Cerebral Venous Sinus Thrombosis Complicating Adult Onset Nephrotic Syndrome
Arun Karat Anandan1, Pradeep Balachandran2, Arpitha Chowksey3, Gomathy Sankaranarayanan4, Usha Samuel5
1 Senior Resident, Department of Nephrology, Government TD Medical College, Alappuzha, Kerala, India.
2 Senior Resident, Department of Nephrology, Government TD Medical College, Alappuzha, Kerala, India.
3 Lecturer, Department of Nephrology, Government TD Medical College, Alappuzha, Kerala, India.
4 Additional Professor, Department of Nephrology, Government TD Medical College, Alappuzha, Kerala, India.
5 Professor, Department of Nephrology, Government TD Medical College, Alappuzha, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arun Karat Anandan, Senior Resident, Department of Nephrology, Government TD Medical College, Alappuzha-688001, Kerala, India.
E-mail: drarunkarat@gmail.com
Nephrotic syndrome is well known for its hypercoagulable state and thrombotic complications. This warrants cautious management of the disease with meticulous monitoring for thrombotic complications as it carries high morbidity and mortality than the original disease itself most often. Here, we present a case of adult onset nephrotic syndrome referred to our centre for further evaluation and management. On detailed work up, she turned out to be a case of minimal change disease. During her recovery period in the hospital she developed headache and diplopia. Sudden onset of neurological symptoms in the background of a thrombotic milieu prompted us to do further neurological evaluation which revealed extensive cerebral venous sinus thrombosis. She received anticoagulation without delay. Although the condition is associated with high mortality our patient showed very good response to anticoagulation and she was discharged in a stable condition.
Anticoagulation, Diplopia, Hypercoagulable state, Minimal change disease
Case Report
A 40-year-old lady presented with complaints of insidious onset facial puffiness that appeared one week back which progressed rapidly to develop into a state of generalised oedema by the third day of symptom onset. Along with this, she also noted a significant decline in the quantity of urine she passed over those days and described the urine as high coloured. After four days into the illness she developed shortness of breath and then she was referred to our hospital from a general practitioner. She did not report any symptom suggestive of decompensated cardiac failure or liver failure. She did not have fever or other clues for a recent infection. She had history of gestational hypertension during her previous two pregnancies which were successfully managed with oral antihypertensives. She did not report any features of connective tissues disorders, recurrent abortion, and any drug intake prior to the onset of this illness including oral contraceptive pills or any significant family history.
Physical examination revealed generalised oedema. Blood pressure was normal (130/80). There was ascites and bilateral pleural effusion and otherwise system examination was unremarkable. Her urine protein quantified to 35g/day. There were no active sediments in the urine. Serum creatinine was 1.5mg/dl. She underwent extensive evaluation to rule out any secondary causes for nephrotic syndrome. Details of the investigations are given in [Table/Fig-1]. She received treatment in the form of injection dexamethasone equivalent to 2mg/kg of prednisolone, Human albumin infusion 1g/kg over 3 days and 5 units of fresh frozen plasma. Urine output improved after 2 days of admission to 1.5L/day and oedema subsided over a period of 1 week. Twenty four hour proteinuria decreased to 2g/day at the end of first week after admission.
Laboratory investigations.
