Peripheral Ameloblastoma in an Adolescent Girl: Differential Diagnosis with Other Gingival Lesions
Saede Atarbashi-Moghadam1, Ali Lotfi2, Fazele Atarbashi-Moghadam3, Yasamin Ghaedsharafi4
1 Assistant professor, Department of Oral and Maxillofacial Pathology, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2 Retired Assistant professor, Department of Oral and Maxillofacial Pathology, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3 Assistant Professor, Department of Periodontics, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4 Student, Research Office, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Fazele Atarbashi-Moghadam, Assistant Professor, Department of Periodontics, 1st floor, School of Dentistry, Shahid Beheshti University of Medical Sciences, Daneshjoo Blvd, Evin, Chamran HWY, Tehran, Iran.
E-mail: dr.f.attarbashi@gmail.com
Differential diagnosis of intra-oral lesions is challenging and rare lesions are usually neglected. Peripheral (extra-osseous) ameloblastoma is the rarest form of ameloblastoma with high predominance in male. It occurs most commonly in the gingiva. The peak of incidence is above 50 years. The purpose of this report is to describe a case of peripheral ameloblastoma in an 18-year-old female, for more acquaintance with this rare lesion. Differential diagnosis of this lesion is also discussed in detail.
Benign, Extraosseous, Odontogenic tumour, Mandible
Case Report
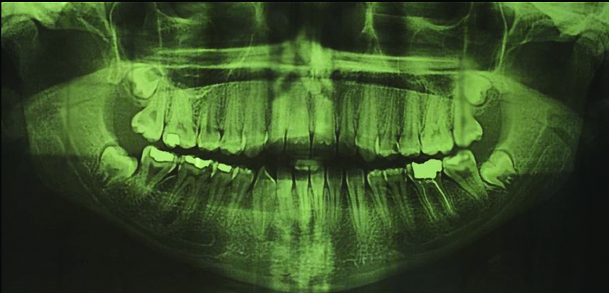
An 18-year-old girl was referred to a private oral pathology center (Tehran-Iran) with the chief complaint of swelling in gums since three years. The swelling grew gradually in size over the period of time. She had neither any other medical problem nor any history of previous trauma. Extra-oral examination was normal. Intra oral examination revealed a firm sub-mucosal mass (measuring 3×1.5 cm) in right mandibular lingual gingiva, extending from midline to second premolar area [Table/Fig-1]. The overlying mucosa was intact. There was no bleeding, no tenderness and no lymphadenopathy. The panoramic radiograph showed no evidence of alveolar ridge changes or intra-osseous lesion [Table/Fig-2]. Considering both clinical and radiographic features, provisional diagnosis of peripheral ossifying fibroma was given. The differential diagnosis includes benign soft tissue neoplasms and peripheral odontogenic tumours. Excisional biopsy was done under local anaesthesia.
Intra oral photomicrograph showing a red-pink submucosal mass in the lingual gingiva of right mandibular area from midline to second premolar.

No evidence of bone involvement in panoramic radiography.
