Flexor Digitorum Profundus Irritation and Pseudotumour Formation Ten Years after a Penetrating Glass Injury
Baris Polat1, Deniz Aydin2, Mehmet Alp Dirik3, Ali Caygur4, Ayse Esin Polat5
1 Department of Orthopaedics and Traumatology, Near East University, Lefkoşa, Cyprus.
2 Department of Orthopaedics and Traumatology, Near East University, Lefkoşa, Cyprus.
3 Department of Radiology, Dr. Suat Günsel Kyrenia University, Girne, Cyprus.
4 Department of Orthopaedics and Traumatology, Dr. Burhan Nalbantoğlu State Hospital, Lefkoşa, Cyprus.
5 Department of Orthopaedics and Traumatology, Dr. Akçiçek State Hospital, Girne, Cyprus.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Baris Polat, Department of Orthopaedics and Traumatology, Near East University, Lefkoşa, Cyprus.
E-mail: drbpolat@hotmail.com
Retained foreign bodies inside the soft tissue following penetrating injuries are common. Late onset of symptoms and complications are possible in these cases. In the present report, we present a case of late flexor digitorum profundus irritation and pseudotumour formation caused by a retained glass piece 10 years after the injury. Pseudotumour is formed by reaction to the retained material as an enlarged portion of tissue that resembles a tumour. The complaints were completely improved soon after removal of the foreign material. Retained soft tissue foreign bodies should be suspected in differential diagnosis of soft tissue masses. History of a penetrating trauma should be questioned persistently. The authors recommend the removal of retained foreign bodies with sharp edges to avoid further injury to the surrounding anatomical structures.
Forearm mass, Retained foreign body, Volar wrist pain, Wrist swelling
Case Report
A 35-year-old male construction worker presented with increasing pain and swelling at the right distal volar forearm and flexion position of the 4th and 5th finger with pain during passive extension for a period of three weeks. He did not report any trauma but had recently changed his job to become a plasterer which involved repetitive flexion-extension movements of the wrist.
