Tracheal Schwannoma: An Uncommon Entity
Zeeshanuddin Ahmad1, Sanjay M Desai2, Amar Jain3, Deepak Agrawal4
1 Senior Resident, Department of Surgical Oncology, Sri Aurobindo Institute of Medical Sciences, Indore, India.
2 Professor and Head, Department of Surgical Oncology, Sri Aurobindo Institute of Medical Sciences, Indore, India.
3 Senior Resident, Department of Surgical Oncology, Sri Aurobindo Institute of Medical Sciences, Indore, India.
4 Professor, Department of Surgical Oncology, Sri Aurobindo Institute of Medical Sciences, Indore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanjay M Desai, Professor and Head, Department of Surgical Oncology, Sri Aurobindo Institute of Medical Sciences, Indore-452001, India.
E-mail: zee_kmc03@rediffmail.com
Primary tracheal tumours are extremely rare with most of them being malignant. Histologically, both primary tracheal tumours and main stem tumours are similar but the former is about 100 times less common than the latter. Primary neurogenic tumours of trachea account for only about 9% of all neoplasms of trachea. Tracheal schwannoma is the rarest of all neurogenic tumours and there is no unanimous opinion regarding line of treatment. They are usually seen in females and their clinical features are not specific. Chronic cough, progressive respiratory distress and sometimes asthma-like symptoms prevail as the presenting complaints. The reported patient had completely obstructing right endobronchial tumour extending in lower third of trachea. Pneumonectomy along with sleeve excision of trachea with hilar dissection was done.
Bronchoscopy, Neurogenic, Pneumonectomy
Case Report
A 34-year-old lady presented with breathlessness for one and half year, cough with expectoration for five months, two episodes of haemoptysis three months back, pain in right side of chest for two months. She was a mother of four children, all born with normal vaginal delivery. Physical examination revealed decreased chest movements and air entry on right side, wheeze on exertion and mild pallor. She was admitted and thoroughly investigated. CECT scan [Table/Fig-1] of chest revealed:
CECT chest: Large endobronchial tumour with hilar lymphadenopathy. Cardiomediastinum and trachea shifted to diseased side. Collapse consolidation of right lung.
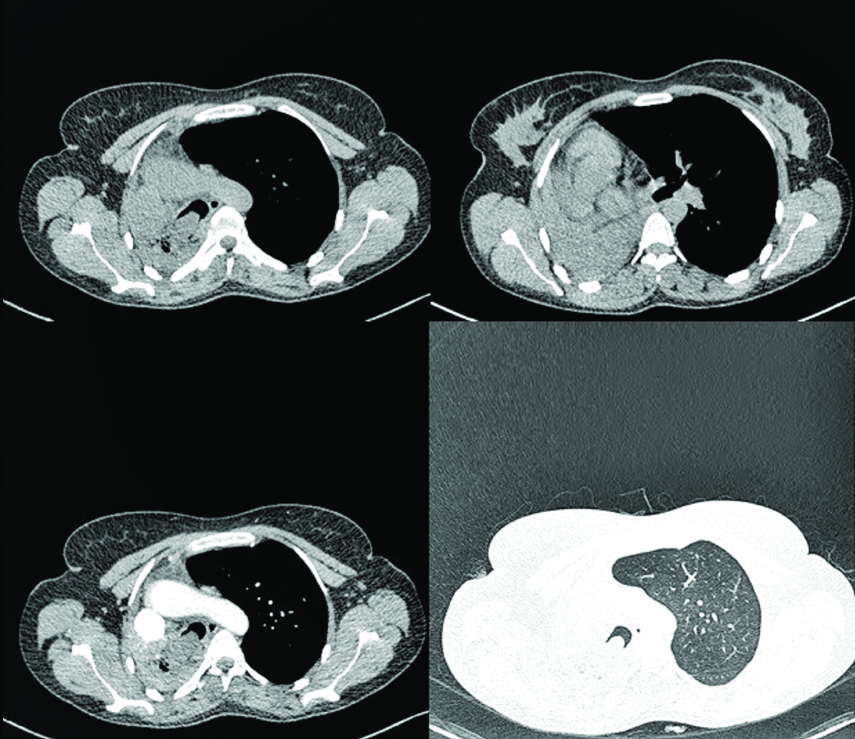
1. Right endobronchial, endotracheal mass with collapse consolidation of right lung. Cardiomediastinum and trachea is shifted towards right side. Right diaphragm is pulled up. Left lung is hyperinflated. Small patch of consolidation is seen in lingular segment of left upper lobe.
