Invasive Breast Carcinoma with Axillary Tuberculous Lymphadenitis
Sunil V Jagtap1, Ravindra G Naniwadekar2, Cyrus Dara Jokhi3, Swati Sunil Jagtap4
1 Professor, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
2 Professor, Department of Surgery, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
3 Assistant Lecturer, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
4 Associate Professor, Department of Physiology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil V Jagtap, Professor, Department of Pathology, Krishna Institute of Medical Sciences, Karad-415110, Maharashtra, India.
E-mail: drsvjagtap@gmail.com
The simultaneous occurrence of breast cancer and tuberculosis is rare. As there are no pathognomic clinical signs and symptoms, it can create problem in diagnosis and treatment of both diseases. A 50-year-old female patient presented with right breast lump diagnosed on histopathology as invasive breast carcinoma Grade III, with extensive granulomatous right axillary lymphadenitis due to tuberculosis. Thus, diagnosis helps in down staging of carcinoma of breast and further management of the case.
Breast lump, Malignant breast lesion, Matted lymph node
Case Report
A 50-year-old female patient presented to surgical oncology unit with right breast lump of three month duration. Lump was gradually increased in size with mild tenderness. It was associated with fever and axillary lymphadenitis. Clinical examination revealed single, large, hard, fixed right breast lump measuring approximately 3.5×2.5×2 cm. The nipple was retracted and surrounding skin was inflamed. There was no history of nipple discharge. The contra-lateral breast was normal. Right axilla showed 3.5×2.5×2 cm mass with variable nodules. There was no significant family history. She had history of tuberculosis 30 years back and had completed the treatment.
Her systemic examination was normal. Her routine investigations showed mild anaemia, mild lymphocytosis, raised Erythrocyte sedimentation rate (ESR). Biochemical parameters were normal. Radiological study showed normal chest X-ray, and ultrasonography of abdomen-pelvis. On mammography, right breast showed irregular increased density mass lesion with foci of multiple calcifications [Table/Fig-1]. It was suspected case of malignant breast lesion.
Right breast showed irregular increased density mass lesion with foci of calcifications.
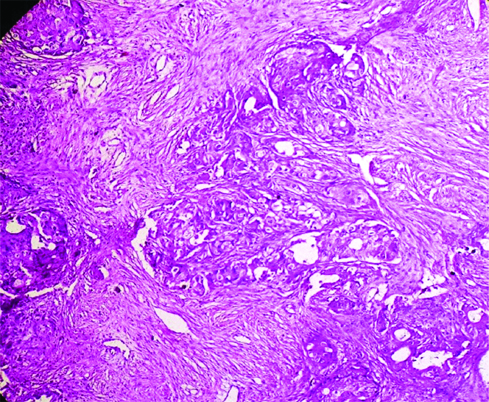
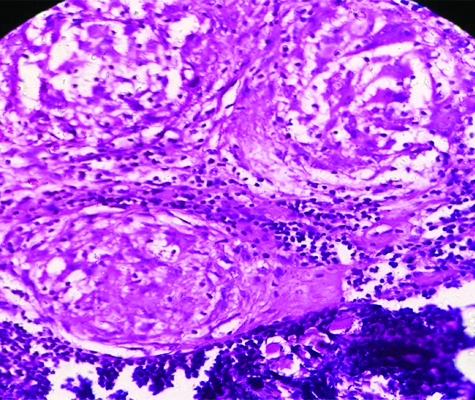
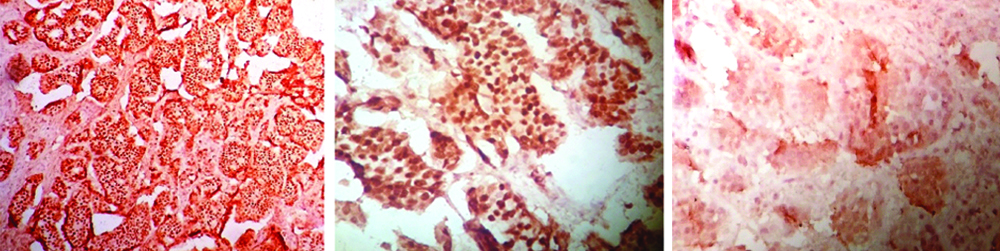
Fine needle aspiration cytology showed positive for duct carcinoma cells. Patient underwent modified radical mastectomy with axillary clearance. The specimen was sent for histopathological examination. The gross specimen of right modified radical mastectomy measured 28×21×4 cm and weighed 1200 g. Skin was unremarkable and measured 11×5 cm. On cut section, breast specimen showed a tumour mass measuring 3.5×2.1×2 cm situated in central retro-areolar region. The tumour was irregular, grey white, firm to hard [Table/Fig-2,3]. Right axillary dissection revealed 16 lymph nodes. Larger lymph node measured 1.8 cm. On cut section, caseation necrosis was noted. The Ziehl-Neelsen (ZN) stain (20%) showed numerous acid fast Bacilli in lymph node section. On microscopy revealed invasive breast carcinoma (NOS) Grade III (Modified RB score of 2+3+3=8), with DCIS-solid cribriform pattern of right breast and right axillary tuberculous lymphadenitis [Table/Fig-4,5,6 and Table/Fig-7]. There was no evidence of any metastasis in axillary lymph nodes. On immunohistochemistry study tumour was positive for Estrogen Receptors (ER) and Progesterone Receptors (PR) and negative for Human Epidermal Growth Factor Receptor 2 (HER-2/Neu) [Table/Fig-8-10].
