Sciatic Nerve Schwannoma at Sciatic Foramen: Importance of Transvaginal Sonography Guided Biopsy and Magnetic Resonance Imaging in its Diagnosis
Puneet Garg1, Anirudh Chawla2, Rajeev Malhotra3, Bhawna S Narula4, Anuj Thakral5
1 Assistant Professor, Department of Radiodiagnosis, VMMC and Safdarjung Hospital, New Delhi.
2 Senior resident, Department of radiodiagnosis, Max superspeciality hospital, Shalimar bagh, New Delhi.
3 Senior consultant and head, Department of radiodiagnosis, Max superspeciality hospital, Shalimar bagh, New Delhi.
4 Senior consultant, Department of pathology, Max superspeciality hospital, Shalimar bagh, New Delhi.
5 Consultant, Department of Radiodiagnosis, Max superspeciality hospital, Shalimar bagh, New Delhi.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Puneet Garg, 40C MIG, DDA Flats, Motia Khan, Paharganj, New Delhi-110055.
E-mail: drpuneet06@gmail.com
Schwannomas are truly encapsulated benign tumours associated with the nerves arising from the schwann cells. Schwannomas arising from the sciatic nerve is of rare occurrence and is estimated to be less than one in hundred cases of schwannomas detected. Generally sciatic nerve schwannomas symptomatically mimic sciatica due to herniated disc or sometimes it may be asymptomatic and incidentally