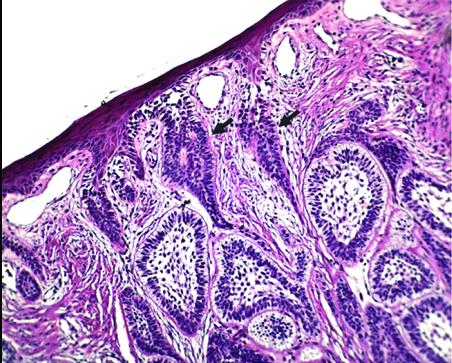
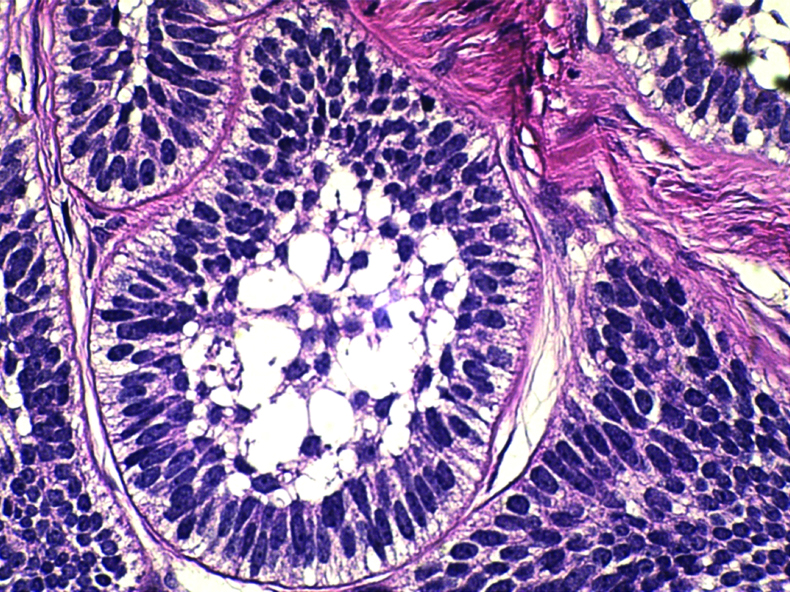
The gross specimen was a well-circumscribed, oval-shaped mass measuring 2.7×1.4 cm. It showed a solid, white and homogenous cut surface [Table/Fig-3]. Microscopic examination on low power demonstrated an odontogenic tumour containing islands of ameloblastic epithelium in follicular pattern that occupied the fibrous (collagenized) stroma. Connection of the neoplasm with basal layer of the surface epithelium was seen [Table/Fig-4]. High power examination revealed tumour islands depicted a single layer of tall columnar ameloblast-like cells surrounding a core of loosely arranged angular cells. The follicular nests fulfilled the Vickers and Gorlin criteria (peripheral cells with hyperchromatic nucleus, palisaded nuclei, reverse polarity and sub-nuclear vacuole formation) [Table/Fig-5]. Some acanthomatous changes in central portion of the nests were also evident. Pseudo-epitheliumatous hyperplasia was also seen. These microscopic features were consistent with the diagnosis of Peripheral Ameloblastoma (PA). Clinical follow-up was performed every three months in the first year after surgery with no evidence of recurrence [Table/Fig-6]. Patient has been placed on annual follow-up.
Gross specimen showing a well-circumscribed, solid, homogenous and creamy-white cut surface.

Microscopic section shows nests and islands of ameloblastic epithelium filling the lamina propria. Connection of the islands with the basal layer of the surface epithelium is also seen (black arrows) 100X; H&E stain.
Follicular nests of the tumour show palisaded peripheral cells with hyperchromatic nucleous, reverse polarity and sub-nuclear vacuole formation (Vickers and Gorlin criteria) surrounded a core of loosely arranged angular cells 400X; H&E stain.
One month after excision of the lesion.

Discussion
Central Ameloblastoma (CA) accounts for about 1% of all oral and maxillofacial pathologies and PA represents approximately 2% to 10% of all ameloblastomas, the rarest form [1,2]. Stanley and Krogh described the first true PA in 1959 [3]. The average age is 52 years and most of the cases are diagnosed in the fifth to seventh decades. It occurs in a considerably higher age group than those of CA. It shows a 1.9:1 male to female predilection [4]. The present case was an 18-year-old female. Development of PA in this age range is extremely rare. According to Philipsen HP series, only 1.48% of cases were under 20 years of age [4]. The commonest location is lingual aspect of mandibular gingiva in the premolar area followed by anterior region, similar to the present case. However, rare cases of buccal mucosa involvement were reported [5-7]. Oteri G et al., reported a desmoplastic form of PA present in maxilla in a 17-year-old boy [1]. Surya V et al., reported a PA in a retromolar region [8]. The aetiology of peripheral odontogenic tumours is indefinite and their sources are remnant of dental lamina that reside in the gingiva (rests of Serres), thus they develop in the gingiva and lingual to the primary teeth [9]. PA usually appears as a painless, sessile, firm nodular mass with smooth surface, but, pebbly and papillary appearance has also been described. It is usually pink in colour, but also seen in red to dark red [3,4].