2. Multiple enlarged pretracheal, right paratracheal and right hilar lymph nodes are noted, largest measuring approximately 16x9 mm in size. No obvious necrosis within the nodes.
Fiberoptic flexible bronchoscopy revealed a huge mass with necrotic slough at origin of right main bronchus.
First biopsy revealed necrotic tissue only. Repeat rigid bronchoscopic biopsy revealed squamous cell carcinoma with necrotic tissue. Surgery was planned keeping in mind the second biopsy report.
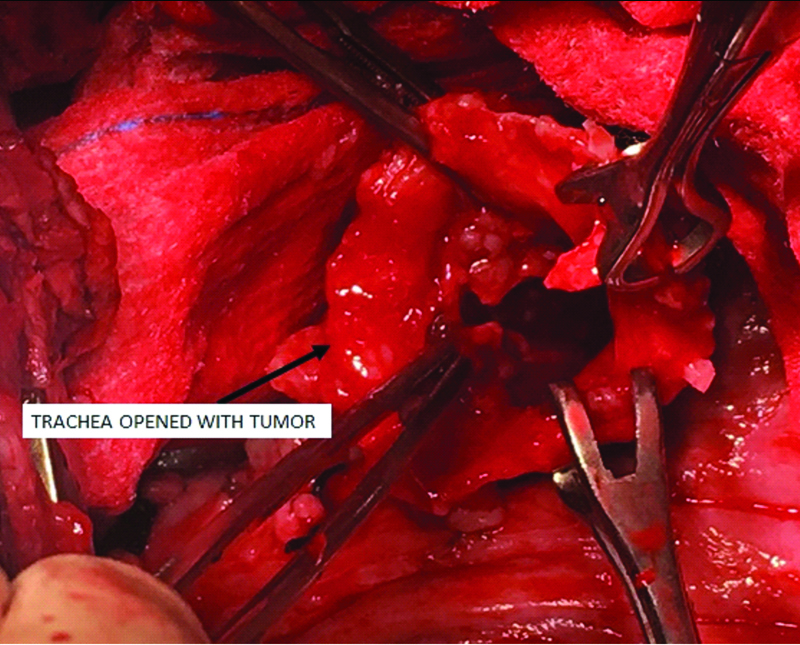
Surgery was done with right posterolateral thoracotomy in 4th intercostal space. Tumour had widened the tracheal diameter to approximately 5cm and the tumour had extended from carina to right main bronchus. Trachea was cut longitudinally with a sleeve at carinal level. Tumour along with a sleeve of trachea was excised with adequate margins. Tumour was polypoidal in nature. As the lung was almost completely destroyed by long standing obstructive pneumopathy, pneumonectomy was done. The longitudinal tracheal ostomy was closed in two layers with prolene 5 0 and buttressed with a pleural patch. This trachea was still admitting 7Fr endotracheal tube. Hilar lymph nodal dissection was completed. The distracted ribs were approximated and sutured with non-absorbable polyamide sutures. Chest was closed in standard fashion with insertion of intercostal chest tubes [Table/Fig-2]. Patient was electively ventilated till next morning. Postoperative convalescent period was uneventful and she was discharged on 10th day.
Trachea opened with intraluminal tumour seen.