detected. In this case report, we are describing a case of asymptomatic middle aged female patient, who is a follow up case of hysterectomy and bilateral salpingo-oophorectomy for a gyanecological malignancy around 5 years back. During routine follow up sonography (TVS), a mass was detected deep within the pelvis, which was further investigated with MRI and found to be a possible nerve sheath tumour of sciatic nerve at the left sciatic foramen. Further TVS guided biopsy and histopathological correlation, confirmed it to be an ancient schwannoma (neurilemmoma).
Hysterectomy, Nerve, Retroperitoneal, Sciatica, Vagina
Case Report
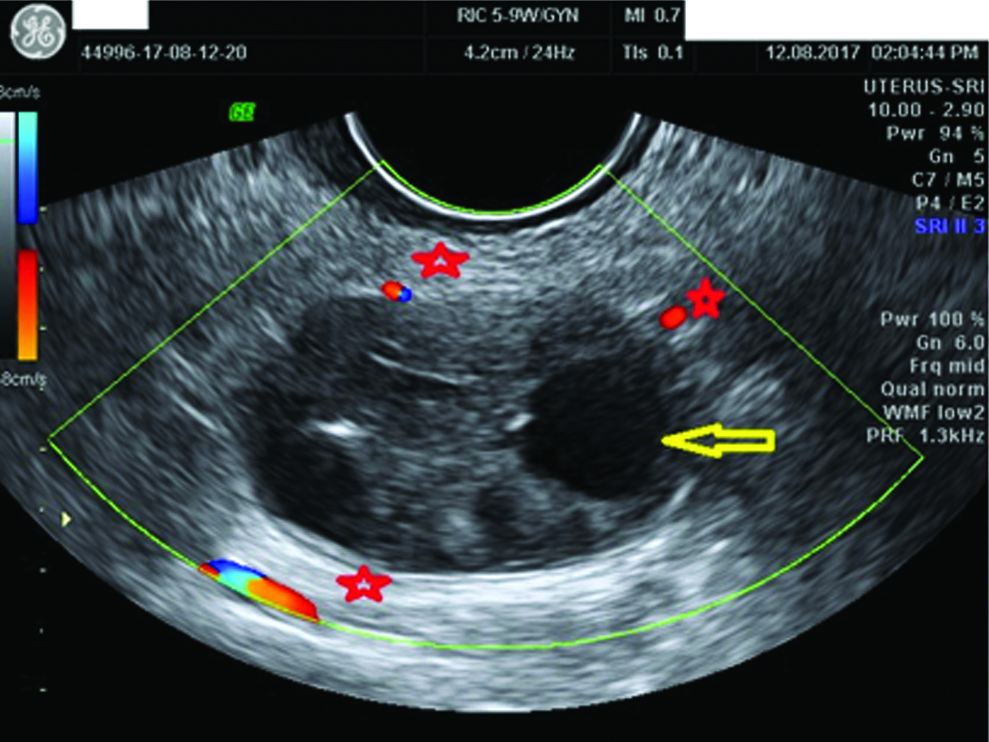
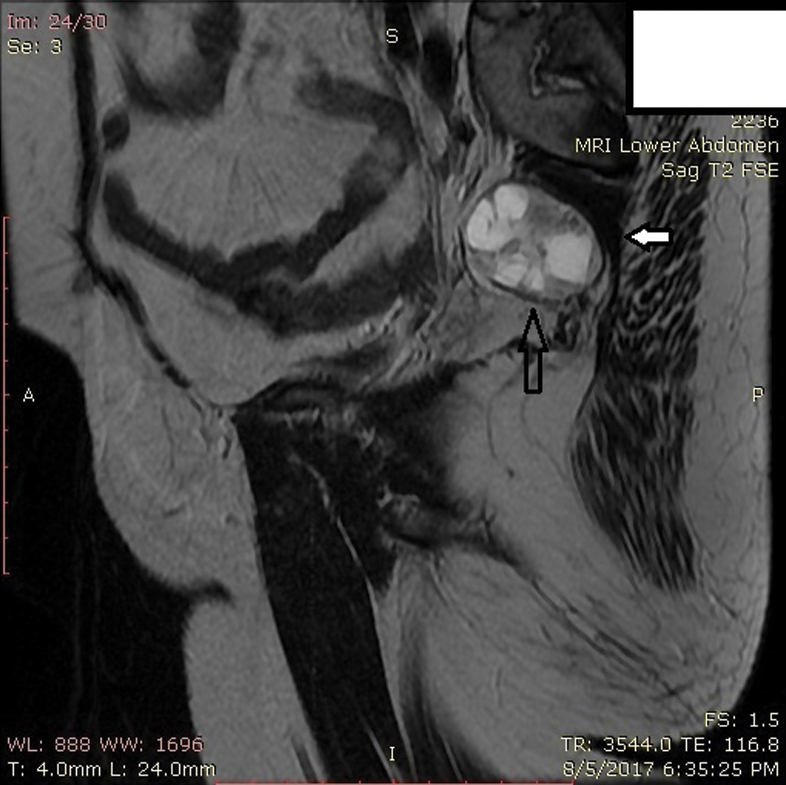
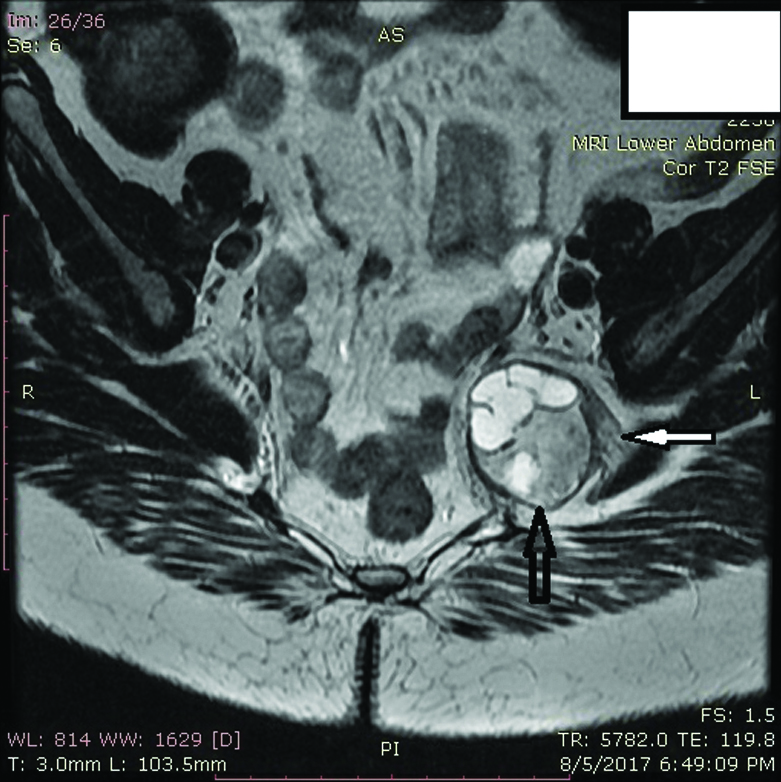
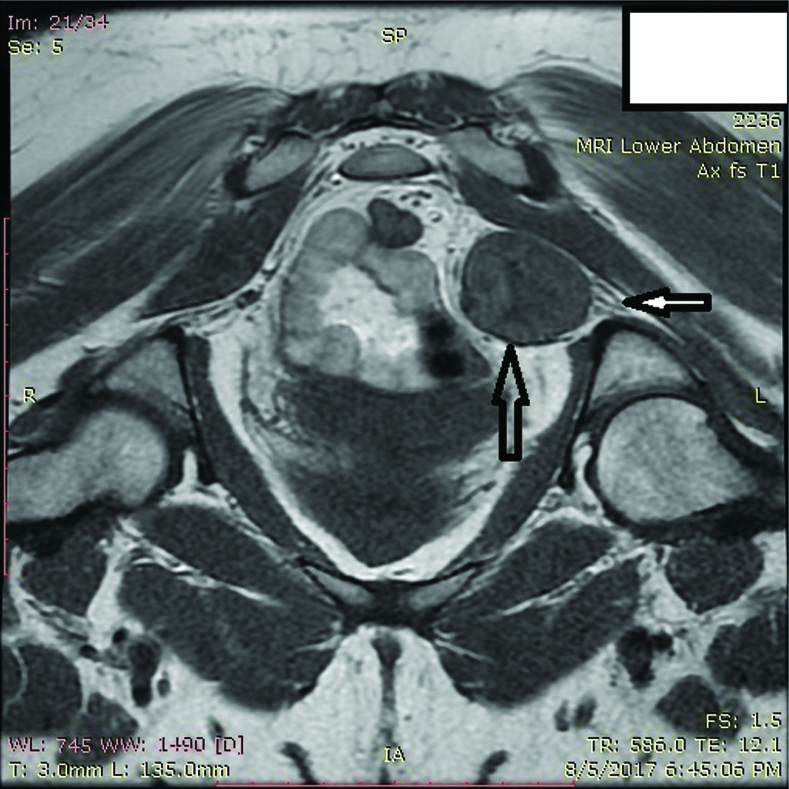
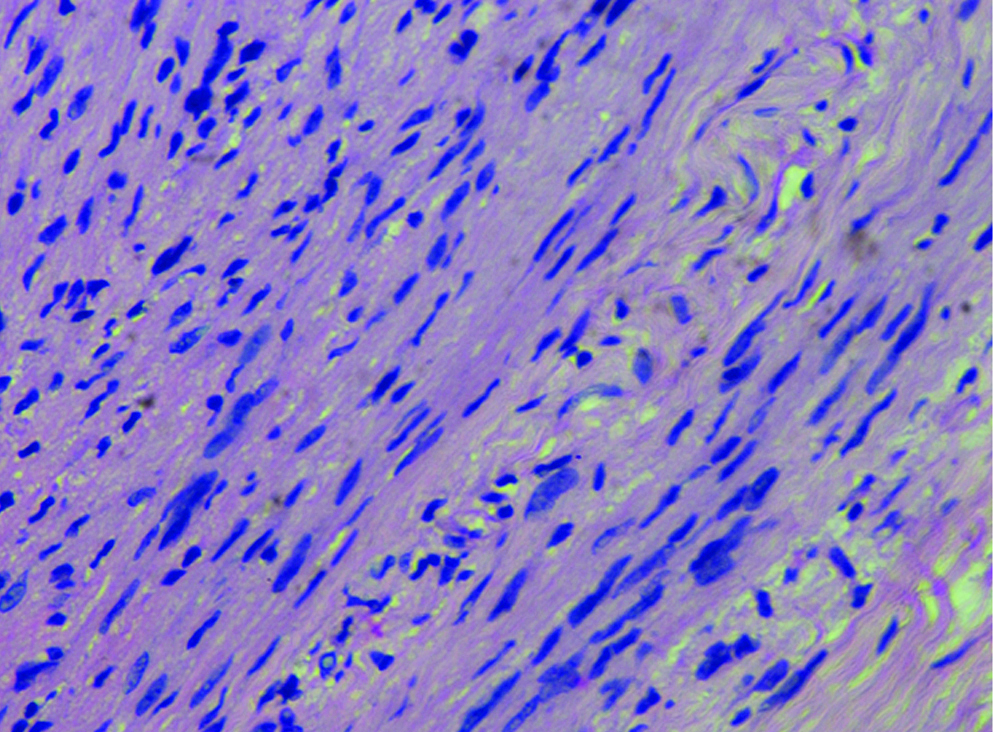
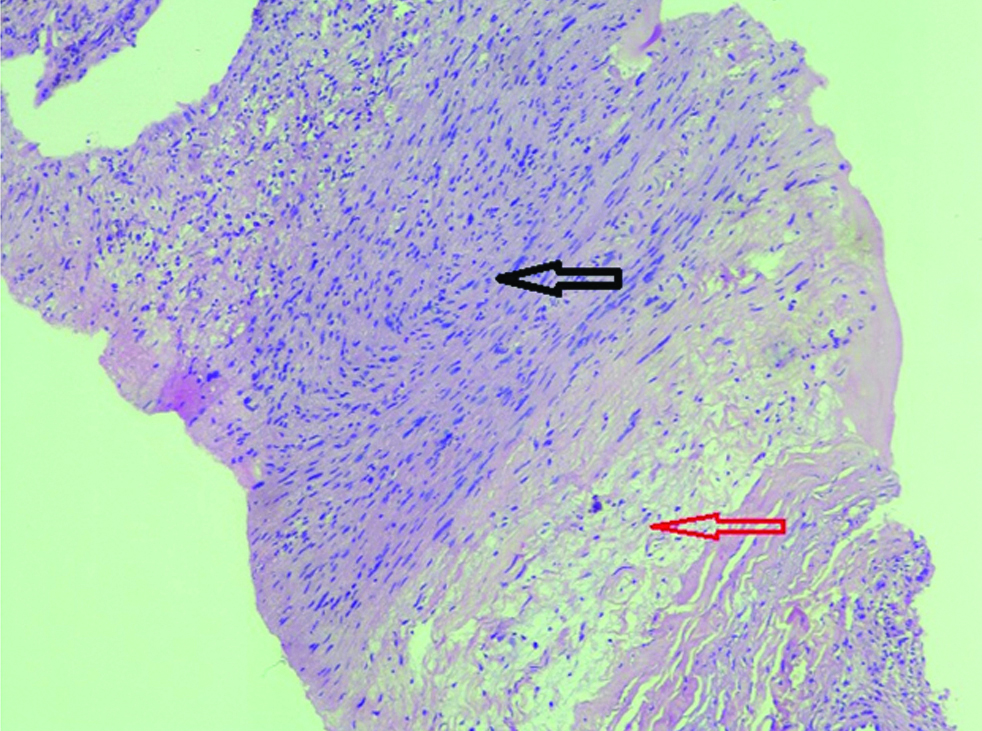
A 55-year-old female patient, who was a follow up case of an unknown gynaecological malignancy treated with hysterectomy and bilateral salpingo-oophorectomy was on a routine follow up for last 5 years. On TVS, there is an incidentally detected rounded soft tissue mass with internal cystic spaces along the left side of the pelvis, approximately 5cm deep to the vaginal fornix [Table/Fig-1]. The lesion is not in