| Urine examination | Lipid profile | Renal biopsy |
|---|
| Protein - ++++Sugar- NilWBC- 0-1RBC- Nil24 hour urine protein-8.5g/day | Total cholestrol- 560mg/dlTriglyceride -141 mg/dlLDL- 452 mg/dlHDL-80 mg/dlVLDL-28 mg/dl | Near normal glomeruli with negative immunoflourescence |
| Total count- 10600/mm3 | Peripheral smearNegative for haematological malignancies |
| Polymorphs-82% | USG AbdomenModerate ascites |
| Haemoglobin-14.5g/dl |
| Hematocrit- 44% | Chest X-rayBilateral minimal pleural effusion |
| Platelet count- 2.6 lakhs/dl |
| ESR-50mm at 1 hour | ECGLow voltage complex |
| Bilirubin – 0.3mg/dl |
| Total protein-4.2g/dl | EchocardiogramMinimal pericardial effusion |
| Albumin- 1.9g/dl |
| SGOT- 15 IU/dl | Stool for occult bloodNegative |
| SGPT-11 IU/dl |
| Alkaline phosphatise-102 IU/L | Tumour markers |
| Blood urea- 35mg/dl | CA-19-9 – normal |
| Serum creatinine-1.5mg/dl | CA-125 – normal |
| Sodium- 130meq/dl | CEA – negative |
| Potassium -3.3 meq/dl | LDH- Normal |
| Blood glucose -96mg/dl | MammogramBirads-1 |
| ANA profile- negative |
| Serum C3 – normal |
| Serum electrophoresis-normal |
| HIV/HbsAg/anti HCV-negative |
| TSH- 3.8 IU/dl. |
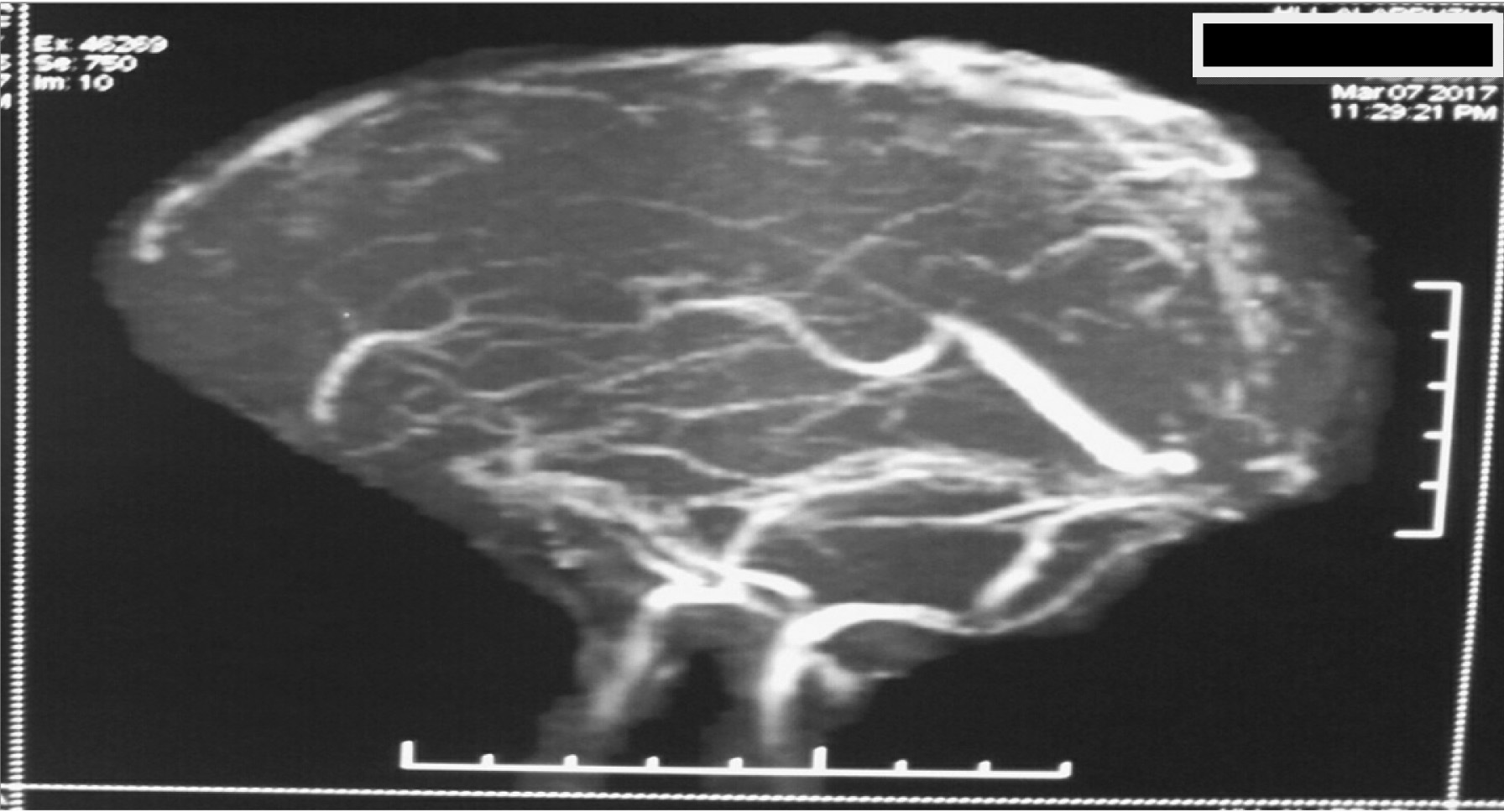
