Idiopathic Abdominal Cocoon and Ileal Fecaloma: A Rare Combination Causing Acute Intestinal Obstruction in an Elderly Male
Narendra Pandit1, Laligen Awale2, Sridhar Keerthi3, Lokesh Shekher Jaiswal4, Shailesh Adhikary5
1 Associate Professor, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
2 Assistant Professor, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
3 Senior Resident, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
4 Associate Professor, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
5 Professor, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Narendra Pandit, Associate Professor, Department of Surgery, B P Koirala Institute of Health Sciences (BPKIHS), Dharan, 1, Nepal.
E-mail: narendrapandit111@gmail.com
Abdominal cocoon is a rare cause of intestinal obstruction commonly seen in adolescent girl or adults of young age group in tropics; however its occurrence in elderly male is rare. Moreover, fecaloma although described in setting of megacolon, it has not been reported for small bowel in presence of cocoon abdomen. Here, we report a rare combination of fecaloma and cocoon abdomen causing intestinal obstruction in an elderly male diagnosed preoperatively by Contrast Enhanced CT (CECT) abdomen and operated successfully by surgery.
Adhesiolysis, Cocoon Abdomen, Ileal loop
Case Report
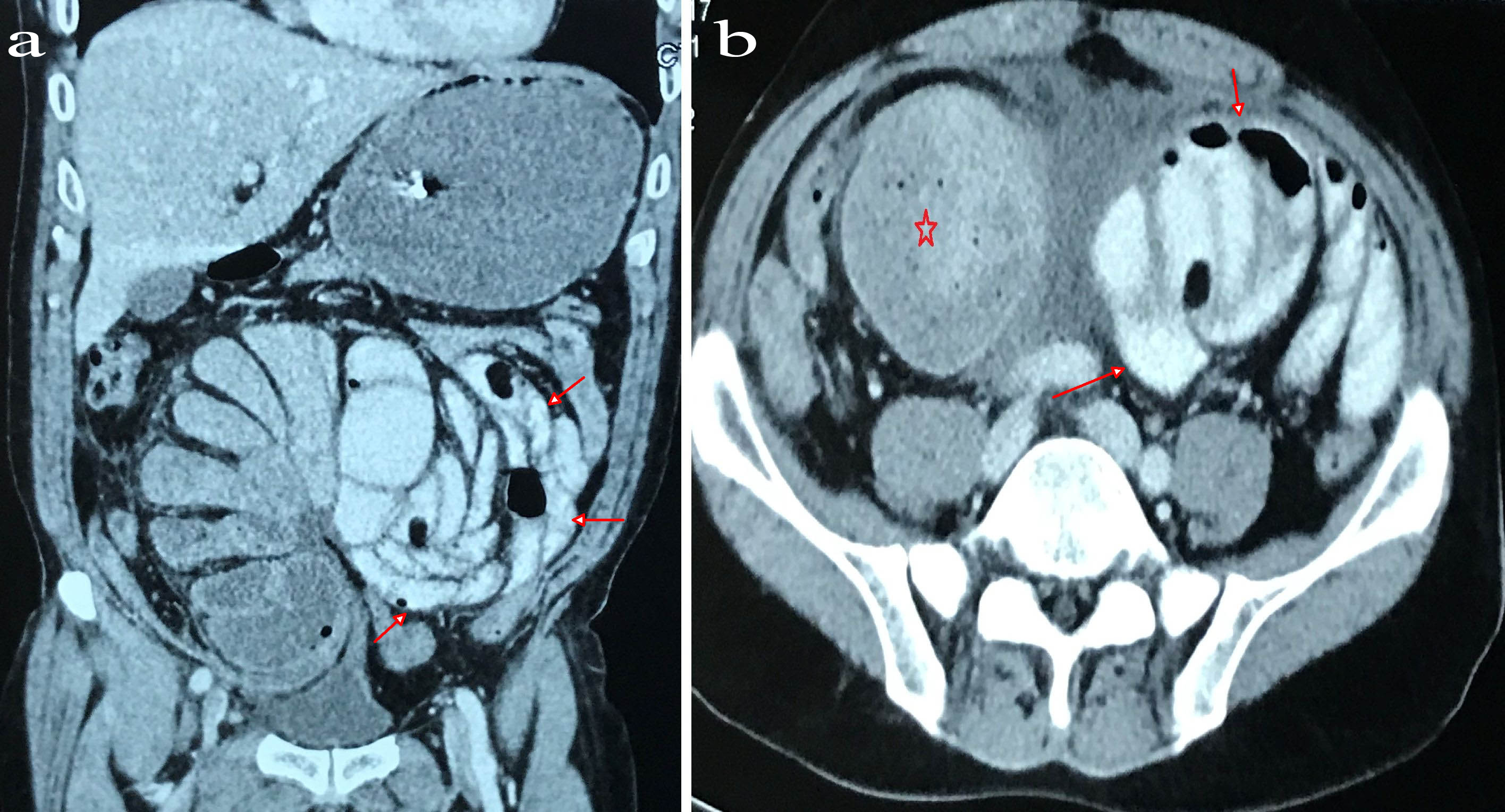
A 67-year-old man, a known hypertensive for five years, presented to emergency department with pain in abdomen, vomiting and without any bowel function for five days duration. He had a history of laxative use for chronic constipation. The patient denied any history of abdominal surgery or tuberculosis. On examination, his abdomen was distended with a tender lump (8 cm by 7 cm) present in the right iliac fossa. Laboratory investigation revealed leucocytosis (17,000 cells/ml) with normal serum chemistry and renal function test. Abdominal X-ray showed ground glass appearance with only few visible bowel loops inspite of obstruction [Table/Fig-1]. Further evaluation with contrast Computed Tomography (CT) abdomen, showed multiple clusters of small bowel loop in an enhancing membrane lying on left side of the abdomen. The terminal ileal loop was forming a well circumscribed lump (7 cm by 6 cm) containing fecal matter [Table/Fig-2(a,b)], suggesting a cocoon abdomen with fecaloma with underlying intestinal obstruction.