the expected location of the left ovary or adnexa and appears to be much deeper. Possibility of a retroperitoneal mass lesion was considered. Patient underwent non contrast MRI of the pelvis to characterize the lesion detected on ultrasound and it was found to be a 3.0 x 3.0 cm lesion appearing heterogeneously hyperintense on T2WI with well defined more hyperintense areas consistent with cystic spaces. The lesion appears heterogeneously hypointense on T1WI. The lesion is seen at left sciatic foramen abutting the left sciatic nerve [Table/Fig-2,3 and 4]. Provisional diagnosis of nerve sheath tumour was made and decision was made to biopsy the lesion. Patient was offered image guided biopsy either using CT or TVS. After explaining the procedure and possible complications, patient consented for TVS guided biopsy. After initial preprocedure investigations including platelet count, PT/INR, viral markers which were within normal range, patient was given prophylactic antibiotics two days prior to the procedure. Under mild intravenous sedation, patient was positioned in lithotomy position on the examination couch. After probe preparation using sterile probe cover and lignocaine jelly to a high frequency TVS probe (9Mhz), disposable biopsy guide was attached to the probe. After locating the lesion on left side of the pelvis and selecting the best possible trajectory without any intervening small bowel loops and major vessels, 10ml of 1% lignocaine was infiltrated into the vaginal mucosa and along the path of the biopsy needle using 20 G chiba needle. A 16 G tru cut biopsy needle was used to take multiple passes from the lesion and the sample was stored in 4% formalin container. Vaginal packing was done post procedure to control any bleeding. Patient complained of mild shooting pain along the left thigh which was managed conservatively using oral non steroidal anti-inflammatory drugs. Antibiotics were continued for three more days. On histopathological analysis of the biopsied specimen, there were uniform spindle cells with ill-defined cytoplasm and dense chromatin along with verocay bodies [Table/Fig-5]. The tumour also shows mixed areas of hypocellular myxoid tissue (antoni B) with areas of cellularity (antoni A) [Table/Fig-6] which confirmed the diagnosis of a schwannoma.
Transvaginal ultrasound image of the lesion with colour flow showing well defined rounded lesion with internal cystic anechoic areas (yellow arrow)) with surrounding vascularity (marked with red stars) and negligible internal vascularity.
Saggital T2 FSE image showing a well defined solid cystic mass lesion in left sciatic foramen (black arrow) located just beneath the left piriformis muscle (white arrow).
Coronal T2FSE image of the pelvis shows the mass lesion (black arrow) in relation to the left sciatic nerve fibres (white arrow).
Axial T1 FSE image of the pelvis (prone) showing the hypointense lesion in left sciatic foramen (black arrow) in relation to the sciatic nerve (white arrow).
H&E; 400x : Uniform spindle cells with ill-defined cytoplasm and dense chromatin along with verocay bodies.
H&E; 100x: Tumour showing cellular fascicular (antoniA) areas (black arrow) and hypocellular (antoniB) myxoid areas (red arrow) consistent with a schwannoma.
Discussion
Schwannomas are benign, encapsulated, slow growing tumours arising from the schwann cells of the nerves which are responsible for myelin formation. Generally Schwannomas arise eccentrically from a nerve unlike in neurofibroma which is engulfed by the nerve fibre [1]. In this case report, we have described about sciatic nerve schwannoma located in the sciatic foramen, which is of rare occurrence and has been described in the literature by few authors [2,3]. According to the literature, these sciatic foraminal lesions can be purely intrapelvic, extrapelvic or both intra and extrapelvic [2].
