Treatment of Tongue Thrusting Habit Using Modified Blue Grass Appliance: A Case Report
K Mithun1, Mala Ram Manohar2, Naveen Shamnur3, G Shivaprakash4, Poorya Naik5
1 Assistant Professor, Department of Orthodontics, A.J. Institute of Dental Science, Mangaluru, Karnataka, India.
2 Professor and Head, Department of Orthodontics, College of Dental Sciences, Davangere, Karnataka, India.
3 Professor, Department of Orthodontics, Bapuji Dental College, Davangere, Karnataka, India.
4 Professor, Department of Orthodontics, College of Dental Sciences, Davangere, Karnataka, India.
5 Professor, Department of Orthodontics, College of Dental Sciences, Davangere, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Mithun, Assistant Professor, Room No. 5, Department of Orthodontics, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India.
E-mail: dr.mithunknaik@gmail.com
Tongue thrusting habit is a major aetiological factor in the development of anterior open bite. Persistence of an infantile swallow during childhood and adolescence leads to a tongue thrusting habit with clinical features of open bite and protrusion of anterior tooth segment. Sequelae of treatment for the habit are removal of the aetiology, retraining exercises and use of mechanical restraining appliances. Palatal crib or palatal spurs are commonly used as habit-breaking appliances. These appliances cause problems like difficulty in speech, mastication, and iatrogenically or self-inflicted injuries. This case report discusses a case with anterior open bite, dental proclination and spacing which was treated by a fixed tongue trainer in the form of modified blue grass appliance and extraction of the first premolar followed by fixed orthodontic therapy for treatment of dentoalveolar protrusion.
Habit breaking appliance, Open bite, Tongue trainer
Case Report
A 19-year-old female patient reported to the department with a chief complaint of forwardly placed upper front teeth since five years. Patient does not give any