STSG is one of the main surgical procedures to repair soft tissue loss in patients with non-healing chronic wounds. Proper wound bed preparation is the mainstay of successful skin grafting [1].
There are number of studies that have focused on the importance of qualitative rather than quantitative bacteriology and others vice versa. But, the impact of bacteria in a wound depends on three major factors like bacterial load, virulence of the bacteria and the host immune response. Therefore, bacteriological culture of chronic non healing wounds that are prepared for skin grafting should be performed.
Hence in this present study, quantitative and qualitative bacteriological profile of granulating wound beds that were prepared for grafting was done, to analyse the influence of bacterial bio-burden on the success rate of STSG.
Materials and Methods
This study was a cross-sectional study, carried out in the Institute of Microbiology, Madras Medical College from March 2016 to August 2016. Approval from the Institutional Ethics committee was obtained before commencement of the study. Informed consent was obtained from patients who satisfied the inclusion criteria. A total of 100 patients with chronic non healing ulcer wounds prepared for STSG were included in the study. Patients with ulcers at multiple sites prepared for STSG were included separately. Patients with age < 18 years and patients with chronic non healing ulcer wounds prepared for full thickness skin grafts or flaps were excluded from the study.
Specimen Collection and Transport
Tissue sample from the recipient wound bed was collected 24 to 72 hours before grafting. The wound was cleaned thoroughly with sterile saline and all superficial exudates removed. Sufficient tissue sample from base or advancing margin of lesion about 3 to 4mm was collected using sterile forceps and placed in a sterile container containing sterile normal saline and transported immediately.
Sample Processing
The sterile container containing the tissue was weighed on an analytical balance. The tissue was removed by using aseptic technique. The empty container was reweighed and subtracted to determine the weight of the tissue in milligrams. The tissue was homogenised for 15 to 30 sec by sterile scalpel petri dish method of homogenisation of tissue and vortex mixed in 5 ml 0.85% sodium chloride. Direct Gram staining was done from the original homogenate.
A 0.1 mL of the original homogenate was streaked onto Blood agar plate and MacConkey agar and labelled as plate 10-1.
A 4.5 mL of sterile normal saline was taken in three test tubes. A 0.5 mL of original homogenate was added to first tube containing 4.5 mL normal saline and serial dilutions made in next two tubes and labelled as 10-2, 10-3, 10-4.
A 0.1 mL of each dilution was plated onto Blood agar plates and plates were labelled as 10-2, 10-3, 10-4.
Plates were incubated for 18 to 24 hours at 37°C under aerobic conditions [6].
Quantitative Measurement of Culture
After 18 to 24 hours of incubation, MacConkey agar and Blood agar plates were observed for growth, colony count and colony morphology. The number of organisms per gram of tissue was determined by counting the colonies in the plate that grew between 30 to 300 colonies.
The total number of organisms was calculated by using the colony count times the dilution factor (using 5 as the factor for the homogenate dilution and dilutions labelled on the plates for subsequent dilutions) divided by original weight of the tissue [6].
The colony count is reported as total count “per gram of tissue”. A colony count of >105 CFU/g was considered as significant growth [1,5].
The success rate of the graft uptake was then assessed between 2nd to 15th postoperative days on clinical grounds.
Statistics
The results were analysed statistically using SPSS version 17.0.
Results
Out of 100 patients, 32 patients had significant bacterial growth with bacterial counts ≥ 105CFU/g of tissue in preoperative quantitative culture. Out of 32 patients, mixed flora was isolated in 2 patients. Seven patients had growth with bacterial counts ≤ 105CFU/g of tissue. Hence a total of 41 bacterial isolates were obtained in preoperative quantitative culture [Table/Fig-1].
Analysis of bacterial isolates based on preoperative quantitative culture results.
| Pre-Op Culture | Bacterial Count | No. of Isolates | Total No. of Isolates |
|---|
| Growth | ≥105CFU/g of tissue | 34 | 41 |
| ≤105CFU/g of tissue | 7 |
| No Growth | - | - | 61 |
Out of 41 preoperative bacterial isolates, 34 (from 32 patients) were significant bacterial growth of counts ≥105CFU/g of tissue in preoperative quantitative culture. Seven patients had growth with bacterial counts ≤ 105CFU/g of tissue [Table/Fig-2].
Analysis of bacterial count in preoperative quantitative bacterial culture n=41.
| Preoperative Bacterial Count CFU/g of tissue | Number of Isolates | Total |
|---|
| 106 | 13 | 34 |
| 105 | 21 |
| 104 | 6 | 7 |
| 103 | 1 |
| TOTAL | 41 | 41 |
In the healed category 61 patients had no growth in preoperative quantitative culture. One patient had Escherichia coli with bacterial count 103 in preoperative quantitative culture with 98% graft uptake postoperatively, which was included in healed category.