These schwannomas can be asymptomatic or can cause compression upon the sciatic nerve thereby producing symptoms of thigh and calf pain or sensory disturbances [4]. As in our case, intratumoral cystic degeneration is more common in schwannomas than neurofibromas [5]. Ancient schwannomas are a rare variant which shows cystic degeneration and reduced cellularity owing to decreased Antoni A cells and increased Antoni B cells. Ancient schwannomas are generally located deep within the pelvis and are usually asymptomatic unless they attain a large size. Other MRI characterstics are intratumoral haemorrhage, calcification and peripheral contrast enhancement [6].
In our case, the lesion was detected and biopsied using TVS guidance. Transvaginal sonography has been traditionally used in evaluating lesions of uterus and adnexae because of good resolution of the probes and small field of view, giving greater clarity to the image. For similar reasons TVS can be used in evaluating non gynaecologic lesions in the pelvis. Owing to the predictable orientation and close proximity of different anatomic structures within the pelvis, different structures that can be seen are distal ureters, bladder, urethra, rectum, sigmoid colon, ileal loops, pelvic vasculature, retroperitoneal structures and pelvic sidewall. Slight modification in probe position and anatomic knowledge of different structures is required to visualize and characterize lesions arising 2from different structures as forementioned above [7]. TVS has also been used by many researchers in the past for biopsy of deep seated pelvis mass lesions [8-10]. Volpi and Park et al., reported diagnostic accuracy of TVS guided biopsy as 95% and 93% respectively [8,9] while Faulkner et al., reported the accuracy as 86% [11]. TVS guided biopsy for deep seated pelvic lesions is more justified because of various reasons like: 1) Real time visualization of the lesion and the needle; 2) Simultaneous colour doppler monitoring to avoid major vascular structures in the needle path; 3) Close proximity of the pelvic lesions to the endovaginal probe; 4) No radiation involved and wider availability [12].
Haemorrhage is not a serious complication during this procedure which can be due to avoidance of larger pelvic vessels along the pelvic sidewall and can be a problem during CT guided biopsies [12]. Vaginal bleeding can be controlled by vaginal packing after the procedure.
We administered prophylactic antibiotics but infection seems to be not a serious and frequent complication as different authors did not use the antibiotics in their patients and neither did they observe any infection after the procedure [9,13].
We could not find any other case reported in the literature about diagnosing and biopsy of the sciatic foramen lesion using transvaginal ultrasonography.
Regarding the surgical management of these lesions, these tumours can be approached via posterior infragluteal incision or transgluteal incision [14]. These two approaches are mainly for the extrapelvic lesions. For intrapelvic lesions, anterior transabdominal approach [15] and combined transabdominal and transgluteal approach has been reported [2]. Generally these tumours are completely resected with complete resolution of symptoms but patient in our study did not undergo surgery since she was explained about the benign nature of the lesion and moreover she was asymptomatic.
Conclusion
Diagnosing and biopsy of the lesion using transvaginal sonography is unique to this article and has not been heard of in the literature so far. Sciatic nerve schwannoma is a known clinical entity which should be kept in mind whenever patient is complaining of sciatica like symptoms in the absence of significant degenerative lumbar disc disease. Transvaginal sonography guided biopsy is another safe alternative for diagnosing such lesions.
