Minor Salivary Gland Sialolithiasis: A Clinical Diagnostic Challenge
Roberto Pippi1, Marcello Santoro2, Angelina Pernazza3, Daniela Bosco4
1 Associate Professor, Department of Oral and Maxillofacial Sciences Faculty of Medicine and Dentistry, Sapienza University of Rome, Roma, Italy.
2 PhD, Department of Oral and Maxillofacial Sciences Faculty of Medicine and Dentistry, Sapienza University of Rome, Roma, Italy.
3 Postgraduate Student, Department of Radiological Sciences, Oncology and Anatomical Pathology, Sapienza University of Rome, Italy.
4 Associate Professor, Department of Radiological Sciences, Oncology and Anatomical Pathology, Sapienza University of Rome, Italy.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Marcello Santoro, via caserta 6, DDS, PhD, Department of Oral and Maxillofacial Sciences, Rome, Italy.
E-mail: santoro_marcello@yahoo.it
Sialolithiasis is a non-neoplastic salivary gland disease that rarely affects the minor salivary glands. There are no guidelines in the literature which can suggest which is the best surgical approach to treat Minor Salivary Glands Sialolithiasis (MSGL). The present case was of a 48-year-old male patient complaining of painful swelling localized in the left back-commissural zone which was 0.5 mm in diameter, for which surgical enucleation approach was done and in that some small calcific masses ranging from 0.2 to 4 mm in diameter were found. They were surrounded by granulation tissue and associated with small pus oozing. Histopathological examination was carried out leading to a final diagnosis of MSGL.
Diagnosis, Surgical enucleation, Swelling
Case Report
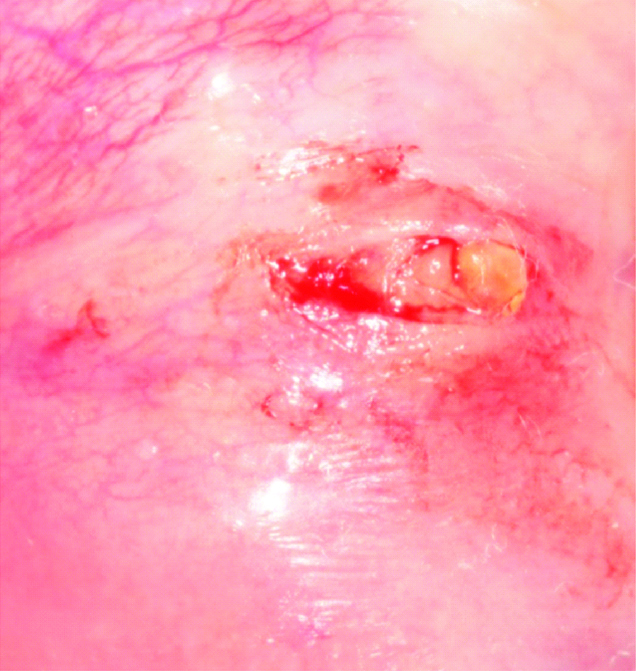
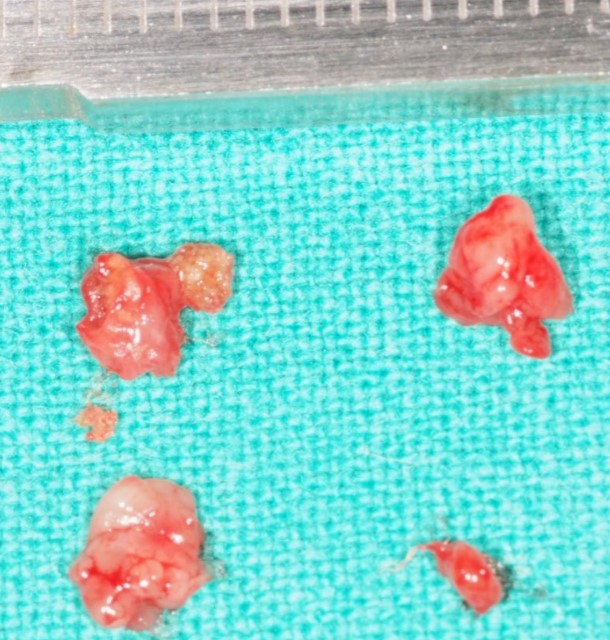
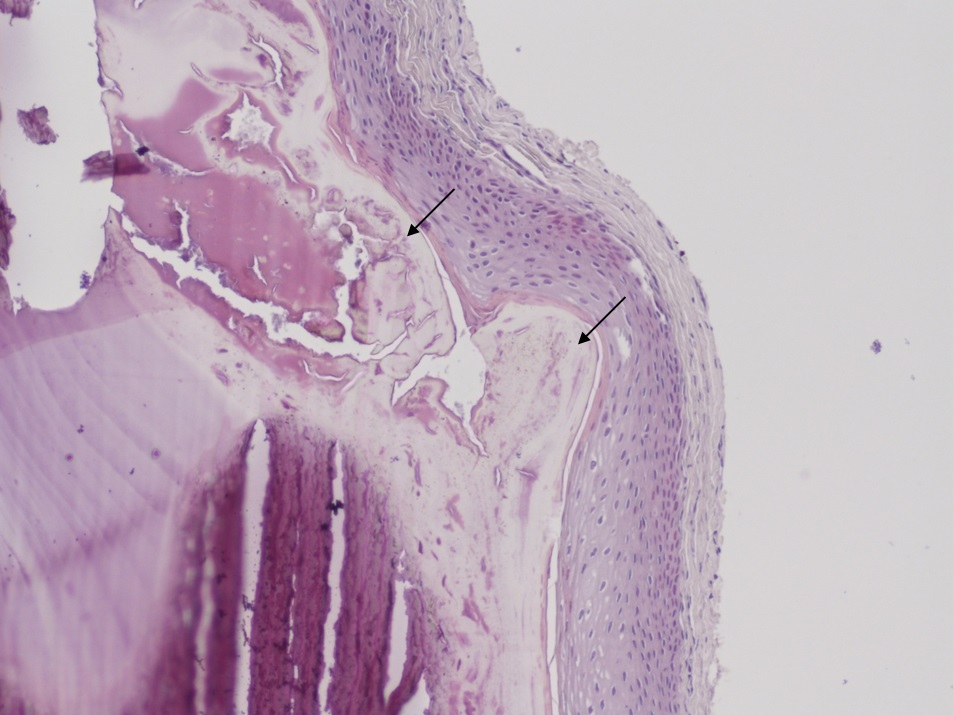
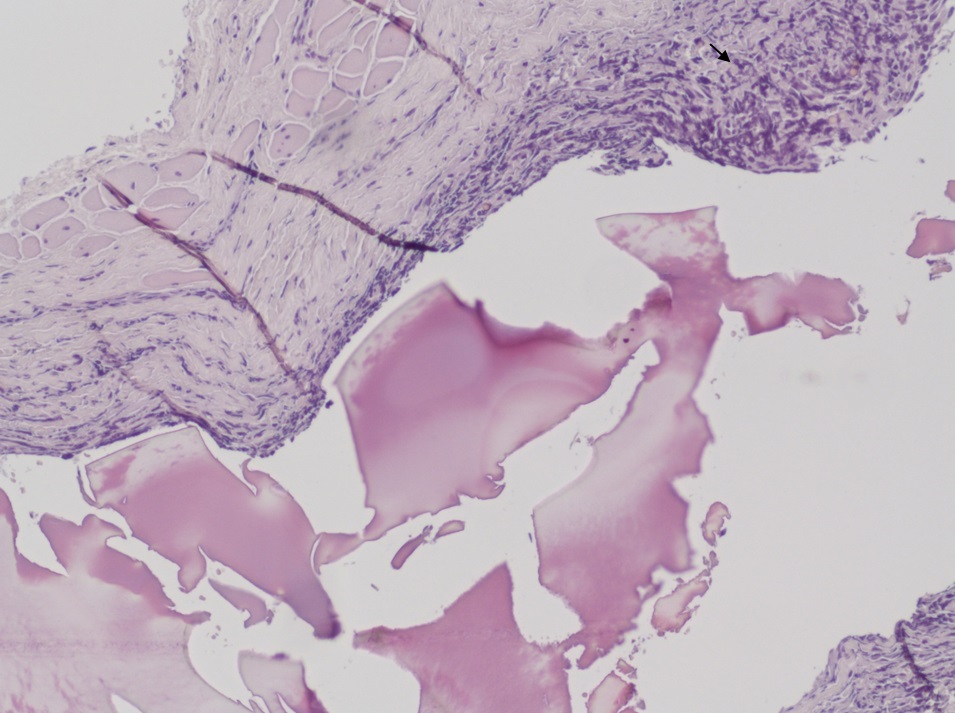
A 48-year-old male patient reported with a chief complaint of painful swelling localized in the left back-commissural zone since 5-6 months. It was consistent in size with no aggravating or relieving factors. No other symptoms or any local mucosal traumas before the swelling were noted by the patient. Intra oral examination revealed diffuse swelling about 0.5 mm in diameter, superficially covered by normal mucosa. On palpation it was fibrous, tender and mobile [Table/Fig-1]. An intra-oral radiograph was performed to detect the presence of any calcifications in the swelling but no calcific deposits were appreciated. The lesion was then enucleated under local anaesthesia, performing a linear incision on its surface, with an antero-posterior direction [Table/Fig-2]. In the swelling context, some small calcific masses ranging from 0.2 