Gross right modified radical mastectomy specimen cut section showing tumour and caseating lymph nodes.

Photomicrograph showing invasive breast carcinoma (Haematoxylin and Eosin, 40X).
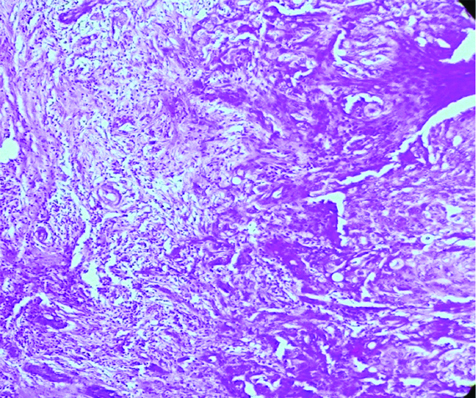
Photomicrograph showing invasive breast carcinoma (Haematoxylin and Eosin, 100X).
Photomicrograph showing lymph node with multiple granulomas (Haematoxylin and Eosin, 40X).
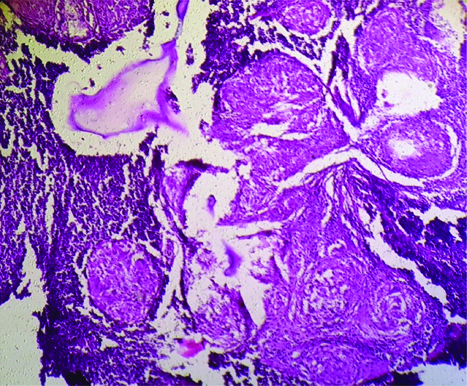
Photomicrograph showing lymph node with multiple caseation granulomas (Haematoxylin and Eosin, 100X).
Showing ER, PR positivity and HER-2/Neu negativity.
The patient received treatment of surgical excision by modified radical mastectomy, followed by four cycles of chemotherapy consisting of two drugs regimen (Adriamycin and Cyclophosphamide) each cycle after 21 days. Second regimen of paclitaxel was started. Patient was given antituberculosis drugs. The specific nutritional care and regular follow-up was advised.
Discussion
Tuberculosis is a major public health problem and estimated to affect one third of the world population with most in developing countries. The co-existence of breast carcinoma and tuberculosis may occur rarely. The pathology may be present as carcinoma of breast with tuberculous mastitis, carcinoma in the breast with axillary tuberculous lymphadenitis or both [1]. Though rare, both are major diseases and may reach to problem in diagnosing as well as management of cases. We report a case of invasive breast carcinoma with axillary tuberculous lymphadenitis, wherein no evidence of tuberculosis was found elsewhere.
The co-existence of carcinoma of breast and tuberculosis of axillary lymph node is rare and was first described in 1899 by Warthin AS [2]. Tuberculous mastitis accounts for only 0.1% of cases even in developed countries where tuberculosis is common [3]. Co-existence of tuberculosis and malignancy have been reported in various organs [4,5].
Most patient with tuberculous mastitis present with well defined hard mass which may be associated with diffuse nodularity, nipple retraction, skin fistula fixation to skin and underlying tissues [6].
The simultaneous occurrence of carcinoma and tuberculosis can lead to difficulties regarding diagnosis and treatment as there are no pathognomic symptoms and signs to distinguish breast tuberculosis from breast carcinoma especially if the upper outer quadrant is involved [1,4].
In a study by Kalpan MH et al., among 14,782 cases of breast cancer, 28 cases had co existing tuberculosis with the breast cancer [7]. Ballini A et al., observed that on clinical presentation it is difficult to distinguish both the diseases [6]. As in both situation patient present with breast lump, fever, anorexia, weight loss and axillary lymphadenitis. Few cases may present with sinus formation. It is essential to look for the presence of granulomas with or without necrosis in association with malignancies particularly in geographical regions with a high prevalence of tuberculosis, for the possibility of coexistent tuberculosis [8].