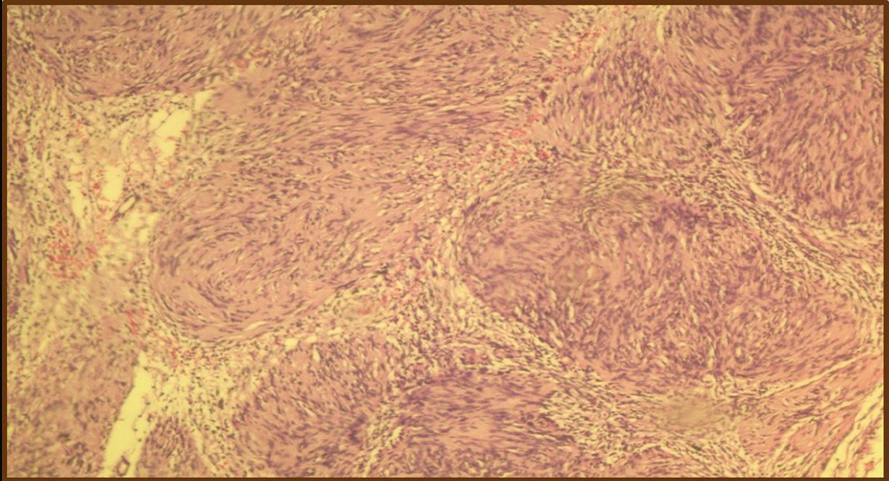
Postoperative histopathology report [Table/Fig-3] showed tumour composed of spindle cells with wavy nuclei, forming hypo and hypercellular areas with Verocay bodies; Surface showing mucosal ulceration, squamous metaplasia with focal dysplasia and dense lymphocytic infiltrate in mucosal and muscle layer. Eight lymph nodes were retrieved, all being inflammatory. Impression of Endobronchial Schwannoma with Alveolar Haemorrhage and changes of pneumonia, right lung was finalized. Patient has been on a regular three monthly follow up for last 11 months and is healthy.
Tumour composed of spindle cells with wavy nuclei, forming hypo and hypercellular areas with Verocay bodies. (H&E 10X).
Discussion
Primary tracheal schwannoma is an uncommon entity with a prevalence of less than 0.5% of all tracheal tumours. Two thirds of all primary tracheal tumours are evenly divided between squamous cell carcinoma and adenoid cystic carcinoma [1]. The remaining one third is a heterogeneous group composed of malignant, intermediate, and benign lesions.
The first reported case of neurogenic intrapulmonary tumour was in 1914 by Askanazy [2]. These are more commonly seen in women with no age predilection with male to female ratio being 1:3. Its clinical presentation is non-specific. Chronic cough, progressive respiratory distress [3] and asthma-like conditions are usual complaints. Suboptimal response to inhaled drugs or appearance of flow loop volume in PFT leads to the need of further investigation. Unfortunately, an average delay of 10-15 months in the diagnosis is reported [4]. The most important and preferred modality for diagnosis is rigid bronchoscopy, because it assesses the extent of the lesion and the length of healthy trachea available for anastomosis. It also provides more accurate measurements than the flexible bronchoscopy and gives the advantage of better control of the obstructed airway and control of any bleeding that may occur following biopsy. Bronchoscopy reveals a solitary, well encapsulated mass arising most often from the posterior wall of trachea; the lower third of the trachea is the most common site followed by the upper and then the middle thirds [5]. Computerized Tomography scan typically shows a well circumscribed enhancing mass within the tracheal lumen with no specific features. MRI of a tracheal schwannoma displays isointense or hyperintense T1-weighted images and hyperintense T2-weighted images with heterogeneous enhancement.
Tracheal schwannoma is primarily a pathological diagnosis. Schwannoma of the trachea arises from intra-luminal neurogenous tissue- Schwann cells of the nerve sheath. These tumours typically are single, well circumscribed; encapsulated tumours attached to a nerve but do not contain an axon. Grossly, they are well circumscribed and encapsulated; microscopically, areas of fibrillary, intensely polar, elongated appearing tissue type with high cellularity (Antoni A areas) as well as areas of loose microcystic myxoid fashion (Antoni B areas) are appreciated. Antoni A areas are punctuated by nuclei arranged in stacked alignments known as palisades which are called Verocay bodies. However, these Verocay bodies are not pathognomic of schwannoma. Capsular invasion, nuclear pleomorphism or mitoses are highly uncommon.
Although not 100% specific, S-100 protein is potentially a reliable marker for the diagnosis of schwannomas and is consistently seen in the Antoni A areas. Immunohistochemical stains for Glial Fibrillary Acidic Protein (GFAP), neurofilament protein and vimentin can also be positive [6]. The differential diagnosis of spindle cell lesions of the larynx and trachea includes spindle cell carcinoma, and wide range of benign and malignant mesenchymal lesions. Malignant lesions include a number of spindle cell sarcomas such as fibrosarcoma, synovial sarcoma, and leiomyosarcoma; however, these are extremely rare in this location and do not arise from the surface epithelium
Tracheal neurofibroma has uncommonly been associated with neurofibromatosis type I, however literature shows no association with schwannoma. Chondromas, papillomas, neurofibromas are benign tumours of trachea in the order of prevalence. The site of the lesion is variable and has been found as low down as the lingular bronchus. Schwannomas cause symptom when the tumour grows to obstruct the tracheobronchial lumen. These symptoms are late as they are slow growing in nature [7].