to 4 mm in diameter were found, surrounded by granulation tissue and associated with a small pus oozing [Table/Fig-3]. After the surgical site was revised, the wound margins were sutured. The histological examination, highlighted the presence of dilated duct, filled with reddish-appearing crystalline stone material characterized by concentrical lamination; the cyst epithelial lining was focally attenuated with diffuse squamous metaplasia and scattered cells with enlarged hyperchromatic nuclei. The cyst wall showed fibrosis and scattered fibroblast and was surrounded by the presence of a marked inflammatory cell infiltrate [Table/Fig-4,5]. The definitive diagnosis of MSGL was made. The post-operative course was uneventful.
A slight swelling is visible (arrow) in the left back-commissural zone, superficially covered by whitish mucosa.

A horizontal 1 cm linear incision has been performed to expose the underlying pathologic tissue.
Apparently calcific masses of 0.2 mm to 4 mm diameter surrounded by granulation tissue.
Calculus (arrows) is seen within a large duct, as concentric laminations of calcification, peripherally surrounded by compressed ductal squamous epithelium. (Haematoxylin&Eosin, 20X).
Epithelial duct erosion surrounded by a marked inflammatory cell infiltrate (arrow). (Haematoxylin&Eosin, 20X).
Discussion
Sialolithiasis is a non-neoplastic salivary gland disease that most commonly affects the submandibular glands, to a lesser extent the parotid glands and, in less than 2%, the sublingual and the accessory or minor salivary glands. Minor salivary glands have a rather ubiquitous distribution within the oral cavity although the gums and the anterior portion of the hard palate are rather rare locations [1-8]. It has been estimated that MSGL is more frequently associated with upper lip (49.2%) followed by upper cheeks (37.3%), lower lip (5.5%), vestibule (4.7%), palate and tongue (1.6%) [1,4]. Clinically, minor salivary gland calculi usually occur in the form of submucosal nodules of increased consistency, ranging from 0.2 to 30 mm, generally uncommon in subjects under 40 years without any sex preference, and radiotransparent in approximately half of the cases [1,5-8]. Surgical removal under local anaesthesia is the most effective treatment for MSGL. Histological examination is always necessary to exclude neoformative diseases [2-5]. Although chewing trauma may play an aetiologic role in the formation of salivary calculi [6], the most recent literature review, showing a predominant distribution of sialolithiasis in the upper lips [1,5], far less vulnerable to chewing traumas than the inferior