significant family history, medical history, dental history or any thumb sucking habit. There were no relevant findings on her digits. On visual examination, the patient was seen to have a habit of tongue thrusting. The patient was internally motivated with a positive attitude towards orthodontic treatment and cited aesthetics as the main reason for desiring orthodontic treatment.
On extra oral examination patient was diagnosed with a dolicocephalic, leptoprosopic face, incompetent lips and convex profile. Smile arc was not consonant with lower lip curvature. The patient displayed a complex type of smile with 100% upper incisors crown exposure, 3mm of gingival exposure and 30% lower crown exposure.
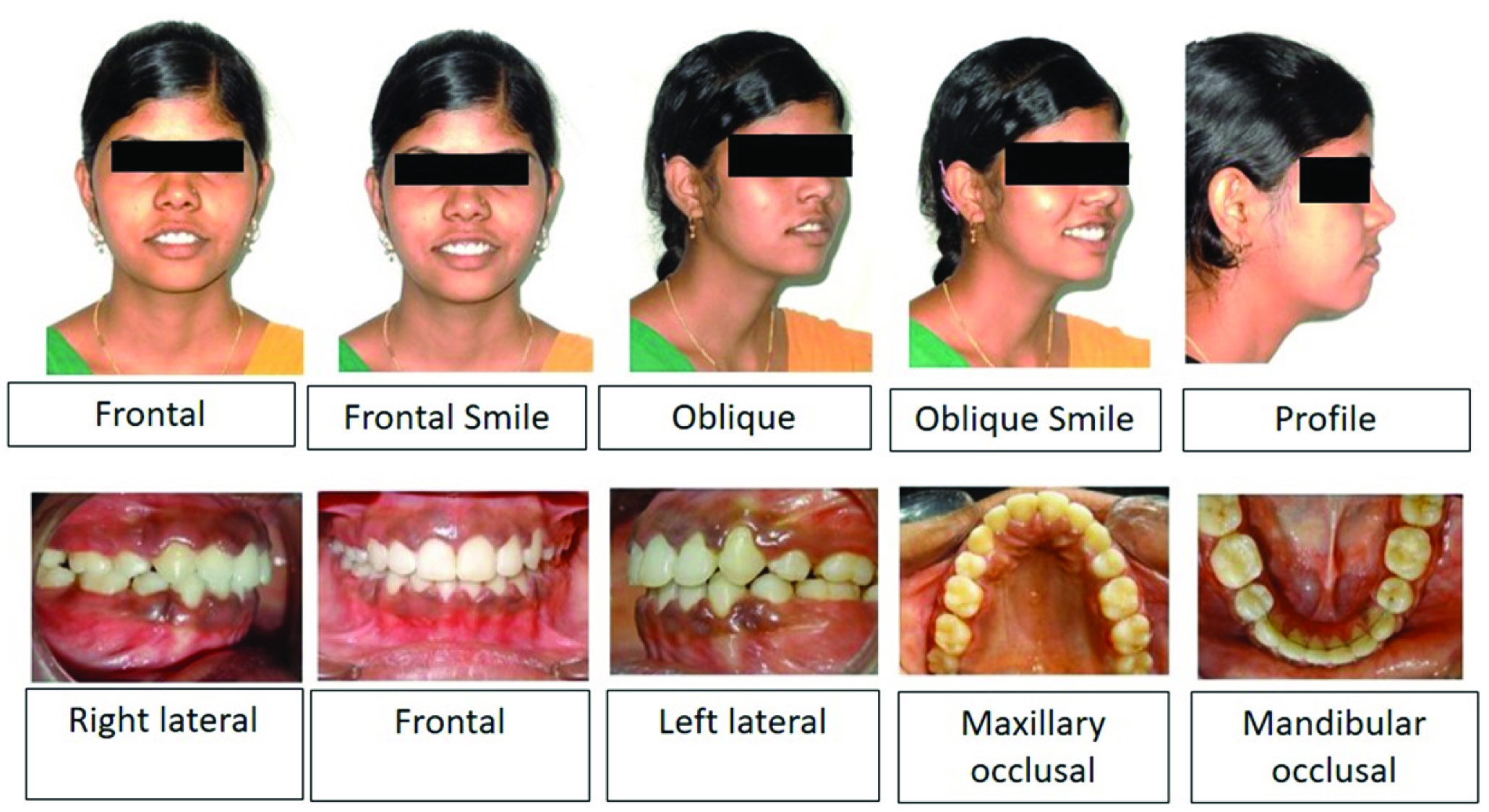
Intraoral examination revealed a U-shaped upper and lower arch with spacing in anteriors. The patient exhibited Class I molar and Class I canine relation bilaterally, an over jet of 2 mm and an overbite of 1.5 mm. Anterior open bite due to the tongue thrusting habit with flat curve of spee was observed in the mandible [Table/Fig-1].