A 3×5 cm sized, tender, nonfluctuating swelling was palpated in his right distal volar forearm. There was no systemic inflammation but mild local inflammation was seen on examination. There was no wound scar over the swelling. The Metacarpophalangeal (MCP), Distal Interphalangeal (DIP) and Proximal Interphalangeal (PIP) joints of the 4th and 5th fingers were in flexion position [Table/Fig-1]. Active extension was limited to −30 degrees for the 4th finger and −60 degrees for the 5th finger. Passive extension was full but painful for both fingers. The 4th and 5th fingers clawing appearance of the right hand looked like ulnar neuropathy, but the sensory and motor examination of the patient was normal. Ulnar pulse was palpable at the wrist level distal to the swollen.
Right hand clinical appearance.

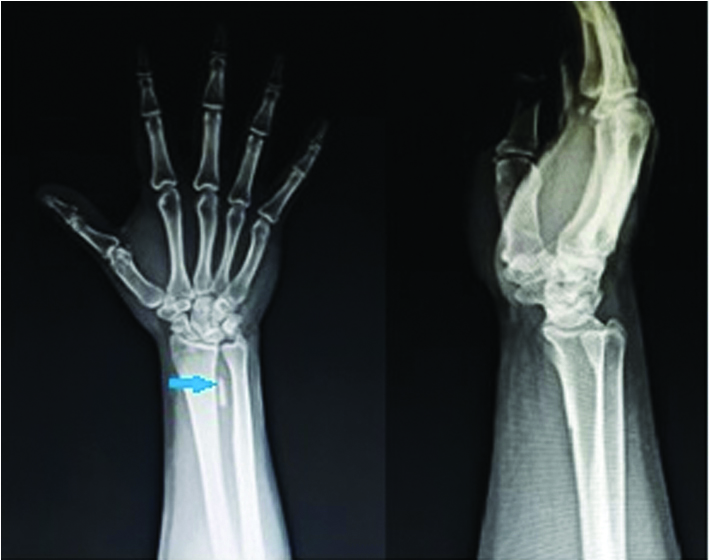
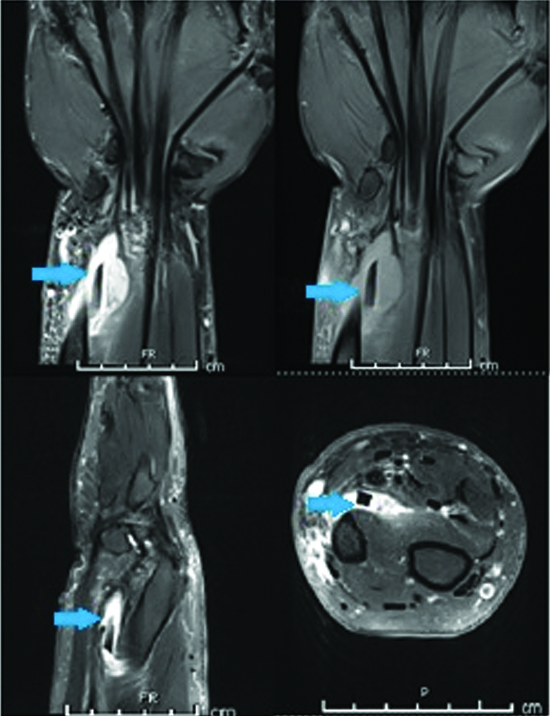
Plain radiographs of the patient revealed the foreign body [Table/Fig-2]. His sedimentation rate, C-reactive protein and white blood cells lab results were normal. A 30 mm foreign body compressing the Flexor Digitorum Profundus (FDP) tendons of the 4th and 5th fingers was inspected by MRI [Table/Fig-3].
Right wrist x-ray (Anteroposterior and Lateral view).
Right wrist MRI coronal, sagittal and axial sequence view.
He was questioned regarding the possibility of foreign material. He explained that a work-related injury occurred due to the penetration of a glass piece from a broken window 10 years previously which was sutured in an emergency room. He refused any radiologic evaluation prior to the suturation. He stated that he had experienced no complaints after the injury until three weeks prior to his admittance to the clinic.
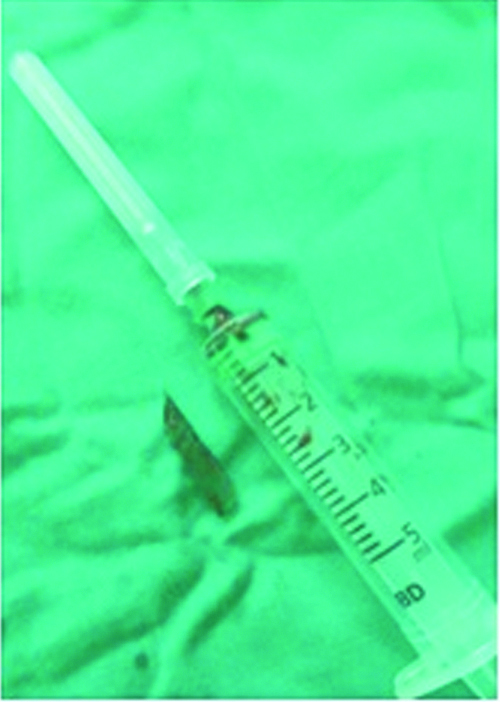
Surgery was performed via a 6 cm volar longitudinal incision over the swelling and a 30 mm glass piece was removed from the FDP muscle [Table/Fig-4]. The retained glass piece was well circumscribed by fibrotic tissues. Samples from the surrounding inflamed and fibrotic tissues were obtained for microbiology. His postoperative neurovascular examination was normal. There were no bacteria, although a high leukocyte count was observed in the gram staining. The culture result was negative for infection. In his one month follow-up, he had no complaints with no pain or swelling around the excision scar and passive-active flexion-extension movement of the 4th and 5th finger was painless. His physical examination revealed full range of motion of the fingers and the wrist with no swelling and tenderness in his last follow-up after six months [Table/Fig-5]. The patient was informed that pictures, radiographs and data from the case would be submitted for publication and he gave his consent.
Removed glass fragment at time of operation.
Right hand clinical appearance six months after surgery.