Abdominal X-ray (erect view) showing few prominent bowel loop with a ground glass appearance.

Contrast enhanced CT abdomen showing conglomerate of multiple small bowel loops on left side of abdomen within thick fibrous membrane (arrow). Evidence of fecaloma in terminal ileum (asterisk).
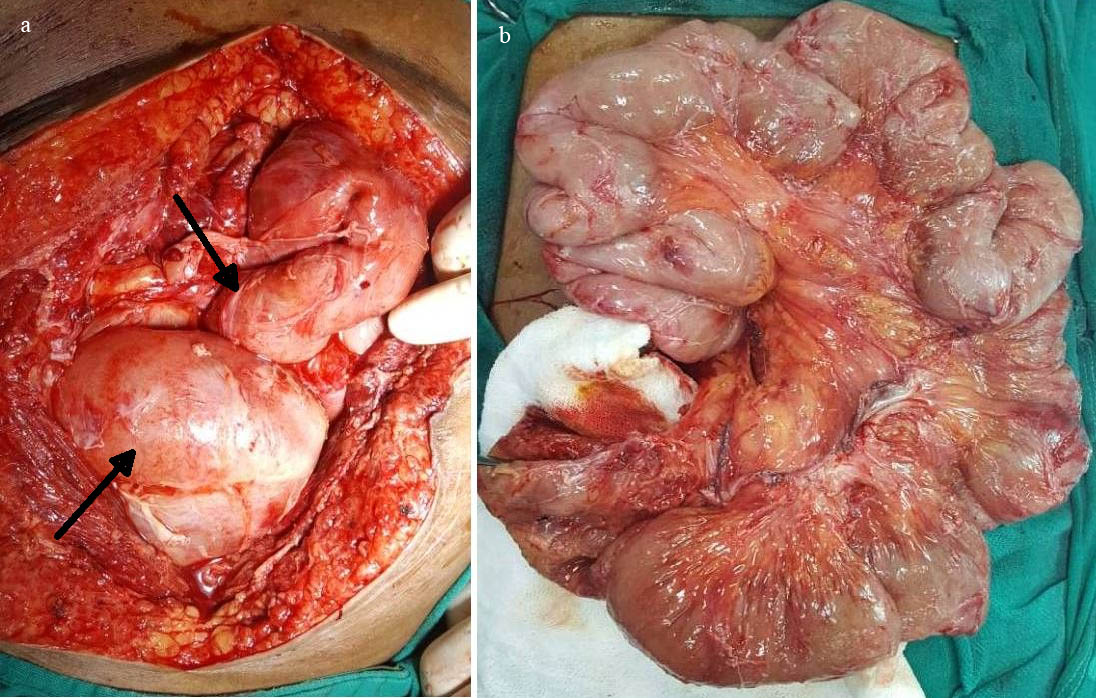
After resuscitation, patient subsequently was taken for laparotomy. Intraoperatively the entire small bowel from the jejunum to ileum was wrapped in a thick membrane in multiple segments (Type 2 abdominal cocoon). The membrane was dissected and released, and entire small bowel underwent adhesiolysis till terminal ileum [Table/Fig-3(a,b)]. The terminal ileum forming the membranous lump was the transition zone of obstruction and was showing patchy gangrenous changes, which was resected and anastomosed 8 cm proximal to the ileocaecal junction. On cut section, the ileum was folded on itself and contained solid feces (fecaloma). The resected ileum and membranes were sent for histopathological examination, which confirmed fibrocollagenous tissue with foci of lymphocytic infiltrates. No atypical cells were seen.
Intraoperative photograph showing small bowel entrapped within dense whitish membrane (arrow) forming cocoon (a). Image showing dilated, flabby bowel after release of membrane (b).
Over the next four days, the patient returned to normal bowel function and was discharged on seventh postoperative day. After 6 months of follow up, patient was doing well and was asymptomatic.
Discussion
The abdominal cocoon is a rare cause of intestinal obstruction most often seen in an adolescent girl from tropical and subtropical countries [1]. The exact aetiology of this entity is unknown. It was first described by Foo [2] in 1978 and is characterized by total or partial encasement of bowel by a thick fibrous membrane [3]. Similarly, fecaloma, a hard intraluminal tumour like mass of feces, which has been described in a setting of chronic constipation in colon in an old age patient, has rarely been reported for ileum [4]. The present case was unique and interesting with a rare combination of ileal obstruction due to fecaloma in a cocoon abdomen in an elderly male, diagnosed preoperatively by CT and managed successfully by surgery.
