Metaphyseal extra articular fracture of distal tibia is common and difficult to treat because of close proximity with ankle joint and usual association with soft tissue injury [1]. By preference these fractures are managed with internal fixation in a view of fact that conservative management predictably causes loss of reduction, ankle stiffness and malunion [2-4]. With emerging techniques involving percutaneous reduction method, interest for internal fixation for these fractures has been further renewed. Intramedullary nails design has been improved in recent years and their indication further extended to fractures nearer to the ankle joint [5]. Success with putting two interlocking screw in the distal fragment has also been reported [6]. These newer tibial nails warrant placement of screws in close proximity to tip of distal nail. These refinements on the reduction and stability have been confirmed in the laboratory as well as in the clinical follow ups [7]. Plating assures anatomic reduction and firm fixation but extensive soft tissue dissection is inevitably leading to increased rate of non union, infection and also inadequacy of soft tissue over the anteromedial tibia results in hardware prominence and wound dehiscence [7,8]. Also, for plating, improved Minimally Invasive Plating Osteosynthesis (MIPO) technique has been introduced which limits the local soft tissue damage [9], which has gained significant recognition in recent years.
Still, at present ideal surgical option for these fractures is controversial in spite of fair number of studies comparing IM nailing with plating [8-13]. Some clinical Controlled trials which directly compares these two methods failed to show uniform result [10,11]. As no concord has been reached, the optimal treatment still remains arguable. Thus, this study was undertaken to evaluate and compare the functional outcome and complication rate of these two modalities i.e., reamed intramedullary nailing and anatomical plating by minimally invasive plate osteosynthesis technique for treatment of distal tibia extra-articular metaphyseal fractures.
Materials and Methods
A prospective comparative study was conducted in Department of Orthopaedic GSVM Medical College and Hospital, Kanpur, Uttar Pradesh, India, in total of 45 patients (male-28, female-17) with age group between 18-60 years having recent (<3weeks) closed, extra-articular distal tibial metaphyseal fracture (OTA type 43A) during the year June 2013 to August 2015. Patients registered in the study after Ethical Committee and Departmental Review Board approval and informed consent of all patients. Pros and cons of each procedure was described to all registered patients and then were divided into two groups depending upon the consent they give for treatment options to be part of study. In group A patients were managed with percutaneous reduction and internal fixation with plating by minimally invasive plate osteosynthesis technique [Table/Fig-1] and in Group B with close reamed intramedullary nailing and were evaluated. All pathological fractures, bilateral tibial fractures, old fractures, previous fracture of same or opposite side tibia and skeletally immature patients were excluded from the study. The 18 patients in total had associated lower third fibula fractures and were stabilized with either plate fixation or rush nail depending upon reduction of fibula achieved intraoperatively (if fibula got reduced with tibial fixation then fixed with rush nail or else with plating). One senior orthopaedic trauma surgeons treated the patient using plating and IM nailing. All patients were reviewed by same surgeon.
Percutaneous reduction and fixation (MIPO) technique for plating.
All patients were followed up regularly with least two years for clinical and radiological evaluation. Anteriorposterior and lateral radiograph were reviewed to ascertain the immediate and final alignment and fracture healing. Malunion was described as angular deformity of more than 10° in any plane or as shortening by 1 cm or more in comparison to contralateral side. Angular deformity was calculated by the angle formed between two lines i.e., one line from center of tibial plateau down to proximal shaft centre and second from ankle joint center up the distal shaft centre in comparison to the contralateral tibia. Tibial length was measured from anterior intercondylar area to inferior articular surface and compared.
Statistical Analysis
The Olerud Molander score was used for functional outcome assessment [12]. Data was analysed using student’s independent unpaired t-test. The chosen level of significance was p-value < 0.05. (software- SPSS version 10.0)
Results
After assessing the eligibility, a total of 45 patients were included, analysed and divided into two groups. Group A (plating) include 20 patients (male-12, female-8) with mean age of 41.90±15.27 years and Group B (IM nailing) include 25 patients (male-16, female-9) with mean age of 41.04±14.07 years which clearly conveys that the injury is more common in middle age group [Table/Fig-2]. There was no statistical difference for age between these two groups. Road traffic accident was primary mode of injury in patients (67%).
