The Leverage Method: A Novel Technique for Difficult Temporomandibular Joint Reduction
Ozkan Onal1, Emine Aslanlar2, Merih Onal3, Cagdas Elsurer4, Cansu Ciftci5
1 Associate Proffesor, Department of Anaesthesiology and Reanimation, Selcuk University Medical Faculty, Konya, Turkey.
2 MD, Department of Anaesthesiology and Reanimation, Selcuk University Medical Faculty, Konya, Turkey.
3 Assistant Proffesor, Department of Ear, Nose and Throat, Selcuk University Medical Faculty, Konya, Turkey.
4 Assistant Proffesor, Department of Ear, Nose and Throat, Selcuk University Medical Faculty, Konya, Turkey.
5 MD, Department of Anaesthesiology and Reanimation, Selcuk University Medical Faculty, Konya, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ozkan Onal, Selcuk University, Medical Faculty, Anaesthesiology and Intensive Care Unit, Selcuklu, Konya, Turkey.
E-mail: drozkanonal@selcuk.edu.tr
Glenoid fossa, Temporomandibular joint dislocation, Temporomandibular joint replacement
Dear Sir,
Posterolateral mandibular dislocation at the Temporomandibular Junction (TMJ) is an infrequent presentation to the Ear Nose Throat (ENT) Department [1]. Several methods have been described for TMJ reduction. The oldest and most conventional technique to manage mandibular dislocation involves the physician using an intraoral bilateral inferior posterior and downward force on the patient’s molar occlusal surfaces [2,3]. In this technique, the physician’s thumbs are placed on the occlusal surface of the patient’s molars, and the physician’s fingers are wrapped laterally around the mandible. A constant inferior and posterior force is then applied, sliding the mandibular condyles back into the glenoid fossa. This technique requires the physician to manually overcome the significant force created by the pterygoid, masseter, and temporalis muscles to reduce the TMJ dislocation. Conscious sedation and significant force are important when applying this reduction technique [1].
Lowery LE et al., described a new technique for treating mandibular dislocation at the TMJ called the “wrist pivot method” [1]. In this technique, the physician’s thumbs are placed at the mentum of the mandible, and an upward force is applied while the fingers are wrapped laterally around the mandible. The simultaneous pivoting action of the physician’s wrists, with the thumb (anterior portion of the fulcrum) pushing superiorly and fingers on the mandibular body pushing inferiorly, allows the condyles to rotate back into the glenoid fossa. Using this new technique, Lowery LE et al., asserted that the muscles of mastication provided assistance rather than impedance, as they promote rotation and reduction [1]. They also stated that the masticatory muscles provide superior and posterior forces and these forces helped, bring reduction into the condyle as the angle of the mandible rotated.
Cheng D described another new technique for treating mandibular dislocation called the “unified hands technique” [4]. In this technique, the physician places both thumbs on the patient’s ipsilateral molar’s occlusal surface to increase the reduction force while applying inferior and posterior pressure. Cheng D reported that the technique of employing two thumbs ipsilaterally intraorally provide more force reduction than conventional methods and thus increased the chance of treating unilateral jaw dislocation [4]. For bilateral dislocations, the unified hands technique is applied first to one side to reduce the dislocation, followed by application of the same technique on the other side. Cheng D applied the unified hands technique successfully to two unilateral jaw dislocations and one bilateral jaw dislocation, without any complications, such as mastication muscle strain, inferior alveolar nerve traction, and mandibular condyle fracture [4]. The same study suggested that a bite block be used to protect the operator’s fingers during the intervention. TMJ dislocatıon represents 3% of all dislocation in the body. Although, anterior dislocation of TMJ is more common form; superior, lateral and posterior dislocations are extremely rare [5]. Around 29 case of superolateral dislocation have been documented in the literature with most of these cases showing associated facial fractures [5]. Only three of these cases showed dislocation without any facial fractures [5]. Present case is the fourth case in the literature documented posterolateral dislocation without any facial fractures.