Axillary lymph node enlargement in breast cancer patients may not always point to a metastatic disease. In the present case, there was significant right axillary adenopathy. On axillary clearance 16 lymph nodes were microscopically detected. All showed extensive caseation necrosis with granuloma formation and on ZN stain (20%) showed numerous acid fast bacilli. Interestingly there was no evidence of metastasis of breast carcinoma. Thus, histopathological diagnosis has helped in down staging of the carcinoma of the breast. Primary axillary lymph node involvement by tuberculosis in adult is uncommon. In present case, at present, there was no evidence of any systemic tuberculosis. The existence of invasive breast carcinoma and tuberculous mastitis may arise in clinical situation when patient present with lump in breast and associated with axillary lymphadenopathy. It is a diagnostic and therapeutic challenge [9,10].
There is no clear consensus on initiation and the duration of anti-tuberculosis therapy and its association with chemotherapy. Alzaraa A et al., recommend that a mastectomy should be performed for operable breast cancer followed by 18 months of anti-tuberculosis therapy [11]. To avoid effect of immunosupression, the chemotherapy is recommended after four weeks of anti-Tuberculosis therapy.
Conclusion
The present case was a rare case of carcinoma breast with tuberculous axillary lymphadenitis which was presented for its clinical and pathological significance. Axillary lymph node enlargement in breast cancer patient may not be a metastatic tumour. So, careful evaluation of lymph nodes for evidence of tuberculosis will be helpful for proper diagnosis and staging in such cases of breast cancer.
[1]. Tulasi N, Raju P, Damodharan V, Radhika TS, A spectrum of co existent tuberculosis and carcinoma of the breast and axillary lymph node: report of five casesThe Breast 2006 15:437-39.10.1016/j.breast.2005.07.00816198111 [Google Scholar] [CrossRef] [PubMed]
[2]. Warthin AS, The coexistence of Tuberculosis and carcinoma of the mammary glandAm J Med Sci 1899 118:2510.1097/00000441-189907000-00003 [Google Scholar] [CrossRef]
[3]. Chottanapau S, Wongtawatchai P, Tuberculous axillary lymphadenitis co existing in patient with invasive carcinoma of breast-a case reportThai Journal of Surgery 2004 25:121-24. [Google Scholar]
[4]. Pandey M, Abraham EK, Chandramohan K, Rajan B, Tuberculosis and metastatic carcinoma coexistence in the axillary lymph node: a case reportWorld J Surg 2003 1:310.1186/1477-7819-1-3PMC156028 [Google Scholar] [CrossRef] [PubMed]
[5]. Desai S, Jagtap S, Janugade H, Coexisting tuberculosis and mucinous adenocarcinoma caecumMed Jr Armed Force India 2005 61:197-99.10.1016/S0377-1237(05)80028-0 [Google Scholar] [CrossRef]
[6]. Ballini A, Zaritzky A, Lupol: breast tuberculosis and carcinomaIsr Med Sci 1989 25:339-40. [Google Scholar]
[7]. Kaplan MH, Armstrong D, Rosen P, Tuberculosis complicating neoplastic disease: a (review of 201 cases)Cancer 1974 33:850-33.10.1002/1097-0142(197403)33:3<850::AID-CNCR2820330334>3.0.CO;2-H [Google Scholar] [CrossRef]
[8]. Khurram M, Tariq M, Shahid P, Breast cancer with associated granulomatous axillary lymphadenitis: a diagnostic and clinical dilemma in region with high prevalence of tuberculosisPathology-Research and Practice 2007 203:699-704.10.1016/j.prp.2007.07.00417826003 [Google Scholar] [CrossRef] [PubMed]
[9]. Bani-Hani KE, Yaghan RJ, Matalka II, Mazahreh TS, Tuberculosis mastitis: a disease not to be forgottenInt J Tuber Lung Dis 2005 9(8):920-25. [Google Scholar]
[10]. Akcay MN, Saglam L, Polat P, Erdoğan F, Albayrak Y, Povoskı SP, Mammary tuberculosis. Importance of recognition and differentiation from that of a breast malignancies: report of three cases and review of the literatureWorld J Surg Onco 2007 5:6710.1186/1477-7819-5-6717577397 [Google Scholar] [CrossRef] [PubMed]
[11]. Alzaraa A, Dalal N, Coexistence of carcinoma and tuberculosis in one breastWorld J Surg Oncol 2008 6:2910.1186/1477-7819-6-2918318914 [Google Scholar] [CrossRef] [PubMed]