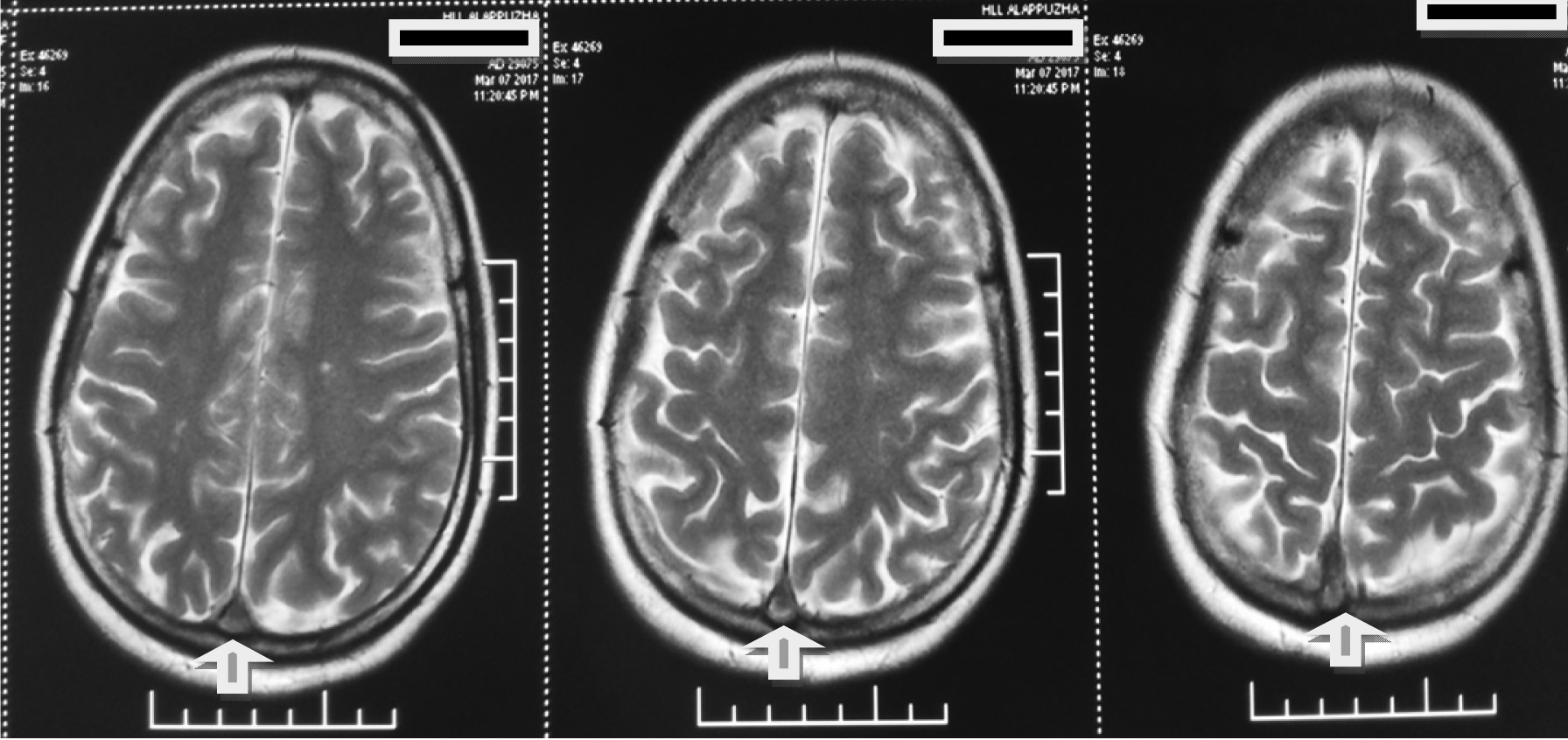
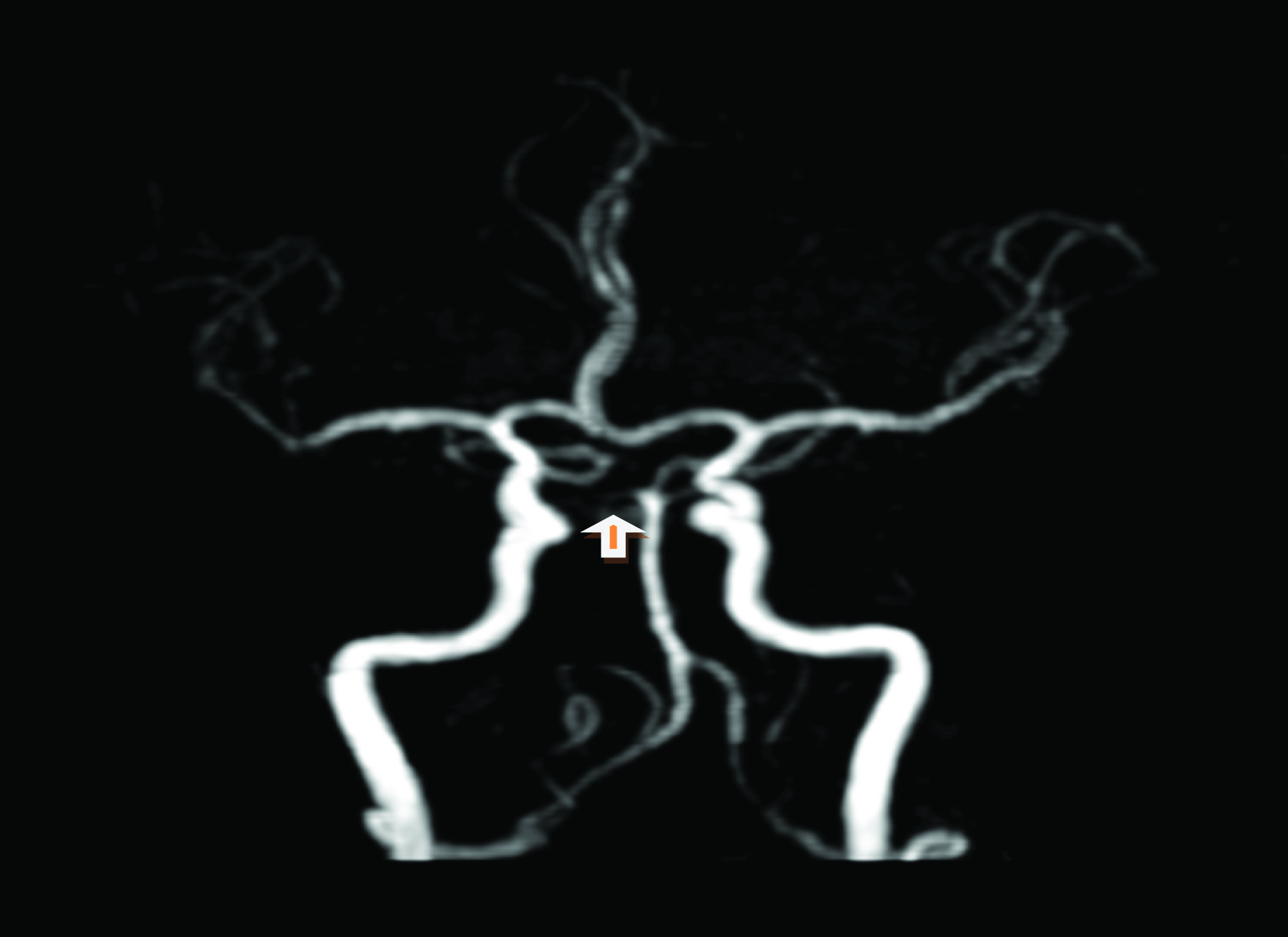
One week after the admission she developed severe headache and vomiting associated with double vision. Physical examination showed papilloedema and bilateral lateral rectus palsy. Suspecting an intracranial lesion with raised ICT, we proceeded with MR imaging of the brain with MR venogram. The imaging showed extensive thrombosis involving the superior sagittal sinus, sigmoid sinus and bilateral transverse sinus [Table/Fig-2,3]. As an incidental finding in MR Angiogram there was fetal origin of both posterior cerebral arteries [Table/Fig-4].