Clinical Differential Diagnosis
The clinical differential diagnosis most often is reactive soft tissue lesions, followed by benign soft tissue neoplasms and peripheral odontogenic tumours [4,10].
Reactive Soft Tissue Lesions
They are induced as a response to irritations or trauma and can be formed on the gingiva as a sessile or pedunculated nodule. They are usually singular and asymptomatic. Surface ulceration may be due to trauma. They are predominant in female [11,12].
Irritation Fibroma (IF) usually has a pink colour and most commonly found in fourth to sixth decades of life [11,12]. The present case was of a patient younger than average age of IF.
Pyogenic Granuloma (PG) has tendency to occur on the facial aspect of interdental papilla of anterior maxilla. Its surface is typically ulcerated. Its colour ranges from red to pink (depending on lesion’s age). It usually entails soft consistency [11,12]. In the present case, we observed a pink, non-ulcerated lesion along with firm consistency.
Peripheral Giant Cell Granuloma (PGCG) present exclusively on gingiva. It appears with blue-purple colour. It most commonly occurs in first five decades of life [12]. The colour of present lesion did not match with PGCG.
Peripheral Ossifying Fibroma (POF) occurred only on gingiva. It ranges from red to pink in colour. Teenagers and young adults are most affected. There is a slight predilection for maxillary arch in incisor-cuspid region and interdental area [11,12]. Resorption of interdental bone and teeth separation may be seen [11]. The age of the patient and the colour and location of this lesion matched with POF.
Benign Soft Tissue Tumours
Fibromatosis is a firm, painless mass, most frequently occurs in children or young adults. The commonest site of the lesion is the paramandibular soft tissue. It often exhibit rapid growth. The lesion can grow to considerable size and is frequently poorly circumscribed showing infiltration into the adjacent tissue [12]. The appearance of this lesion and growth rate was not consistent with Fibromatosis.
Myofibroma is typically a painless mass develops most frequently in first four decades of life. The most common location is the mandible. Some myofibromas exhibit rapid enlargement [12]. The present lesion matched with characteristics of myofibroma.
Peripheral Odontogenic Tumour
Peripheral odontogenic fibroma is the most common peripheral odontogenic tumours followed by PA [9]. It typically occurs on the gingiva of the mandible [12]. Because of their rarity, it was considered, the latest differential diagnosis in the present case.
Histopathologic Differential Diagnosis
Peripheral variant of odontogenic fibroma, ameloblastic fibroma, developing odontoma (PDO) and ameloblastic fibro-odontoma (PAFO) may be confused with PA, microscopically [9,12]. The presence of dentinoid or cementum-like materials and the lack of peripheral columnar cells with reverse polarity in peripheral odontogenic fibroma should help to differentiate it from PA [12]. The connective tissue of three other peripheral odontogenic tumours shows dental papilla-like structures instead of fibrous stroma of PA. In PDO and PAFO, dental materials is evident [9].
Bone involvement is not seen in PA, but superficial alveolar erosion was also reported [1, 4]. Bone involvement must be ruled out for diagnosis of PA from CA with invasion into soft tissue [13]. PA possibly originates from rests of dental lamina beneath the oral mucosa or from the basal epithelial cells of the gingival epithelium [4,5]. Similarly connection of the ameloblastic islands with the basal layer of the surface epithelium was seen in present case. Surgical excision is the treatment of choice [2]. Unlike the CA, it demonstrates an innocuous clinical behaviour. Recurrence is rare [10]. But long term follow-up was recommended [2]. Some examples of malignant transformation in PA have been described [4,10].
Conclusion
PA is one of rare intra oral lesions and its occurrence in young adult female is extremely rare. Also, this lesion has benign behaviour, but some of them were reported to undergo malignant transformation, then familiarity with clinical and histopathology of this lesion was important and the patients need long term follow-up.