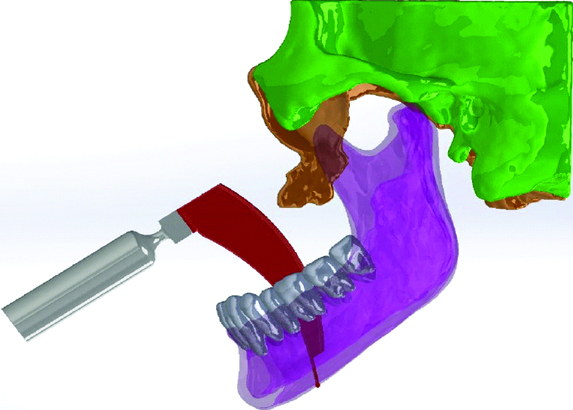
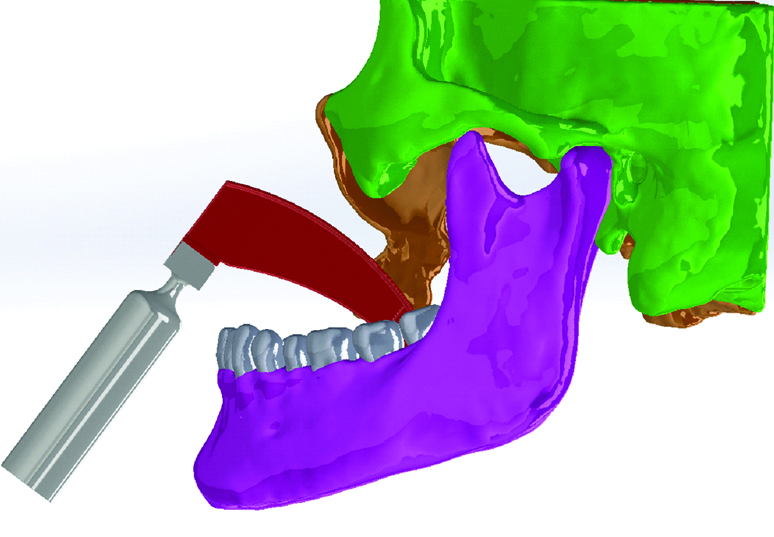
We describe a new technique that has been successfully applied in the treatment of difficult posterolateral TMJ reduction with the help of a laryngoscope, which was not previously applied. A 50-year-old healthy man presented to the ENT department with right sided mandibular pain and an inability to close his mouth due to trauma but without fracture, two days ago [Table/Fig-1,2]. The ENT department tried to reduce posterolateral TMJ dislocation at the service many times but could not reduce it; therefore, it was planned to be reduced under sedation in the operating theater. The patient was monitored and given 100 mcg of fentanyl (Talinat, Vem, Turkey) and 40 mg of propofol (Propofol, Fresenius, Italy), for sedation. The conventional technique was attempted three times by the otolaryngologist but he did not succeed it. The patient received additional sedation, 50 mcg of fentanyl (Talinat, Vem, Turkey) and 30 mg of propofol (Propofol, Fresenius, Italy), and a fourth conventional reduction attempt was made but was again unsuccessful. After consultation, we decided to use a laryngoscope for TMJ reduction, which was used and identified first time by us. An additional 60 mg propofol was given and direct laryngoscopy was applied first time in the literature to reduce the TMJ replacement. The first attempt using the laryngoscope was successful. Direct laryngoscopy allowed the mandibular body to be pushed superiorly, enabling the condyles to rotate back into the glenoid fossa. Bimanual reduction carried out by applying downward and outward pressure over the molar region. In the present case, the outward and lateral pressure were applied to the patient’s jaw by laryngoscope placing it to the premaxilla region not over the molar region bimanually [Table/Fig-3a-c]. Therefore, dislocation was replaced with less force and without risk of human bite for surgeon [Table/Fig-4].
Three dimentional CT image shows superolateral dislocation of left condyle (blue arrow).