Pre-treatment: Extra oral and Intra oral photographs.
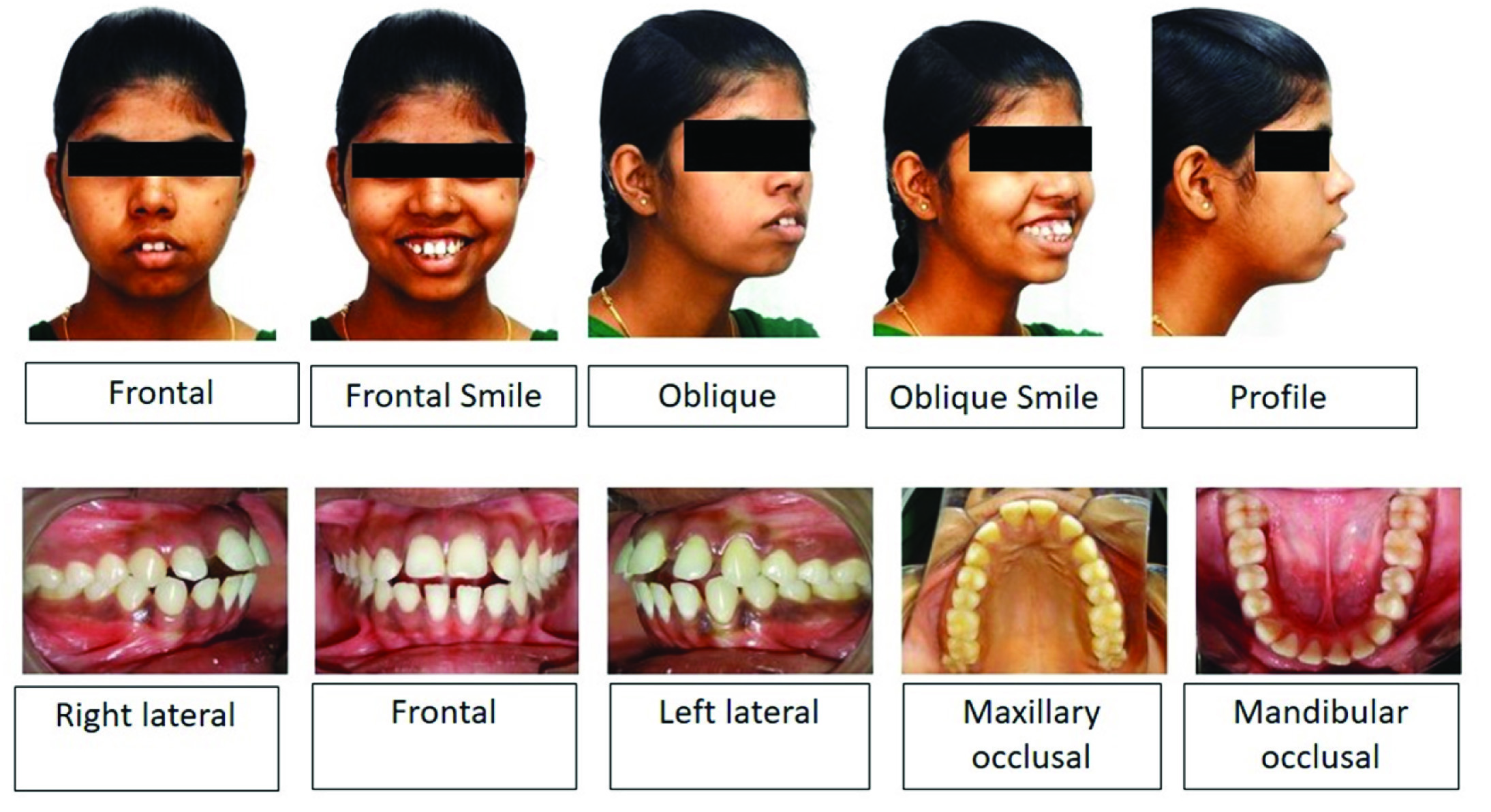
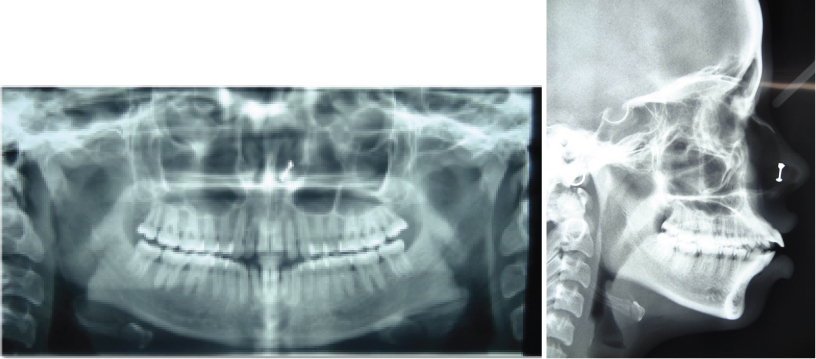
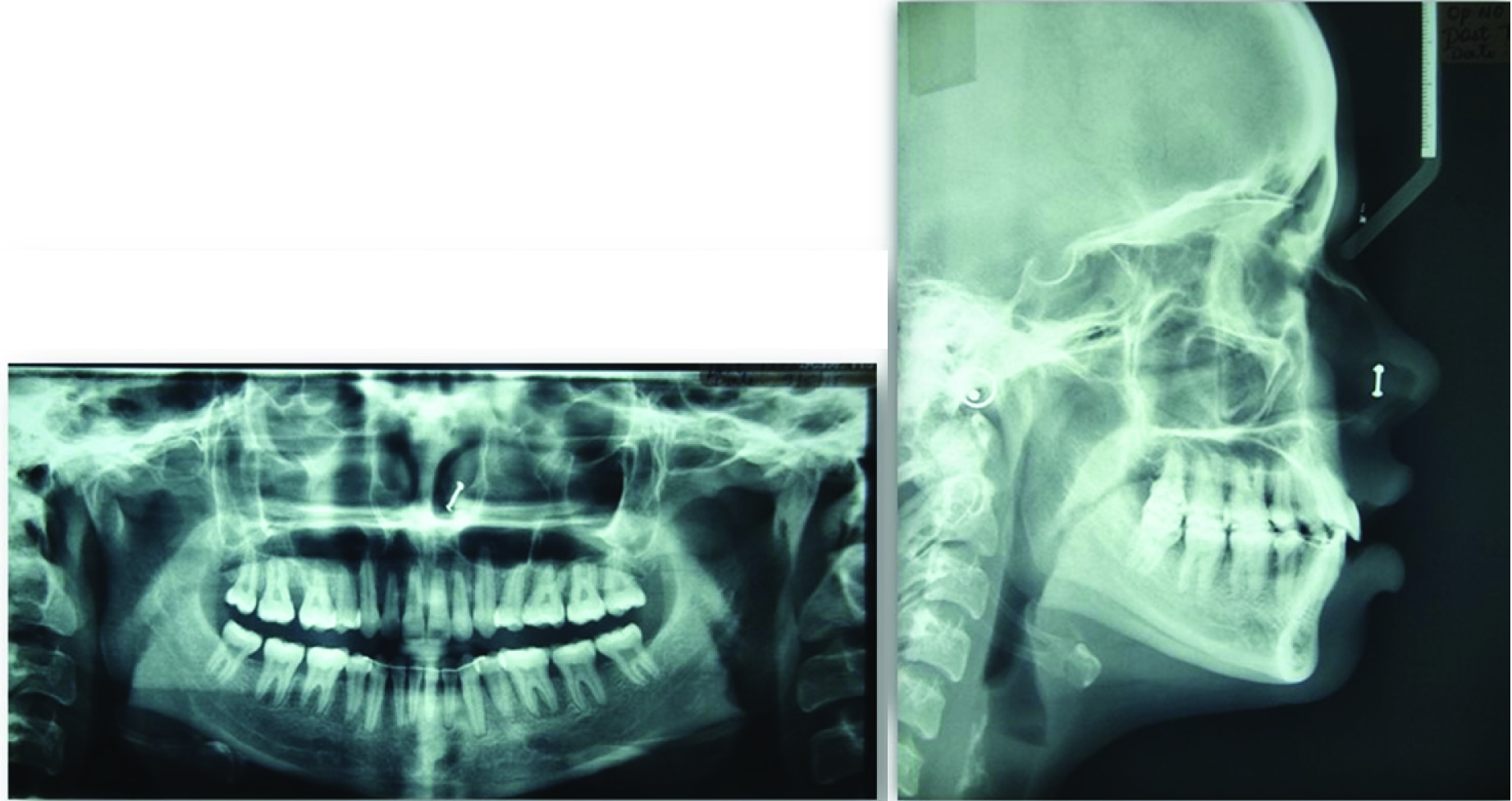
Orthopantomogram examination revealed asymmetrical condylar morphology bilaterally. All third molars root formation was two third complete suggesting dental age of 19-20 years. On Cephalometric examination, the patient had a skeletal class I jaw relationship with an average mandibular plane angle, proclined upper anteriors by 14 mm and proclined lower anteriors by 9 mm. The abnormal position of the tongue was also confirmed by tracing the pre-treatment lateral cephalogram [Table/Fig-2].
Pre-treatment Orthopantomogram (OPG) and Lateral cephalogram.
Thus the case was diagnosed as a skeletal class I jaw relationship with Angle’s class I molar and class I canine relationship bilaterally with an anterior open bite due to tongue thrusting habit.