Abdomen cocoon most commonly are congenital or idiopathic in origin and mostly seen in young age patients [1]. It has also been reported in a four-year-old child and a premenarche girl from India and Saudia Arabia [5,6]. On contrary, in a large study of 65 patients from china by Li et al., the entity was commonly seen in middle age group patient with mean age of 39 years (range 14-79), and was seven times more common in the male population [7].
In an elderly population, the abdominal cocoon can be due to idiopathic or secondary cause. The secondary cause of origin may be due to tuberculosis (most commonly), intrabdominal malignancy, postoperative cases, primary peritonitis, peritoneal dialysis, liver transplantation, drugs (propranolol), liver cirrhosis, sarcoidosis, following abdominal trauma or any subclinical persistent intrabdominal infections [1,3].
In Eastern region of Nepal, tuberculosis followed by malignancy is the most likely secondary cause for the cocoon as people are chronically exposed to tuberculosis, being the endemic region for tuberculosis [8]. However, the biopsy turned out to be negative for both tuberculosis and malignancy suggesting idiopathic nature. It can be hypothesized that the multiple cocoon in our case was due to chronic constipation and stasis of small bowel leading to bacterial overgrowth which per se was the reason for persistent subclinical intrabdominal infection. Furthermore, the stasis with cocoon formation led to development of aperistaltic bowel segment and fecaloma in ileum, although commonly described for large bowel in a setting of megacolon [4].
Patient may be asymptomatic with cocoon abdomen if congenital. But most commonly, the presentation is non-specific or it may present with subacute to acute intestinal obstruction (80%) followed by lump abdomen (50%) due to clusters of bowel in membrane or solid feces in ileum forming fecaloma [9]. In the present case, the entire small bowel was wrapped in a fibrous membrane (type 2 abdominal cocoon) with an ileal fecaloma forming a lump and causing intestinal obstruction. Historically, diagnosis was made by barium study or at the time of laparotomy. But contrast CT if done preoperatively can suggest the presence of cocoon abdomen by presence of thick enhancing membrane and characteristic “cauliflower sign” where the bowel loops are arranged in a concertina shape [9,10]. Moreover, the fecaloma can be depicted on CT scan by hypodense mass lesion in ileum with presence of “mottled air” appearance.