one, points out the possible sharing of several factors, however not completely defined, in the aetiology of the MSGL, rather than the traumatic factor only [6], which, in fact, was not reported in the present case. The occlusion of salivary ducts by mucous membrane plugs, exfoliated epithelial cells, colonies of bacteria and foreign bodies seems to be the initial stage for the development of calculi. Local mechanical and biochemical factors such as trauma, inflammation, increased viscosity, and saliva acidity may promote calcium precipitation [5,6]. The secretion characteristics are also not the same for all minor salivary glands. The saliva produced by the lower gland of the lower lip and the palate has a lower viscosity and a lower mucous content than that produced at the upper lip or cheeks and this would explain the increased frequency of MSGL in these locations [2,4-8]. Within the salivary glands, physiologically, small concretions, called microliths, are also included which, although not directly related to the formation of calculi, could be capable of triggering scialoadenitic processes through a recurrent obstruction. Irritating factors are also capable of inducing spastic contractions of the ducts resulting in salivary stasis. Also the spread of mucus in the subcutaneous layer, following the breakdown of a mucocele, may constitute a predisposed condition for the formation of a new calcification nucleus [1,4-8]. All clinical data of the present case fall within those described in the international literature, although both the retro-commissural location and the time elapsed between the lesion occurrence and the moment in which the patient underwent the first examination were unusual [1]. Moreover, although MSGL is less frequently asymptomatic, in the present case the buccal swelling was painful and purulent, which could make it difficult to clinically differentiate from over-infected mucocele, lipoma, fibroma and benign or malignant lesion of minor salivary glands. The negativity of radiographic examinations was not useful for diagnosis as well, as in about 50% of cases, lithiasic concretions are radiotransparent [1-8]. There are no guidelines in the literature about the best surgical approach to the MSGL, although the treatment may be strongly affected, as in any other type of lesion, by the preliminary diagnosis and by the lesion size. In the present case, since neither fistulas nor deep or superficial tissue adherences were present, a single linear incision on the mucosal lesion surface allowed both the complete enucleation by blunt dissection of the pathological tissue and the lithiasic concretions it contained and the perfect facing of surgical wound margins for suturing, which led to early primary healing without any complications. Enucleation was not previously reported for MSGL, while an excisional biopsy was everywhere described [1,2,4-6].