Treatment Objectives
The main objective of the treatment was to eliminate the aetiology which in this case was the tongue thrusting habit. The other treatment objectives were to improve the profile, lip competency, smile aesthetics and achieve normal overjet, overbite and proclination of upper/lower anteriors.
Treatment Mechanics
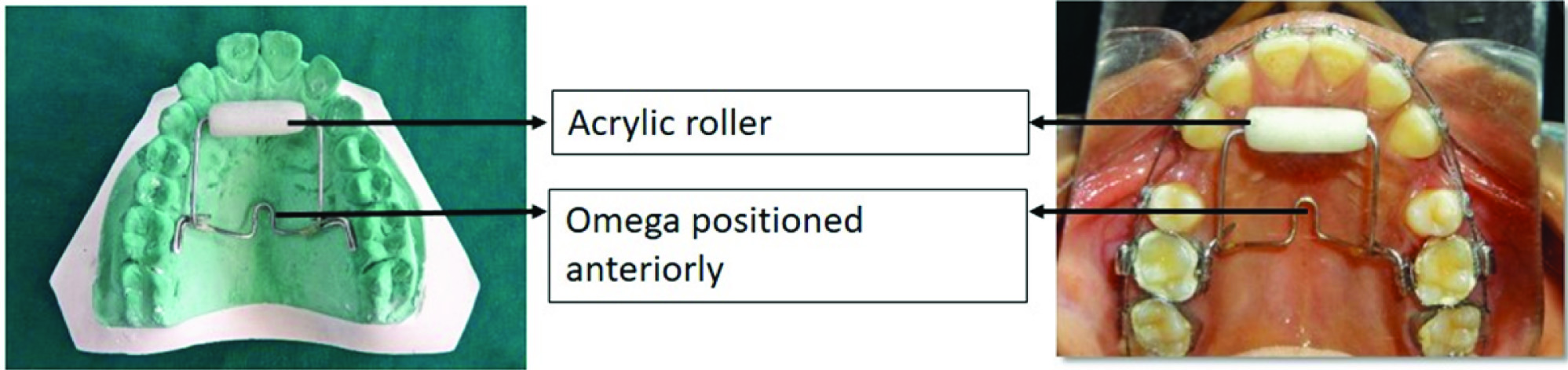
Tongue exercise: Haskell and Mink described a non-punitive fixed appliance to stop thumb-sucking which they called the Bluegrass (BG) Appliance [1]. The components of modified blue grass appliance were molar bands, lingual sheath, stainless steel wire and a hexagonal shaped acrylic roller [Table/Fig-3]. The maxillary first molars were banded with a lingual sheath. A modified transpalatal arch made up of 0.036” stainless-steel wire extending from the molar band to the rugae of the anterior palate which encompassed a hexagonal shaped acrylic roller was placed on the lingual sheath. The omega part of the transpalatal arch was positioned anteriorly to elicit pressure from the tongue which helped in intrusion of molars [2]. The entire assembly was placed 4-5 mm away from the palate to avoid any extrusive component acting on molars which could worsen the profile [3]. The patient was instructed to play by spinning the roller with tongue which establishes a new non-harmful habit of playing with the roller.
Modified blue grass appliance.