[1]. Oteri G, Lentini M, Pisano M, Cicciu M, Peripheral desmoplastic ameloblastoma in adolescent age: clinico-pathological and immunohistochemical analysis of a caseOpen Dent J 2014 8:159-63.10.2174/187421060140801015925317210 [Google Scholar] [CrossRef] [PubMed]
[2]. Bertossi D, Favero V, Albanese M, De-Santis D, Martano M, Padovano-di-Leva A, Peripheral ameloblastoma of the upper gingiva: Report of a case and literature reviewJ Clin Exper Dent 2014 6(2):e180-84.10.4317/jced.5112424790720 [Google Scholar] [CrossRef] [PubMed]
[3]. LeCorn DW, Bhattacharyya I, Vertucci FJ, Peripheral ameloblastoma: a case report and review of the literatureJ Endod 2006 32(2):152-54.10.1016/j.joen.2005.10.02816427467 [Google Scholar] [CrossRef] [PubMed]
[4]. Philipsen HP, Reichart PA, Nikai H, Takata T, Kudo Y, Peripheral ameloblastoma: biological profile based on 160 cases from the literatureOral Oncol 2001 37(1):17-27.10.1016/S1368-8375(00)00064-6 [Google Scholar] [CrossRef]
[5]. Goda H, Nakashiro K, Ogawa I, Takata T, Hamakawa H, Peripheral ameloblastoma with histologically low-grade malignant features of the buccal mucosa: a case report with immunohistochemical study and genetic analysisInt J Clin Exper Pathol 2015 8(2):2085-89. [Google Scholar]
[6]. Yuwanati MB, Singh A, Gadbail AR, Mhaske S, Hybrid peripheral ameloblastoma of cheek mucosaBMJ Case Rep 2013 doi:10.1136/bcr-2013-00951010.1136/bcr-2013-00951023853015 [Google Scholar] [CrossRef] [PubMed]
[7]. Woo SB, Smith-Williams JE, Sciubba JJ, Lipper S, Peripheral ameloblastoma of the buccal mucosa: case report and review of the English literatureOral Surg Oral Med oral Pathol 1987 63(1):78-84.10.1016/0030-4220(87)90344-6 [Google Scholar] [CrossRef]
[8]. Surya V, Verma P, Amale K, Siwach P, A case of peripheral ameloblastoma of retromolar trigone: Histopathological and immunohistochemical profileContemp Clin Dent 2015 6(4):564-66.10.4103/0976-237X.16985426681867 [Google Scholar] [CrossRef] [PubMed]
[9]. Atarbashi Moghadam S, Mokhtari S, Peripheral developing odontoma or peripheral ameloblastic fibroodontoma: a rare challenging caseCase Rep Dent 2016 2016:937901710.1155/2016/937901726981293 [Google Scholar] [CrossRef] [PubMed]
[10]. Beena VT, Choudhary K, Heera R, Rajeev R, Sivakumar R, Vidhyadharan K, Peripheral ameloblastoma: a case report and review of literatureCase Rep Dent 2012 2012:57150910.1155/2012/57150922570798 [Google Scholar] [CrossRef] [PubMed]
[11]. Meiller TF, Garber K, Scheper M, A review of common oral pathology lesions, with a focus on periodontology and implantologyJ Evid Based Dent Pract 2012 12(3 Suppl):254-62.10.1016/S1532-3382(12)70049-0 [Google Scholar] [CrossRef]
[12]. Neville BW, Damm DD, Allen CM, Chi AC, Oral and maxillofacial pathology 2016 4th EditionPhiladelphiaSaunders [Google Scholar]
[13]. Lascane NA, Sedassari BT, Alves Fde A, Gallottini MH, de Sousa SC, Peripheral ameloblastoma with dystrophic calcification: an unusual feature in non-calcifying odontogenic tumoursBraz Dent J 2014 25(3):253-56.10.1590/0103-644020130002425252263 [Google Scholar] [CrossRef] [PubMed]