Hormone (ADH), increased pigmentation secondary to excess Melanocyte-Stimulating Hormone (MSH), and ectopic insulin production resulting in hypoglycaemia are some of the endocrinopathies that can be produced by a pulmonary carcinoid tumour in a patient who is otherwise asymptomatic [5].
Endocrine manifestations occur in 1-7% of cases including the carcinoid syndrome, which occurs in 86% of patients with liver metastases [2]. Our case did not have carcinoid syndrome. Carcinoid tumours may present as “iceberg-like lesion”, with a small amount of endobronchial growth and a prominent parenchymal mass [6].
Our case had right main stem central obstruction due to the tumour. The main symptoms in our case were chest pain and breathlessness. There were no symptoms of carcinoid syndrome in our case.
Histopathologically, they are classified as TCs and ACs. Typical carcinoids account for about 9 out of 10 lung carcinoids. They grow slowly and rarely spread beyond the lungs. Atypical carcinoids are much rarer than typical lung carcinoids. They tend to grow faster than typical carcinoids. There is a greater chance that they will spread (metastasize) beyond the lungs. They have increased mitotic activity and necrosis [7].
Of the many histopathologic techniques available, immune-histochemistry is considered to be the most sensitive and accurate in distinguishing TCs and ACs [2]. Our patient was a case of atypical carcinoid tumour since it had malignant potential with metastasis to regional lymph nodes. Also, microscopically it showed increased mitotic activity.
Surgery is the standard treatment for stage I-II and most stage III, which accounts for 75% and 15% respectively [8]. Combination of everolimus plus octreotide may represent the best option. The most significant prognostic factor is the histopathological subtype, because 5-years survival rate of typical and atypical carcinoids are 87% to 98% and 56%-73%, respectively [3]. Carcinoid tumours of the lung generally have a better prognosis than other forms of pulmonary malignancy. They have an overall 5-year survival rate of 78-95% and a 10-year survival rate of 77-90% [9]. Typical carcinoid tumours have been found to have a much better prognosis than do the atypical variety [10]. Atypical carcinoid tumours have been associated with a 5-year survival rate of 40-60% and a 10-year survival rate of 31-60%, depending on the series. Garcia-Yuste et al., has observed that the mediastinal nodal involvement and histological sub-type as the most important factors influencing the prognosis in these patients [11]. A study conducted by Ducrocq et al., examined factors determining long-term survival after resection of typical carcinoid tumours [12]. It failed to demonstrate any prognostic significance for sex, tumour size (T1 versus T2), tumour location (central versus peripheral), and type of resection. The study confirms a good prognosis after complete resection of typical carcinoid tumours, including those with lymph node metastasis. The main prognostic factors are histology (with a significantly higher survival for typical carcinoid tumours), lymph node, and metastasis [13].
Conclusion
In conclusion, diagnosis of bronchial carcinoids is often overlooked in young patients in the absence of specific symptoms. The present case demonstrated that the bronchial carcinoid can present in young adults, and with early diagnosis and surgery, the patient can be cured of the disease.
Financial or Other Competing Interests
None.
Consent was Obtained from Patient for Publishing the Case Report.
[1]. Hendifar A, Marchevsky A, Tuli R, Neuroendocrine tumors of the lung: current challenges and advances in the diagnosis and management of well-differentiated diseaseJ Thoac Onco 2016 12(3):425-36.10.1016/j.jtho.2016.11.222227890494 [Google Scholar] [CrossRef] [PubMed]
[2]. Bora M, Vithiavathi S, Primary bronchial carcinoid: A rare differential diagnosis of pulmonary koch in young adult patientLung India 2012 29(1):59-62.10.4103/0970-2113.9236622345917 [Google Scholar] [CrossRef] [PubMed]
[3]. Girard N, Cadranel J, Brambilla E, Cordier J, Rare Primary Lung Tumors. In: Murray and Nadel’s Textbook of Respiratory Medicine (Editors) Broaddus VC, Mason RJ, Ernst JE, King Jr TE, Lazarus SC, Murray JF, et al 2016 6th EditionLondonElsevier Publ.:965-79980.10.1016/B978-1-4557-3383-5.00054-3 [Google Scholar] [CrossRef]
[4]. Han B, Sun JM, Ahn JS, Park K, Ahn AJ, Clinical outcomes of atypical carcinoid tumors of the lung and thymus: 7-year experience of a rare malignancy at single instituteMed Oncol 2013 30(1):479-81.10.1007/s12032-013-0479-x23377986 [Google Scholar] [CrossRef] [PubMed]
[5]. Kunz P, Carcinoid and neuroendocrine tumors: building on successJ Clin Oncol 2015 33(16):1855-63.10.1200/JCO.2014.60.253225918282 [Google Scholar] [CrossRef] [PubMed]
[6]. Zhong CX, Yao F, Zhao H, Shi JX, Fan LM, Long-term outcomes of surgical treatment for pulmonary carcinoid tumors: 20 years’ experience with 131 patientsChin Med J (Engl) 2012 125(17):3022-36. [Google Scholar]
[7]. Kulke M, Benson A, Bergsland E, Berlin J, Blaszkowsky L, Choti M, Neuroendocrine TumorsJ Natl Compr Canc Netw 2012 10(6):724-64.10.6004/jnccn.2012.007522679117 [Google Scholar] [CrossRef] [PubMed]
[8]. Machuca TN, Cardoso PF, Camargo SM, Surgical treatment of bronchial carcinoid tumors: a single-center experienceLung Cancer 2010 70(2):158-62.10.1016/j.lungcan.2010.01.01520223552 [Google Scholar] [CrossRef] [PubMed]
[9]. Cao C, Yan TD, Kennedy C, Hendel N, Bannon PG, McCaughan BC, Bronchopulmonary carcinoid tumors: long-term outcomes after resectionAnn Thorac Surg 2011 91(2):339-43.10.1016/j.athoracsur.2010.08.06221256263 [Google Scholar] [CrossRef] [PubMed]
[10]. Brambilla E, Travis W, Colby T, Corrin B, Shimosato Y, The new World Health Organization classification of lung tumoursEur Respir J 2001 18(6):1059-68.10.1183/09031936.01.0027530111829087 [Google Scholar] [CrossRef] [PubMed]
[11]. García-Yuste M, Matilla JM, Cueto A, Paniagua JM, Ramos G, Cañizares MA, Typical and atypical carcinoid tumours: Analysis of the experience of the Spanish multi-centric study of neuroendocrine tumours of the lungEur J Cardio-Thorac Surg 2007 31(2):192-97.10.1016/j.ejcts.2006.11.03117196822 [Google Scholar] [CrossRef] [PubMed]
[12]. Ducrocq X, Thomas P, Massard G, Barsotti P, Giudicelli R, Fuentes P, Operative risk and prognostic factors of typical bronchial carcinoid tumorsAnn Thorac Surg 1998 65(5):1410-14.10.1016/S0003-4975(98)00083-6 [Google Scholar] [CrossRef]
[13]. Hindié E, The NETPET Score: Combining FDG and Somatostatin receptor imaging for optimal management of patients with metastatic well-differentiated neuroendocrine tumorsTheranostics 2017 7(5):1159-63.10.7150/thno.1958828435455 [Google Scholar] [CrossRef] [PubMed]