A total of 38 patients who had reduced graft uptake were included in non-healed category, out of which, only 32 patients had significant bacterial growth in preoperative quantitative culture. Six patients, who had insignificant bacterial growth, also showed reduced graft uptake [Table/Fig-3].
Analysis of clinical evaluation of graft uptake n=100.
| Category | Percentage of Graft Uptake | Number of Patients |
|---|
| Healed (62) | 100% | 61 |
| 98 & 99% | 1 |
| Non Healed (38) | 75 to 97% | 29 |
| 5 to 74% | 9 |
| <5% | 0 |
| Total | 100 |
Graft uptake was reduced when preoperative quantitative bacterial count was ≥105. The correlation between preoperative bacterial count and graft uptake rate was statistically significant, as analysed by “Independent sample t-test”, p-value <0.05 [Table/Fig-4].
Analysis of significance of preoperative bacterial count on graft uptake rate.
| Pre-Op Quantitative Bacterial Count | No. of Patients with Reduced Graft Uptake | Mean Graft Uptake % | p-value |
|---|
| ≤105 | 32 | 78.32% | 0.024 |
| ≤104 | 7 | 93.00% | |
The most commonly isolated pathogens in preoperative quantitative culture were Staphylococcus aureus (26.4%) and Pseudomonas aeruginosa (26.4%) [Table/Fig-5].
Graft uptake was reduced if preoperative wound bed was infected with Pseudomonas aeruginosa or Staphylococcus aureus. The correlation between bacterial type and graft uptake rate was statistically significant, as analysed by “One sample t-test” (p-value <0.05) [Table/Fig-6].
Bacteriological profile of preoperative quantitative bacterial culture.
| Type of Isolate | Organism | Total Number of Organisms | Percentage |
|---|
| Gram Positive Cocci | Staphylococcus aureus | 9 | 26.4% |
| Gram Negative Bacilli | Pseudomonas aeruginosa | 9 | 26.4% |
| Pseudomonas species | 3 | 8.9% |
| Klebsiella pneumonia | 3 | 8.9% |
| Klebsiella oxytoca | 2 | 5.8% |
| Acinetobacter baumannii | 3 | 8.9% |
| Escherichia coli | 1 | 2.9% |
| Proteus mirabilis | 3 | 8.9% |
| Proteus vulgaris | 1 | 2.9% |
| TOTAL | 34 | 100% |
Analysis of the significance of preoperative bacterial isolates on the graft uptake rate.
| Isolate | Mean of Graft Uptake Percentage | p-value |
|---|
| Staphylococcus aureus | 75.55% | 0.002 |
| Pseudomonas aeruginosa | 68.88% | 0.000 |
| Pseudomonas species | 80.00% | 0.020 |
| Klebsiella species | 85.00% | 0.008 |
| Acinetobacter baumannii | 88.33% | 0.020 |
| Proteus species | 88.33% | 0.020 |
| Escherichia coli | 94.50% | 0.045 |
This plot in [Table/Fig-7] depicts the relation of percentage of graft uptake and the preoperative bacterial isolates. The mean of graft uptake percentage and its 95% CI limits are represented.
A 95% Confidence interval plot.
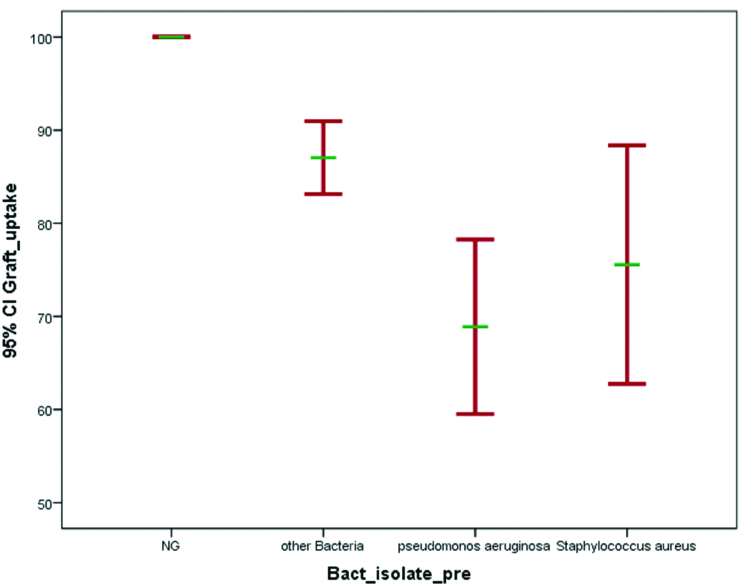
Mean of graft uptake percentage in patients with Staphylococcus aureus in preoperative quantitative culture was 75.55%, with Pseudomonas aeruginosa was 68.88%, and with other bacteria was 87%.