Demographic data and result. Data was analysed using unpaired independent student’s t-test.
| Parameter | Group A mean±S.D. | Group B Mean±S.D. | T score | p-value | Inference |
|---|
| Age (years) | 41.90±15.27 | 41.04±14.07 | 0.066 | >0.05 | Non significant |
| Time of callus formation (weeks) | 13±6.34 | 12.00±2.14 | 0.15 | >0.05 | Non significant |
| Union time (weeks) | 26.60±7.14 | 25.64±4.07 | 0.11 | >0.05 | Non significant |
| Angulation (degree) | 1.45±2.66 | 3.54±3.66 | 0.76 | >0.05 | Non significant |
| Shortening (cm) | 0.21±0.32 | 0.28±0.34 | 0.009 | >0.05 | Non significant |
| Surgical time (minutes) | 94.50±10.11 | 79.00±5.59 | 2.0 | <0.05 | Significant |
| Surgical delay (days) | 11.8±4.8 | 9.8±4.6 | 1.44 | >0.05 | Non significant |
| OMA score | 81.5±12.9 | 82.4±11.5 | 0.60 | >0.05 | Non significant |
(OMA= Oleurd Molandar score)
Mean surgical delay in Group A was 11.8±4.8 days and in Group B was 9.8±4.6 days (t-value 1.44, p-value 0.802). Surgical time in Group A was 94.50±10.11 minutes compared to 79.00±5.59 minutes in Group B and was statistically significant (t-value- 2.0, p-value<0.05) [Table/Fig-2].
In Group A, the mean time required for union was 26.60±7.14 week (range, 20-44 week), whereas in Group B, the time required was 25.64±4.07 week (range, 18–40 week). A p-value and t-value for the same were 0.594 and 0.11 respectively and were insignificant [Table/Fig-2]. Three patients in Group A and one patient in Group B failed to show callus formation by 20 weeks time so secondary procedure in form of bone grafting was done to achieve osteosynthesis at earliest in a view of reducing morbidity. Graft was taken from iliac crest and theses patients achieve union 44 weeks.
Partial weight bearing was allowed when there was appearance of callus formation on radiographs. Average mean time for appearance of callus in Group A was 13±6.34 weeks and in Group B was 12±2.14 weeks (t-value-0.15, p-value>0.05) [Table/Fig-2]. Functional outcome was assessed after two years of surgery with Olerud Molandar score. Mean Oleurd Molandar score for Group A was 81.5±12.9 (range, 40-95) and for Group B was 82.4±11.5 (range, 60-95). A p-value and t-value for the OMA score were 0.802 and 0.60 respectively [Table/Fig-2]. Both group had good score but slightly better in Group B. After analysis using unpaired student’s t-test, no significant difference was found in union rate, angular deformity, shortening and Oleurd Molandar score between the two groups.
Mean angulation in Group A was 1.45±2.66 degree and in Group B was 3.54±3.66 degree (t-value 0.76, p-value 0.107). Average shortening was 0.21±0.32 cm in Group A and in Group B was 0.28±0.34 cm (t-value 0.009, p-value 0.446). Shortening of 1 cm or more was found in 5% cases (1 case) in Group A and 8% cases (2 cases) in Group B. Malunion was found in 1 patient in Group A and 4 patients in Group B [Table/Fig-3].
Comparision of functional outcome by Oleurd Molandar score at final follow-up.
| Olerud Molander score | Group A | Group B |
|---|
| No. of Patients (%age) | No. of Patients (%age) |
|---|
| 91-100 (excellent) | 4 (20%) | 6(24%) |
| 61-90 (good) | 15 (75%) | 17(68%) |
| 31-60 (fair) | 1(5%) | 2(8%) |
| Mean score | 81.5±12.9 (range 40-95) | 82.4±11.5 (range 60-95) |
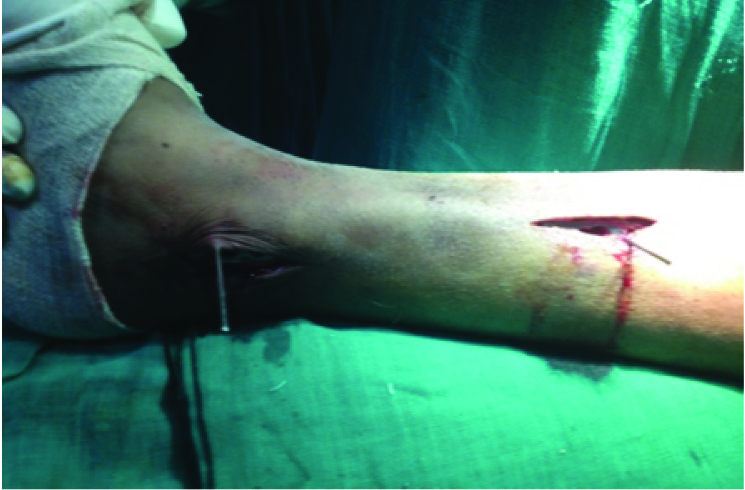
Skin necrosis with superficial infection occur over medial malleoli exposing the hardware in two patient [Table/Fig-4] and hardware prominence with mild pain around malleoli was found in six patients (30%) in Group A (plating). Deep seated infection occurred in one patient in Group A which was debrided thoroughly followed by prolonged antibiotic therapy and secondary suturing. Superficial infection appeared in two patients in group A which subsided by antibiotics and continued dressing. None of the patients in Group B showed sign of infection till follow up. In Group B, two patients had mild diffuse pain around medial side of leg centered over screw head and seven patients had mild anterior knee pain and discomfort while kneeling (28%).