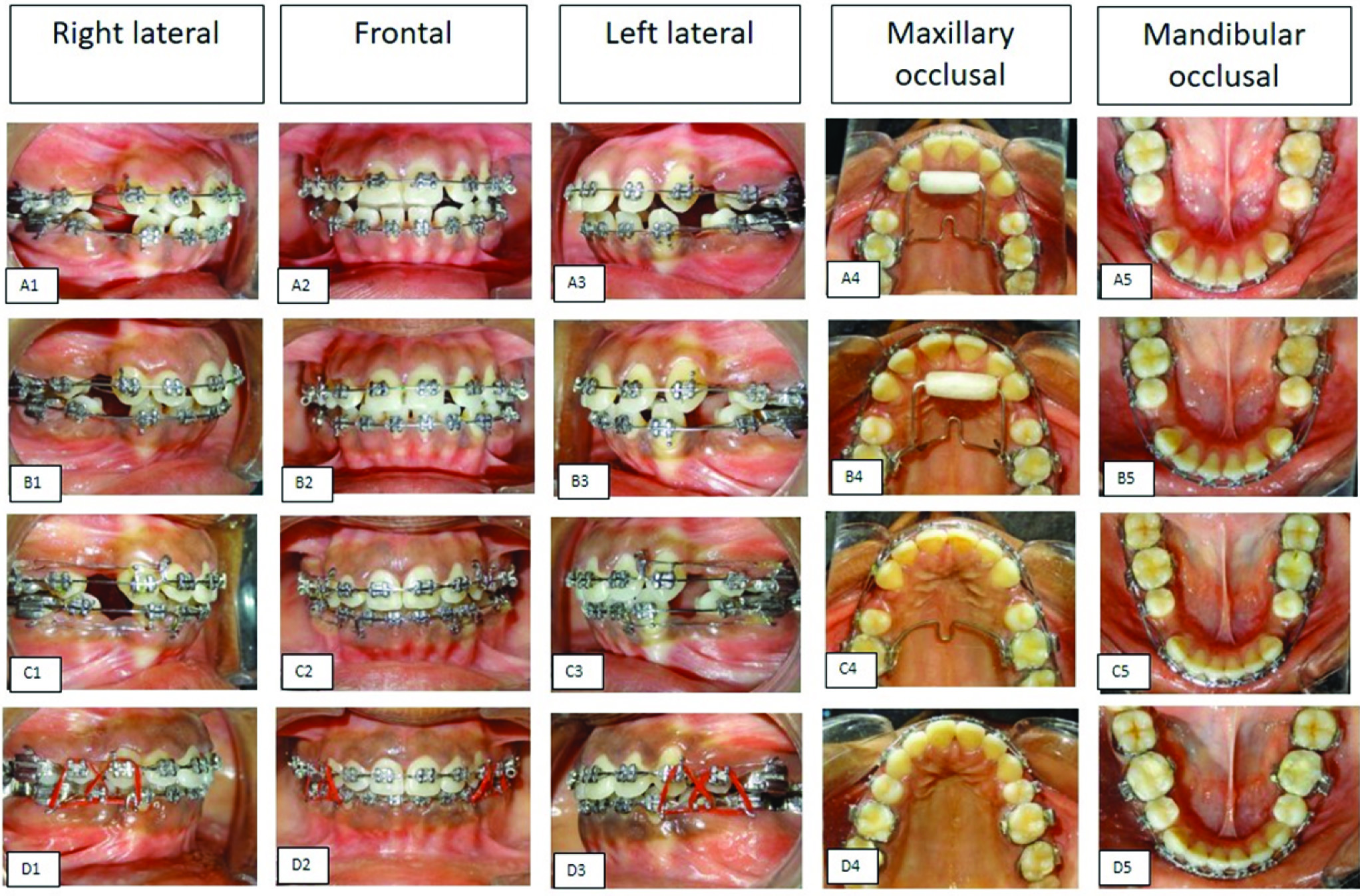
Fixed orthodontic mechanotherapy: Extraction of all first premolars 14,24,34,44 was performed. A 0.022’’ slot Preadjusted Edgewise Appliance (PEA) brackets with MBT prescription were used in upper and lower arch. Leveling and aligning with a sequence of round and rectangular nickel titanium wires were carried out for 5 months [Table/Fig-4] A,B(1,2,3,4,5) Retraction was carried out in 19x25 stainless steel using sliding mechanics with an active tie back [Table/Fig-4] C(1,2,3,4,5). Finishing and detailing were carried out based on the post retraction findings. Settling was achieved using triangular elastics [Table/Fig-4] D(1,2,3,4,5). Debonding was done after achieving the treatment objectives. A fixed lingual retainer made up of 0.010’’ multistrand wire was bonded on the lingual surface of mandibular anterior teeth. An impression was made, and a wrap-around hawley’s retainer was delivered in the maxillary arch. The total duration of the treatment was 18 months. Pre and Post treatment photographs and radiographs revealed correction of tongue thrusting, improvement in the profile, overjet and overbite. Improved smile aesthetics and correction of proclination of upper/lower anteriors was also seen [Table/Fig-5,6 and 7].