The rarity of such lesions has resulted in the paucity of consensus on standard surgical techniques but the primary treatment is surgical excision. Bronchoscopic excision, sleeve excision or tracheal resection, are all commonly accepted treatment modalities [7].
Surgical excision can either be done bronchoscopically [8]; limited resection of the trachea with lung preservation or pneumonectomy upto the carina when the tumour has reached upto carina and long term obstructive collapse has damaged the lung. Bronchoscopic resection when done adequately shows no recurrence in the 5 years follow up period. Tumour can also be approached from neck [9]. Late recurrences have been seen upto 12 years [10]. Laser resection with CO2 or Nd- YAG laser seems to be effective treatment for pedunculated tumours without the extratracheal extension. Tracheal resection with reconstruction has been propagated for sessile lesions with or without an extra-tracheal component.
Conclusion
Tracheal schwannoma are rare tumours with non-specific presentation. This results in delayed treatment. Bronchoscopy is the choice of investigation. Excision can either be done bronchoscopically or surgically.
Limited data results in absence of consensus in treatment guidelines
[1]. Grillo HC, Mathisen DJ, Primary tracheal tumours: treatment and resultsAnn Thorac Surg 1990 49:69-77.https://doi.org/10.1016/0003-4975(90)90358-d10.1016/0003-4975(90)90358-D [Google Scholar] [CrossRef]
[2]. Roviaro G, Montorsi M, Varoli F, Binda R, Cecchetto A, Primary pulmonary tumours of neurogenic originThorax 1983 38:942-45.https://doi.org/10.1136/thx.38.12.94210.1136/thx.38.12.9426665754 [Google Scholar] [CrossRef] [PubMed]
[3]. Demirjian BG, Gomez GA, Nguyen JL, Kharestan A, A rare case of obstructing tracheal schwannomaChest 2010 138(4):50Ahttps://doi.org/10.1378/chest.991410.1378/chest.9914 [Google Scholar] [CrossRef]
[4]. Karlan MS, Livingston PA, Baker DC Jr, Diagnosis of tracheal tumorsAnnals of Otology, Rhinology & Laryngology 1973 82(6):790-99.https://doi.org/10.1177/00034894730820060710.1177/0003489473082006074357418 [Google Scholar] [CrossRef] [PubMed]
[5]. Rusch VW, Schmidt RA, Tracheal schwannoma: management by endoscopic laser resectionThorax 1994 49:85-86.https://doi.org/10.1136/thx.49.1.8510.1136/thx.49.1.858153948 [Google Scholar] [CrossRef] [PubMed]
[6]. Schwannoma-Surgical Pathology Criteria-Stanford University School of Medicine [Google Scholar]
[7]. Moukarbel HAL, Tawil RV, El Khatib A, Ussama MH, Tracheal schwannoma: A misleading entityMiddle East Journal of Anesthesiology 2010 20(4):611-13. [Google Scholar]
[8]. Isaac BTJ, Christopher DJ, Thangakunam B, Gupta M, Tracheal schwannoma: Completely resected with therapeutic bronchoscopic techniquesLung India : Official Organ of Indian Chest Society 2015 32(3):271-73.https://doi:10.4103/0970-2113.15625210.4103/0970-2113.15625225983416 [Google Scholar] [CrossRef] [PubMed]
[9]. Han DP, Xiang J, Ye ZQ, He DN, Fei XC, Wang CF, Primary tracheal schwannoma treated by surgical resection: a case reportJournal of Thoracic Disease 2017 9(3):E249-E252.https://doi.org/10.21037/jtd.2017.02.8510.21037/jtd.2017.02.8528449512 [Google Scholar] [CrossRef] [PubMed]
[10]. Righini CA, Lequeux T, Laverierre MH, Reyt E, Primary tracheal schwannoma: One case report and a literature reviewEur Arch Otorhinolaryngol 2005 262:157-60.TetracyclineTeratologyhttps://doi.org/10.1007/s00405-004-0778-010.1007/s00405-004-0778-015060831 [Google Scholar] [CrossRef] [PubMed]