[1]. Beaman FD, Kransdorf MJ, Menke DM, Schwannoma: radiologic-pathologic correlationRadioGraphics 2004 24(5):1477-81.10.1148/rg.24504500115371621 [Google Scholar] [CrossRef] [PubMed]
[2]. Spinner RJ, Endo T, Amrami KK, Dozois EJ, Babovic-Vuksanovic D, Sim FH, Resection of benign sciatic notch dumbbell-shaped tumorsJ Neurosurg 2006 105(6):873-80.10.3171/jns.2006.105.6.87317405258 [Google Scholar] [CrossRef] [PubMed]
[3]. Haspolat Y, Ozkan FU, Turkmen I, Kemah B, Turhan Y, Sarar S, Sciatica due to Schwannoma at the Sciatic NotchCase Rep Orthop 2013 2013:510901Available fromhttp://dx.doi.org/10.1155/2013/51090110.1155/2013/51090123762699 [Google Scholar] [CrossRef] [PubMed]
[4]. Tan LA, Bradbury J, Bonnin J, Horn EM, Minimally invasive resection of an extrapelvic sciatic schwannomaJ Clin Neurosci 2010 (10):1314-16.10.1016/j.jocn.2009.12.03120594852 [Google Scholar] [CrossRef] [PubMed]
[5]. Kakkar C, Shetty CM, Koteshwara P, Bajpai S, Telltale signs of peripheral neurogenic tumors on magnetic resonance imagingThe Indian Journal of Radiology & Imaging 2015 25(4):453-58.10.4103/0971-3026.16944726752825 [Google Scholar] [CrossRef] [PubMed]
[6]. Shanbhogue AK, Fasih N, Macdonald DM, Sheikh AM, Menias CO, Prasad SR, Uncommon primary pelvic retroperitoneal masses in adults: a pattern-based imaging approachRadio Graphics 2012 31(3):795-817.10.1148/rg.32311502022582360 [Google Scholar] [CrossRef] [PubMed]
[7]. Chang TS, Bohm-Velez M, Mendelson EB, Non-gynecological applications of transvaginal sonographyAJR 1993 160(1):87-93.10.2214/ajr.160.1.84166558416655 [Google Scholar] [CrossRef] [PubMed]
[8]. Volpi E, Zola P, De Grandis T, Rumore A, Volpe T, Sismondi P, Transvaginal sonography in the diagnosis of pelvic malignant recurrence: integration of sonography and needle-guided biopsyUltrasound Obstet Gynecol 1994 4(2):135-38.10.1046/j.1469-0705.1994.04020135.x12797207 [Google Scholar] [CrossRef] [PubMed]
[9]. Park J, Kim C, Park B, Ultrasound-guided transvaginal core biopsy of pelvic masses: feasibility, safety, and short-term follow-upAmerican Journal of Roentgenology 2016 206(4):877-82.10.2214/AJR.15.1570226913556 [Google Scholar] [CrossRef] [PubMed]
[10]. Plett SK, Poder L, Brooks RA, Morgan TA, Transvaginal ultrasound-guided biopsy of deep pelvic massesJ Ultrasound Med 2016 35(6):1113-11.10.7863/ultra.15.0800227091918 [Google Scholar] [CrossRef] [PubMed]
[11]. Faulkner RL, Mohiyiddeen L, McVey R, Kitchener HC, Transvaginal biopsy in the diagnosis of ovarian cancerBJOG 2005 112(7):991-93.10.1111/j.1471-0528.2005.00619.x15958006 [Google Scholar] [CrossRef] [PubMed]
[12]. Gupta S, Nguyen HL, Morello FA Jr, Ahrar K, Wallace MJ, Madoff DC, Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: Anatomic and technical considerationsRadioGraphics 2004 24(1):175-89.10.1148/rg.24103506314730045 [Google Scholar] [CrossRef] [PubMed]
[13]. O’Neill MJ, Rafferty EA, Lee SI, Arellano RS, Gervais DA, Hahn PF, Transvaginal interventional procedures: aspiration, biopsy, and catheter drainageRadiographics 2001 21(3):657-72.10.1148/radiographics.21.3.g01ma2065711353114 [Google Scholar] [CrossRef] [PubMed]
[14]. Montano N, Novello M, D’Alessandris QG, Magarelli N, Pallini R, Lauriola L, Intrapelvic sciatic notch schwannoma: microsurgical excision using the infragluteal approachJ Neurosurg 2013 119(3):751-55.10.3171/2013.3.JNS12116123581593 [Google Scholar] [CrossRef] [PubMed]
[15]. Consales A, Poppi M, Stumpo M, Sciatic schwannoma spanning the sciatic notch: removal by an anterior, transabdominal approachBr J Neurosurg 2006 20(1):46-48.10.1080/0268869060060377616698610 [Google Scholar] [CrossRef] [PubMed]