A (1,2,3,4,5) 0.016 Nickel Titanium, Modified Blue grass appliance, B (1,2,3,4,5) 17×25 Nickel Titanium, C (1,2,3,4,5) 19×25 Stainless steel retraction, D (1,2,3,4,5) Post retraction- settling elastics.
Post-treatment: Extraoral and Intraoral photographs.
Post-treatment Orthopantomogram (OPG) and Lateral cephalogram.
Post treatment lateral cephalogram findings.
| S. No. | Parameter | Mean | Pre-Treatment | Post-Treatment |
|---|
| Skeletal |
| 1 | SNA Angle (Degree) | 82 | 81 | 82 |
| 2 | SNB Angle (Degree) | 80 | 80 | 80 |
| 3 | ANB Angle (Degree) | 2 | 1 | 2 |
| 4 | N Prep. to Pt. A (mm) | 0±2 | –1.5 | 2 |
| 5 | N Prep. to Pog (mm) | 0 to –4 | –4.5 | –5 |
| 6 | GoGn to SN (Degree) | 32 | 30 | 26.5 |
| 7 | Angle of Inclination (Degree) | 85 | 91 | 89 |
| 8 | Lower Anterior of FAce Height (mm) | 66.1±4.3 | 70 | 69 |
| 9 | Effective Maxillary Length (mm) | 92.7±2.3 | 93 | 91 |
| 10 | Effective Mandibular Length (mm) | 120±3.4 | 122 | 115 |
| 11 | Y-Axis Angle (Degree) | 66 | 67 | 65 |
| 12 | Facial Axis Angle (Degree) | 0 | –3 | 2 |
| 13 | Sum of Post Angles (Degree) | 396±6 | 395 | 388 |
| Dental |
| 14 | U1 to NA Angle (Degree) | 22 | 43 | 25 |
| 15 | U1 to NA (mm) | 4 | 18 | 3 |
| 16 | U1 to SN Angle (Degree) | 102 | 127 | 112 |
| 17 | L1 to NB Angle (Degree) | 25 | 44 | 33 |
| 18 | L1 to NB (mm) | 4 | 13 | 6 |
| 19 | L1 to A Pog (mm) | 1 to 2 | 9 | 3 |
| 20 | L1 to Mand Plane Angle (Degree) | 90 | 112 | 93 |
| 21 | Inter Incisal Angle (Degree) | 130 | 93 | 127 |
| Soft Tissue |
| 22 | S Line to U Lip (mm) | –2 | 6.5 | 3 |
| 23 | S Line to Lip (mm) | 0 | 10.5 | 5 |
| 24 | Nasolabial Angle (Degrees) | 90 to 110 | 97 | 115 |
Discussion
Tongue thrust can be broadly classified into primary and secondary tongue thrusting. Primary tongue thrusting can be due to learned behaviour, prolonged thumb sucking and nasal congestion. Secondary tongue thrusting is due to extraction of deciduous tooth or anterior open bite [4]. Clinical management of tongue thrusting habit through conventional therapies includes sequential use of appliances to correct each of the problems individually. Thus, the modified appliance introduced in the presented case report corrected the tongue thrusting habit and anterior open bite. Crib rake type of appliances have a punitive approach which are intended as a punishment, as opposed to a positive reinforcement approach [5].
Sayın MO et al., studied the initial effects of the tongue crib by means of Magnetic Resonance Imaging. They stated that the tongue tip was positioned more posteriorly when the crib was in place and, to compensate for this adaptive changes occurred in the anterior and midportions of the dorsum of the tongue [6]. A lack of success with crib therapy reported by Subtelny and Sakuda was associated with crib wear of less than 6 months. We chose to use a fixed crib appliance that would remain in the mouth for more than 6 months [7]. It has been reported that using a compliance-free, fixed appliance for the correction of open bite and inhibition of habits produces more favourable results [8,9].