Poor opacification in the region of SSS and sigmoid sinus.
T2WI serial section showing thrombus in the region of trocula.
Fetal origin of posterior cerebral arteries.
Anticoagulation was immediately started with heparin infusion and later changed to oral vitamin k antagonist warfarin and she had marked improvement in symptoms after 3 days of treatment. She was discharged after one week in good clinical condition and is under regular follow up now.
Discussion
The most worrisome complication of nephrotic syndrome of any aetiology is the associated enhanced thrombotic tendency. Though thrombosis affecting the venous bed is most often seen clinically, the risk of arterial thrombosis is also high in nephrotic syndrome. Patients with nephrotic syndrome have 800 times higher risk of thrombotic complications in comparison with the general population [1]. The pathological changes that disrupt the fine tuned balance between procoagulant and anticoagulant system in the body is well described. This include changes in the levels of coagulation factors, decline in the level and activity of anticoagulant proteins (antithrombin III & protein S), decrease in plasmin, decreased fibrinolytic activity, increased plasma fibrinogen etc. Haemoconcentration, increased blood viscosity, increase in platelet aggregabilty also contribute to it along with iatrogenic factors like use of corticosteroids, injudicious use of diuretics and dehydration [2].
Cerebral Venous Thrombosis (CVT) was first described by Ribes in 1825 [3]. Although CVT is increasingly being recognised with better awareness and widespread availability of MR imaging, CVT secondary to Nephrotic syndrome is not very common. It is very rare in childhood onset nephrotic syndrome [4]. One study conducted long back showed that clinically significant thrombosis was more common in adults than in children and commonly seen in patients of 20-45 years of age [5,6]. CVT or any thrombotic complications tend to be more common at the time of first presentation as in our patient [7]. The clinical presentation is variable from subtle signs to coma and moreover in many patients it is totally asymptomatic. When dealing with a patient with active nephrotic syndrome clinician should be highly vigilant about this life threatening complication which can present with unexplained neurological signs and symptoms [8].
MRI with venogram has high sensitivity and is the imaging modality of choice [9]. Conventional angiogram may be required if MR venogram turns out to be normal in a patients with high suspicion of CVT [10]. Management involves addressing all the factors contributing to the thrombotic milieu and anticoagulation. Heparin followed by oral anticoagulation is the standard of care [11]. There is no clear cut guidelines for duration of anticoagulation specifically designed for this disease. Anticoagulation should be continued until the patient achieves complete remission [12]. Some authors recommend 3-6 months of oral anticoagulation and a repeat MR venogram at 6 months [13]. There are case reports of successful thrombolysis of extensive CVT in the literature but strong evidence is lacking in this regard [1]. Prophylactic anticoagulation may be given if the serum albumin is <2/dl, serum fibrinogen >6g/L or antithrombin III level is <70% of the normal [14].