Discussion
STSG are the gold standard treatment for the skin defects due to chronic non healing wounds. Even though the success of skin grafts depends on multiple factors, well vascularised non infected wound bed prior to grafting is crucial.
The purpose of the present study was to analyse the influence of preoperative bacterial bio-burden on the influence of graft uptake rate, by obtaining preoperative bacterial culture of pre-grafted wound bed.
Analysis of Bacterial Isolates Based on Preoperative Quantitative Culture Results
Among the 100 patients who underwent STSG surgery, 32 patients had significant bacterial growth with bacterial counts ≥105CFU/g of tissue from the wound bed, in preoperative aerobic quantitative culture. Out of 32 patients, mixed flora was isolated in two patients. One patient had infection with Klebsiella pneumoniae and Acinetobacter baumanii. The other patient had infection with Staphylococcus aureus and Proteus mirabilis. There were seven patients who had growth with bacterial counts ≤105CFU/g of tissue. Hence a total of 41 bacterial isolates were obtained in preoperative quantitative culture [Table/Fig-1,2].
The rate of preoperative bacterial growth in this study differs from the rates that were reported in other studies. In the study by Leslie Gilliland E et al., 54(61%) patients out of 88 patients showed growth in the immediate preoperative period [7]. In another study, wounds culture done immediately before grafting showed around half (53%) the wound beds had been infected, while the other half (47%) showed no growth in culture [8].
The lower rate of isolation of bacteria on this study is because quantitative bacterial culture was done preoperatively by taking tissue bit from wound bed and only those with bacterial count of ≥ 105CFU/g of tissue were interpreted as significant growth. But in both the above mentioned studies only qualitative bacterial culture was done by collecting wound swab.
The differences in the rate of preoperative bacterial growth may also be due to varying sample size, age and gender distribution of the patients, patients with concomitant illness, indication for STSG and the use of prophylactic antibiotic therapy.
Analysis of Clinical Evaluation of Graft Uptake
In the present study graft uptake was divided into two groups: healed versus not-healed, with five subgroups in total [9].
The healed category was divided into two subgroups:
Completely healed (100%);
Healed with 98% or more graft uptake.
The not-healed category was divided into three subgroups:
Less than 98% but more than 75% take (75%-98%);
75% or less but more than 5% take (5%-75%);
5% or less take (0-5%).
Mean graft uptake in this present study was 92%. In the healed category 61 patients had no growth in preoperative quantitative culture. Escherichia coli with bacterial count 103 was isolated in one patient in preoperative quantitative culture with 98% graft uptake postoperatively, who was also included in healed category. A total of 38 patients who had reduced graft uptake were included in non-healed category, out of which, only 32 patients had significant bacterial growth in preoperative quantitative culture. Six patients, who had insignificant bacterial growth, also showed reduced graft uptake [Table/Fig-3].
Significance of Preoperative Bacterial Count on Graft Uptake Rate
In this study the significance of preoperative bacterial count on the outcome of graft uptake was analysed [Table/Fig-4]. In the present study mean of graft uptake percentage of patients with ≥105CFU/g of tissue in preoperative quantitative culture was 78.32% and mean of graft uptake percentage of patients with ≥105 was 93%. It was thus observed that graft uptake was reduced when preoperative bacterial culture was ≥105CFU/g of tissue, which is statistically significant (p<0.05).
This observation was similar to the few studies that have considered the number of organisms to be critical for skin graft healing. In the study by Majewski W et al., which had shown the usefulness of quantitative bacteriology for the determination of the severity of infections, the healing results of skin grafts were better in the group where the number of bacteria in 1 cm2 of ulceration was lower [10]. In another clinical study, conducted by Bacchetta CA et al., it was observed that the wounds which were heavily contaminated with 107 organisms had skin graft failure. Graft uptake was better in wounds with lower bio-burden [11].
Bacteriological Profile of Preoperative Quantitative Bacterial Culture
Out of the 34 aerobic bacterial isolates obtained from 32 patients in the present study from the pre-grafted wound bed, the predominant pathogens isolated by quantitative culture were Staphylococcus aureus and Pseudomonas aeruginosa each 26.4% [Table/Fig-5].
The other isolates were Klebsiella pneumonia (8.9%), Klebsiella oxytoca (5.8%), Escherichia coli (2.9%), Proteus mirabilis (8.9%), Proteus vulgaris (2.9%), and Acinetobacter baumanii (8.9%). Three Pseudomonas species (8.9%) were isolated out of which one was Pseudomonas fluorescens, and two were Pseudomonas putida.