Treatment is by meticulous excision of the peritoneal membrane and lysis of adhesion with or without resection of bowel containing fecaloma, without causing iatrogenic enterotomy and uncontrolled spillage of enteric content [1,9]. This may be the scenario in patients with cocoon due to tuberculosis or malignancy where the membranes are thick and the bowel is inflamed, densely adherent containing liquid enteric content. We were fortunate to have a distal ileum loaded with solid fecal content instead of being liquid, hence preventing the spillage of content.
Prognosis after surgery was excellent. Recurrence after surgery is rarely seen, and in one of the largest study of 24 cases found only 6% recurrence over a follow up period of 9 years which was managed with “suck and drip” method [1].
Conclusion
Intestinal obstruction due to abdominal cocoon and fecaloma in the ileum is a very rare situation. Contrast enhanced CT abdomen readily diagnoses the entity preoperatively. Management is best done by surgical approach by lysis of membrane with or without resection of fecaloma bearing segment.
[1]. Wei B, Wei HB, Guo WP, Zheng ZH, Huang Y, Hu BG, Diagnosis and treatment of abdominal cocoon: a report of 24 casesAm J Surg 2009 198:348-53.10.1016/j.amjsurg.2008.07.05419217609 [Google Scholar] [CrossRef] [PubMed]
[2]. Foo KT, Ng KC, Rauff A, Foong WC, Sinniah R, Unusual small intestinal obstruction in adolescent girls: the abdominal cocoonBr J Surg 1978 65:427-30.10.1002/bjs.1800650617656764 [Google Scholar] [CrossRef] [PubMed]
[3]. Ibrahim NA, oludara MA, Abdominal cocoon in an adolescent male patientTrop Doct 2009 39:254-56.10.1258/td.2009.09010419762590 [Google Scholar] [CrossRef] [PubMed]
[4]. Yoo HY, Park HW, Chang SH, Bae SH, Ileal Fecaloma presenting with small bowel obstructionPediatr Gastroenterol Hepatol Nutr 2015 18(3):193-96.10.5223/pghn.2015.18.3.19326473140 [Google Scholar] [CrossRef] [PubMed]
[5]. Rao PLNG, Mitra SK, Pathak IC, Abdominal cocoon- a cause of intestinal obstruction in a 4 -year -old girlIndian Pediatr 1979 16:1047-48. [Google Scholar]
[6]. Sahoo SP, Gangopadhyay AN, Gupta DK, Gopal SC, Sharma SP, Dash RN, Abdominal cocoon in children: a report of four casesJ Pediatr Surg 1996 31(1):987-88.10.1016/S0022-3468(96)90431-5 [Google Scholar] [CrossRef]
[7]. Li N, Zhu W, Li Y, Gong J, Gu L, Li M, Surgical treatment and perioperative management of idiopathic abdominal cocoon: single-center review of 65 casesWorld J Surg 2014 38(1):1860-67.10.1007/s00268-014-2458-624519587 [Google Scholar] [CrossRef] [PubMed]
[8]. Sharma V, Singh H, Mandavdhare HS, Tubercular Abdominal Cocoon: Systematic Review of an Uncommon Form of TuberculosisSurg Infect (Larchmt) 2017 18(6):736-41.10.1089/sur.2017.11028759335 [Google Scholar] [CrossRef] [PubMed]
[9]. Tannoury JN, Abboud BN, Idiopathic sclerosing encapsulating peritonitis: Abdominal cocoonWorld J Gastroenterol 2012 18(17):1999-2004.10.3748/wjg.v18.i17.199922563185 [Google Scholar] [CrossRef] [PubMed]
[10]. Basu A, Sukumar R, Sistla SC, Jagdish S, "Idiopathic" abdominal cocoonSurgery 2007 141:277-78.10.1016/j.surg.2005.12.00417299859 [Google Scholar] [CrossRef] [PubMed]