Skin necrosis exposing hardware with superficial infection in plating group (Group A).

Discussion
Currently, both the techniques (IM Nailing and Plating) are used with relative success and there are pros and cons of each for distal tibial metaphyseal fracture. Vallier HA et al., showed distal tibia fractures can be managed effectively with either plates or nails [9]. Similarly Janssen KW et al., and Kwok CS et al., found no difference in union time in plating and nailing [10,11]. In the present study, to avoid surgical delay bias, we preferred treating these fractures with delay of one or two weeks. This surgical delay also improves the soft tissue condition around ankle. We noticed union was slightly early in nailing group as compared to plating. However, this was not significant (p-value>0.05).
Maintaining alignment in frontal and sagittal planes after IM nailing in distal tibial metaphyseal zone is a demanding task [13]. Increased malalignment after nailing in the metaphyseal fractures may result because of either incorrect entry point or due to difference between nail diameter and medullary canal size [14,15]. In a prospective randomized trial Im GI et al., concluded that ORIF with plating restore alignment better than IM nailing [16]. The average angulation in their trial was 0.9° in plating group compared to 2.8° after IM nailing. In another series authors found malunion in 40.7% cases managed with nailing [17]. The possible reason for this high rate could be no fixation done for fibula. Egol KA et al., in their study shows interconnections between adjunctive fibular stabilization and ability to maintain fracture reduction and they recommend fibular plating accompanying IM nailing for these fractures [18]. Furthermore, Kumar A et al., also reported that intact fibula or fibular fixation provides initial rotational stability [19]. In the present study, we found fixing fibula help us to restore alignment of tibia better without any significant delay in union time. Though, postoperative angulation was larger in group which was managed with IM nailing, however there was no statistically significant difference in incidence of malunion in both group. This finding may mean that the majority of angulations after IM nailing were well within acceptable limits even though the degree of angulation was greater than that of plating.
A recent meta-analysis by Mao Z et al., revealed insignificant difference in deep seated infection in IM nailing and plating but showed a significant difference in delayed wound healing and superficial skin infection and favours IM nailing [20]. Anterior knee pain was main postoperative complication after IM nailing whereas soft tissue complications such as superficial infection diffuse pain around medial malleolus were associated with plating in the present study. Janseen KW et al., also showed significant higher anterior knee pain as compare to plating [10]. The lack of surgery around the knee is one advantage of plating, but has chances of wound dehiscence and infection.
Some recent meta-analyses and systematic reviews are inconclusive in recommending one implant over other for these fractures [11,20,21]. Xue XH et al., prefered IM nail compared to plate [21] while Kowk CS et al., and Mao Z et al., concluded that both are appropriate treatment for distal tibial metaphyseal fractures [11,20]. In the present study, postoperative functional outcome were similar between nailing and plating groups.
Limitation
The limitations of the present study were small sample size and lack of long term follow-up. More number of patients could have better statistical evaluation. Long term functional status of patients could have more evident with extended follow-up. Also the study had undeniable shortcomings because of lack of proper randomization.
Conclusion
The results showed that both IM nailing and plating were effective methods in managing distal tibial metphyseal extra articular fracture, with functional outcome almost similar. Though IM nailing is associated with significantly lesser surgical time then plating, but there is no difference between union rates, malalignment functional outcome between these two groups. Therefore, we propose that both plate fixation and IM nailing are alternatives for the treatment of distal tibial metaphyseal fractures.
(OMA= Oleurd Molandar score)