The results were similar to study conducted by Thomsen TR et al., in which the bacterial flora of wound bed from 14 skin graft operations was examined [12]. The study showed Staphylococcus aureus, Pseudomonas aeruginosa, Klebsiella oxytoca and Enterococcus species as the common pathogens. The results were also similar to the study conducted by Majewski W et al., in which, it was observed that among the isolated bacteria in preoperative wound bed before skin grafting, the most common were Staphylococcus aureus (62.9%) [10]. In another study by Bowler PG et al., the most common pathogens in chronic diabetic wound infections were aerobic bacteria such as Staphylococcus aureus, including MRSA strains, Coagulase negative Staphylococci, Streptococcus species and Enterobacteriaceae family [4].
Significance of Preoperative Bacterial Isolates on the Graft Uptake Rate
In the present study significance of type of bacteria isolated in the preoperative quantitative culture on graft uptake rate was analysed [Table/Fig-6].
The mean graft uptake percentage in this study, when pre-grafted wound was infected with Pseudomonas aeruginosa was 68.88% and for Staphylococcus aureus was 75.55%. This was similar to the study by Gilliand EL et al., in which the mean graft uptake rate of wound beds infected with Staphylococcus aureus was reduced to 75% [7].
In the current study, the mean graft uptake was reduced by 24.5% if immediate preoperative culture showed Staphylococcus aureus and mean graft uptake reduced by 31.2% if immediate preoperative culture showed Pseudomonas aeruginosa, when compared to the no growth group. Thus, the graft uptake was reduced if preoperative wound bed was infected with Pseudomonas aeruginosa and Staphylococcus aureus, which was found to be statistically significant (p-value <0.05).
These observations were similar to the retrospective study by Gilliand EL et al., in which it was observed that analysis of the immediate preoperative swab results suggested that it was Staphylococcus aureus and Pseudomonas which significantly affect skin graft healing, median graft take being reduced by 15% (p<0.05) and 40% (p<0.01) respectively when compared to the ‘no growth’ group [7].
In another retrospective study, conducted by Høgsberg T et al., it was analysed that that once the ulcers were infected with Pseudomonas aeruginosa, even weeks or months preoperatively, the success of skin graft uptake was reduced [9]. Their results showed that 33.3% of ulcers with Pseudomonas aeruginosa were healed by the 12-week follow-up, while 73.1% of ulcers without Pseudomonas aeruginosa were so by the same time.
The results of this present study were also similar to that of Jackson DM et al., in that the isolation of Pseudomonas aeruginosa from an ulcer immediately prior to skin grafting significantly impairs skin graft take [13]. Unal S et al., had also observed that Pseudomonas aeruginosa was an equally prominent danger in skin graft survival [14].
In the current study the mean graft uptake if preoperative quantitative culture showed Pseudomonas species was 80.00%, for Klebsiella species was 85.00%, for Acinetobacter species and Proteus species was 88.33% each, and for Escherichia species was 94.5% [Table/Fig-6]. Even though statistically significant correlation could be detected between the reduced graft uptake and these bacteria when grown preoperatively, the mean graft uptake percentage was better when compared to Staphylococcus aureus and Pseudomonas aeruginosa, as depicted in the 95% CI plot [Table/Fig-7]. The plot depicts the relation of percentage of graft uptake and the preoperative bacterial isolates. The mean of graft uptake percentage and its 95% CI limits are represented. Patients with no growth on preoperative quantitative culture had 100% graft uptake. Mean of graft uptake percentage in patients with Staphylococcus aureus in preoperative quantitative culture was 75.55%, with Pseudomonas aeruginosa was 68.88%, and with other bacteria was 87%.
This differs from the study conducted by Høgsberg T et al., in which no statistically significant correlation could be detected between the clinical outcome and the other microorganisms [9]. Also, in the study conducted by Gilliand EL et al., bacteria other than Staphylococcus aureus and Pseudomonas aeruginosa did not show any significant difference in the clinical outcome of graft uptake [7].
Limitation
A long term follow up of the patients to assess the graft uptake was not done due to non-feasibility. Anaerobic bacteria causing infection and hence graft failure, was not studied because of lack of resources.
Conclusion
The effect of bacteria on wound healing thus depends on the bacterial bio-burden in the wound and the virulence of the bacteria. This study thus emphasises the importance of quantitative and qualitative bacteriological culture of pre-grafted wound beds prior to skin grafting, to determine the severity of infections in the wound bed, thereby preventing graft failure.