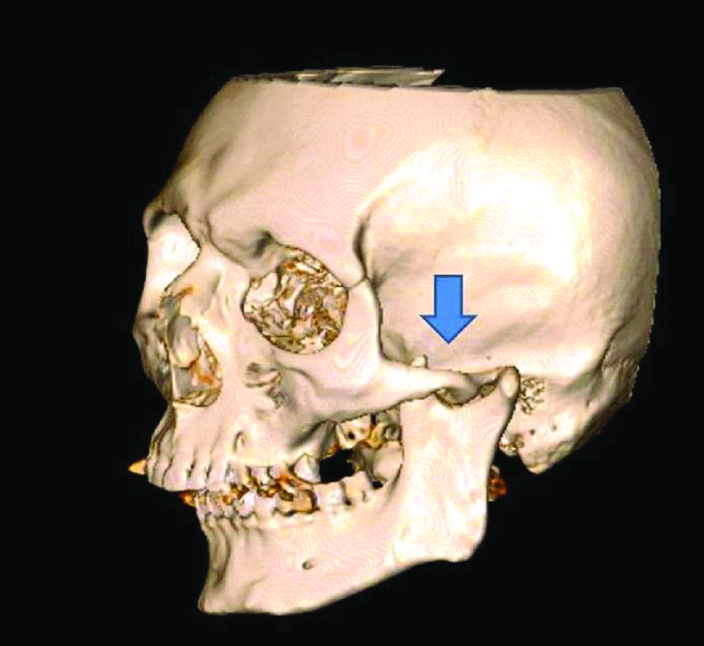
Image of the dislocated TMJ.
Maneuvers of the leverage method respectively. {The outward (orange arrow) and lateral pressure (blue arrow) were applied the patient’s jaw by laryngoscope placing it to the premaxilla region not over the molar region bimanually}. Direct laryngoscopy allowed the mandibular body to be pushed superiorly, enabling the condyles to rotate back into the glenoid fossa.
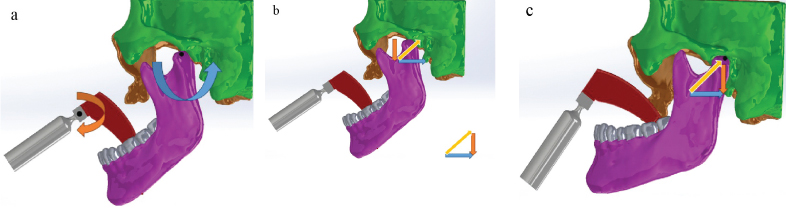
Image of the reducted TMJ.
In conclusion, we describe a novel technique, the leverage technique, for mandibular dislocation, which has not been previously described in the literature.
The leverage technique has the advantage of protecting the operator from a human bite, without using a bite block. In addition, conscious and significant forces are not required. This technique can facilitate physician’s work. Most importantly, by removing the need for significant force, the leverage technique overcomes the possibility of serious complications, such as mastication muscle strain, inferior alveolar nerve traction, and mandibular condyle fracture. The new technique described by us can be supported by a study with a high number of patients.
[1]. Lowery LE, Beeson MS, Lum KK, The wrist pivot method, a novel technique for temporomandibular joint reductionJ Emerg Med 2004 27:167-70.10.1016/j.jemermed.2004.03.00715261360 [Google Scholar] [CrossRef] [PubMed]
[2]. Luyk NH, Larsen PE, The diagnosis and treatment of the dislocated mandibleAm J Emerg Med 1989 7:329-95.10.1016/0735-6757(89)90181-2 [Google Scholar] [CrossRef]
[3]. Chan TC, Harrigan R, Ufberg J, Vilke G, Mandibular reductionJ Emerg Med 2008 34(4):435-40.10.1016/j.jemermed.2007.06.03718242920 [Google Scholar] [CrossRef] [PubMed]
[4]. Cheng D, Techniques and procedures unified hands technique for mandibular dislocationJ Emerg Med 2010 38(3):366-67.10.1016/j.jemermed.2008.12.02219303239 [Google Scholar] [CrossRef] [PubMed]
[5]. Srinath N, Umashankar DN, Naik C, Biradar J, Superolateral dislocation of the intact mandibular condyle: report of a rare case with a reviewInt J Oral Maxillofac Surg 2017 46(11):1424-28.10.1016/j.ijom.2017.05.01228610821 [Google Scholar] [CrossRef] [PubMed]