Thus a positive reinforcing approach as modified blue grass appliance with a roller was used in the presented case report. The roller is placed in the most superior aspect of the palate which does not cause obstruction with eating, emotional problems, and iatrogenically “self-inflicted” wounds and presents minimal disturbance to speech. The roller of the appliance is based on the principles of positive reinforcement which works through a counterconditioning response to the original conditioned stimulus for tongue thrusting [1].
The roller has been used in the present case to rectify the tongue thrusting habit and anterior open bite. The roller can be used as an elective treatment strategy for concurrent interception of sucking habit and repair of the dentofacial malformations according to Zameer M et al., [10]. In the present case it has been used to correct the tongue thrusting habit and anterior open bite. In order to prevent the recommencing of the habit after stoppage, the roller must be placed for an additional six months. This is in accordance with the protocol by Haryett RD et al., and was followed in this case [11].
The modified blue grass appliance has an edge over the palatal crib by virtue of being a fixed appliance that can be used in non-subservient patients. Another plus is that it circumvents the extrusion of the molar teeth. An alternative innocuous and gentle habit of playing with the roller was introduced to change the neuromuscular activity and harmonise the tongue position.
Conclusion
This case represents the use of a modified blue grass appliance with a roller as a positive reinforcing approach to correct the tongue thrusting habit. When the patient played with the roller it created a new habit, thus breaking the old one and holding true for the adage “the proper way to eliminate bad habits is to replace them with good ones.”
[1]. Haskell BS, Mink JR, An aid to stop thumb sucking: the “Bluegrass” appliancePediatr Dent 1991 13(2):83-85. [Google Scholar]
[2]. Chiba Y, Motoyoshi M, Namura S, Tongue pressure on loop of transpalatal arch during deglutitionAm J Orthod Dentofacial Orthop 2003 123(1):29-34.10.1067/mod.2003.5112532060 [Google Scholar] [CrossRef] [PubMed]
[3]. Nikkerdar A, Butterfly arch: a device for precise controlling of the upper molars in three planes of spaceJournal of Dentistry (Tsehran, Iran) 2013 10(3):221-26. [Google Scholar]
[4]. Subtelny JD, Oral habits: Studies in form, function, and therapyAngle Orthod 1973 43:347-83. [Google Scholar]
[5]. Massler M, Wood AW, Thumb-suckingJournal of Dentistry for Children 1949 16(1):01-09. [Google Scholar]
[6]. Sayin MO, Akin E, Karaçay S, Bulakbaşi N, Initial effects of the tongue crib on tongue movements during deglutition: a Cine-Magnetic resonance imaging studyAngle Orthod 2006 76(3):400-05. [Google Scholar]
[7]. Subtelny JD, Sakuda M, Openbite: Diagnosis and treatmentAm J Orthod 1964 50:337-58.10.1016/0002-9416(64)90175-7 [Google Scholar] [CrossRef]
[8]. Cozza P, Baccetti T, Franchi L, Mucedero M, Comparison of 2 early treatment protocols for open-bite malocclusionsAm J Orthod Dentofacial Orthop 2007 132(6):743-47.10.1016/j.ajodo.2005.11.04518068591 [Google Scholar] [CrossRef] [PubMed]
[9]. Giuntini V, Franchi L, Baccetti T, Mucedero M, Cozza P, Dentoskeletal changes associated with fixed and removable appliances with a crib in open-bite patients in the mixed dentitionAm J Orthod Dentofacial Orthop 2008 133(1):77-80.10.1016/j.ajodo.2007.07.01218174075 [Google Scholar] [CrossRef] [PubMed]
[10]. Zameer M, Basheer SN, Reddy A, Kovvuru SK, A single versatile appliance for habit interception and crossbite correctionCase Reports in Dentistry 2015 2015:60754510.1155/2015/60754526640722 [Google Scholar] [CrossRef] [PubMed]
[11]. Haryett RD, Hansen FC, Davidson PO, Chronic thumb-sucking: a second report on treatment and its psychological effectsAmerican Journal of Orthodontics 1970 57(2):164-78.10.1016/0002-9416(70)90263-0 [Google Scholar] [CrossRef]