Conclusion
Several diseases, other than MSGL, may affect sub-mucosal tissues such as inflammatory, traumatic, and tumoural, both benign and malignant. Since their diagnosis is often difficult or impossible by clinical examination only, it should be integrated by an accurate investigation and by the histological examination. The anatomic location of the lesion is sometimes important as well, in addressing the presumptive diagnosis, in relation to the different frequency of occurrence of some lesions, the slightly different histological tissue structure, and somewhat different functionality. The simple surgical enucleation of a long lasting clinically benign sub-mucosal lesion can be performed provided that no lesion adherences with peripheral tissues are clinically detectable.
[1]. Okada H, Yokokawa M, Komiya M, Akimoto Y, Kaneda T, Yamamoto H, A rare case of sialolithiasis of the lower lip simulating a mucocele and review of the literatureQuintessence Int 2011 42(7):589-94. [Google Scholar]
[2]. Pippi R, Severi A, Alò PL, Pilloni A, George B, Minor salivary glands calculi: an unusual case found in the hard palate mucosaInt J Oral Biol 2002 :79-81. [Google Scholar]
[3]. Pippi R, Technical notes about soft tissues biopsies of the oral cavityMinerva Stomatol 2006 55(10):551-66. [Google Scholar]
[4]. Boyd AS, Sialolith of a minor salivary glandJ Cutan Pathol 2013 40(8):695-98.10.1111/cup.1219123859700 [Google Scholar] [CrossRef] [PubMed]
[5]. Ben Lagha N, Alantar A, Samson J, Chapireau D, Maman L, Lithiasis of minor salivary glands: current dataOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 100(3):345-48.10.1016/j.tripleo.2004.12.02316122664 [Google Scholar] [CrossRef] [PubMed]
[6]. Lee LT, Wong YK, Pathogenesis and diverse histologic findings of sialolithiasis in minor salivary glandsJ Oral Maxillofac Surg 2010 68(2):465-70.10.1016/j.joms.2009.03.04120116725 [Google Scholar] [CrossRef] [PubMed]
[7]. Kimura M, Enomoto A, Shibata A, Nishiwaki S, Umemura M, A case of sialolithiasis in a minor salivary gland of the buccal mucosaJ Clin Diagn Res 2016 10(11):ZD06-ZD07.10.7860/JCDR/2016/21977.876628050512 [Google Scholar] [CrossRef] [PubMed]
[8]. Brazao-Silva MT, Prosdocimi FC, Lemos-Junior CA, de Sousa SO, Clinicopathological aspects of 25 cases of sialolithiasis of minor salivary glandsGen Dent 2015 63(3):e22-26. [Google Scholar]