Conclusion
Nephrotic syndrome is an uncommon disease in adult population. Besides its timely diagnosis extensive search should be carried out for any secondary causes including occult malignancy before starting the definitive treatment. Simultaneously treating physician should monitor for complications that may arise in the nephrotic milieu. Thrombotic complications are fairly common and their proper management significantly lowers the morbidity and mortality of the disease.
[1]. Kerlin Bryce A, Ayoob R, Smoyer William E, Epidemiologyand pathophysiology of nephrotic syndrome—associated thromboembolic diseaseClin J Am Soc Nephro 2012 7(3):513-20.10.2215/CJN.1013101122344511 [Google Scholar] [CrossRef] [PubMed]
[2]. Pendergraft WF, Nachman PH, Charles Jennette J, Falk RJ, Primary Glomerular Disease. In:Brenner & Rector’s the kidney 2016 table 32.510th EditionElsevier [Google Scholar]
[3]. Raizer JJ, De Angelis LM, Cerebral sinusthrombosis diagnosed by MRI and MR Venography in cancer patientsNeurology 2000 54:1222-26.10.1212/WNL.54.6.122210746588 [Google Scholar] [CrossRef] [PubMed]
[4]. Babu A, Boddana P, Robson S, Ludeman L, Cerebral infarction in patient with minimal change nephrotic syndromeIndian J Nephrol 2013 23:51-53.10.4103/0971-4065.10720323580806 [Google Scholar] [CrossRef] [PubMed]
[5]. Mehls O, Andrassy K, Koderisch J, Herzog U, Ritz E, Hemostatis and thromboembolism in children with nephritic syndrome: differences from adultsJ Pediatr 1987 110:862-67.10.1016/S0022-3476(87)80397-9 [Google Scholar] [CrossRef]
[6]. Xu H, Chen K, Lin D, Dai L, Chen H, Xu Z, Cerebral venous sinus thrombosis in adult nephrotic syndromeClin Nephrol 2010 74(2):144-49.10.5414/CNP7414420630135 [Google Scholar] [CrossRef] [PubMed]
[7]. Bhoobun S, Jalloh AA, Jacobsen KH, Cerebral venous thrombosis in a child with nephrotic syndrome: case reportThe Pan African Medical Journal 2012 13:5710.11604/pamj.2012.13.57.195423346271 [Google Scholar] [CrossRef] [PubMed]
[8]. Nishi H, Abe A, Kita A, Toki T, Noda N, Tsuchihashi D, Cerebral venous thrombosis in adult nephrotic syndrome due to systemic amyloidosisClin Nephrol 2006 65(1):61-64.10.5414/CNP6506116429845 [Google Scholar] [CrossRef] [PubMed]
[9]. Fluss J, Geary D, deVeber G, Cerebral sinovenous thrombosis and idiopathic nephrotic syndrome in childhood: report of four new cases and review of the literatureEur J Pediatr 2006 165(10):709-16.10.1007/s00431-006-0147-716691407 [Google Scholar] [CrossRef] [PubMed]
[10]. Sunil Kumar K, Lakshmi AY, Padmanabhan S, Vengamma B, Siva Kumar V, Cerebral venous sinus thrombosis in nephrotic syndromeIndian J Nephrol 2005 15:103-04. [Google Scholar]
[11]. Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M, Guidance for the management of venous thrombosis in unusual sitesJournal of Thrombosis and Thrombolysis 2016 41:129-43.10.1007/s11239-015-1308-126780742 [Google Scholar] [CrossRef] [PubMed]
[12]. Akatsu H, Vaysburd M, Fervenza F, Cerebral venous thrombosis in nephrotic syndromeClin Nephrol 1997 48(5):317-20. [Google Scholar]
[13]. Thanu S, Unni VN, Anil M, Rajesh R, George K, Cerebral venous thrombosis in Nephrotic syndromeAmrita Journal of Medicine 2014 10(2):1-44. [Google Scholar]
[14]. Hashmi M, Wasay M, Caring for cerebral venous sinus thrombosis in childrenJ Emerg Trauma Shock 2011 4(3):389-94.10.4103/0974-2700.8387021887032 [Google Scholar] [CrossRef] [PubMed]