Discussion
Retained foreign bodies in soft tissues could cause delayed problems, even up to10 years later, as observed in the present case. Chronic pain, infection, damage to the surrounding anatomical structures, Range of Motion (ROM) restriction and pseudotumour formation are some of the wide array of problems that can occur [1-3]. In the present case, delayed presentation of the retained glass material after a prolonged asymptomatic period is particularly interesting. Although, several similar cases have been reported in the literature [4,5]. The present study is unique as the delayed presentation was caused by overuse of the muscle in which the glass material was retained. Also, this case report highlights the importance of radiologic evaluation after penetrating injuries.
The reasons for delayed problems are not clear. Inflammatory reaction to the retained inorganic foreign body causes fibrous tissue encapsulation and it may remain dormant for years. The new onset of symptoms could be explained by three scenarios. In the first scenario, infection of the foreign body through a haematogenous process may be the reason for the symptoms [6]. In the present case, there were no systemic infection but mild infection was seen and the laboratory results were negative for systemic infection. Furthermore, postoperative gram staining and culture were negative. The second scenario involves damage caused by migration of the glass piece. Migration of foreign materials has been reported in the literature. Yang SS et al., reported a case of glass material migration through the hand, which caused a flexor pollicis longus tendon rupture over a period of 30 years [4]. In this case, the entrance point was not determined, as there was no scar formation. Therefore, there was no definitive evidence of migration of the foreign body. In the third scenario, any recent trauma could cause damage to the surrounding tissues; thus, the formation of inflammation results in pain and pseudotumour formation. In the case, the patient did not report any recent trauma. Nevertheless, his job had changed and he subsequently overused flexor muscles with repetitive flexion-extension movements. His complaints started soon after his job changed. It is possible that sharp edges of the glass caused injury to the surrounding fibrotic tissue and muscle with repetitive flexion-extension movements of the wrist. Irritation of the flexor digitorum profundus muscle caused painful extension motion and flexion posture of the 4th and 5th fingers.
In literature, it is recommended that retained organic structures like wooden particles should be extracted because of the risk of infection [1]. On the other hand, retained metal objects can be asymptomatic. However, inorganic materials with sharp edges may cause problems due to migration, trauma or repetitive muscle contractions. Previous reports as well as this case showed the risk of injury to the surrounding anatomical structures by the retained glass material [4,5]. Hence, the authors recommend removal of retained glass pieces and other foreign materials with sharp edges.
Conclusion
Retained soft tissue foreign bodies should be suspected in differential diagnosis of soft tissue masses. History of a penetrating trauma should be questioned persistently, as the retained foreign bodies could even cause symptoms many years after the injury.
[1]. Gulati D, Agarwal A, Wooden foreign body in the forearm-presentation after eight yearsUlus TravmaAcilCerrahiDerg 2010 16(4):373-75. [Google Scholar]
[2]. Meurer WJ, Radial artery pseudoaneurysm caused by occult retained glass from a hand lacerationPediatrEmerg Care 2009 25(4):255-57.10.1097/PEC.0b013e31819e374419369839 [Google Scholar] [CrossRef] [PubMed]
[3]. Yanay O, Vaughan DJ, Diab M, Brownstein D, Brogan TV, Retained wooden foreign body in a child’s thigh complicated by severe necrotizing fasciitis: A case report and discussion of imaging modalities for early diagnosisPediatrEmerg Care 2001 17(5):354-55.10.1097/00006565-200110000-0000911673714 [Google Scholar] [CrossRef] [PubMed]
[4]. Yang SS, Bear BJ, Weiland AJ, Rupture of the flexor pollicis longus tendon after 30 years due to migration of a retained foreign bodyJ Hand Surg Br 1995 20(6):803-05.10.1016/S0266-7681(95)80052-2 [Google Scholar] [CrossRef]
[5]. Ozsarac M, Demircan A, Sener S, Glass foreign body in soft tissue: possibility of high morbidity due to delayed migrationJ Emerg Med 2011 41(6):e125-28.10.1016/j.jemermed.2008.04.05119038521 [Google Scholar] [CrossRef] [PubMed]
[6]. Ipaktchi K, Demars A, Park J, Ciarallo C, Livermore M, Banegas R, Retained palmar foreign body presenting as a late hand infection: proposed diagnostic algorithm to detect radiolucent objectsPatient Saf Surg 2013 7(1):2510.1186/1754-9493-7-2523844904 [Google Scholar] [CrossRef] [PubMed]