Tuberculosis is a very common disease in developing countries. With the re-emergence of TB as an important infection worldwide, more and more cases of extra-pulmonary TB are being reported with unusual features. The clavicle is an uncommon site of skeletal TB. About 15% of TB patients have extra-pulmonary lesions of which 1-3% are bone and joint lesions [1]. TB of the sterno-clavicular region constitutes 1-2% of extra-pulmonary peripheral TB [2]. TB of the clavicle accounts for <1% of all osteoarticular TB [3]. Destruction of clavicle without pulmonary involvement pose of a diagnostic dilemma to clinch a diagnosis of tubercular osteomyelitis [2].
Osteomyelitis of the clavicle can occur either due to haematogenous spread or as a secondary infection from a contiguous infective focus. The infection reaches the clavicle via arteries as a result of bacillemia or uncommonly via the veins [4]. In children, clavicular osteomyelitis is due to haematogenous spread [5]. In adults, it is commonly due to secondary infection in association with some predisposing factors [6]. Tubercular osteomyelitis of clavicle has been reported after subclavian catheterisation and after head and neck surgery [7]. Tubercular osteomyelitis of clavicle occurs mainly in adults and is rare in children [8]. The incidence of pyogenic and fungal clavicular osteomyelitis is also uncommon [8].
Primary tubercular osteomyelitis of the clavicle is rare and only few case reports are available in literatures [9]. We are presenting the role of cross-sectional imaging in patients of tubercular osteomyelitis of the clavicle in eight patients with different clinical settings all of which were pathologically proven.
Materials and Methods
We conducted a hospital based prospective study, where eight patients of tubercular osteomyelitis of the clavicle were studied from June 2015 to December 2016 in the Department of Radiodiagnosis after due approval from the Institutional Ethics Review Board. The study was carried out in a Tertiary Care Centre in North East India. Informed consent was obtained from all patients or guardians, as applicable.
Inclusion criteria: All patients presenting with swelling over the clavicle or sternoclavicular joint, and subsequently diagnosed as TB were included in the study irrespective of age and sex.
Exclusion criteria: Patients associated with pulmonary, spinal or other appendicular joint TB were excluded.
Initially all patients were evaluated with plain radiographs followed by a cross-sectional imaging, either CT or MRI scan. CT was done in 6 patients and MRI in two patients.
CT scans of clavicle and sternoclavicular joints were studied using Siemens Somatom Spirit Dual Slice CT Scanner (Siemens Medical Systems, Erlangen, Germany) with 2 mm slice thickness and 1 mm reconstruction intervals. Contrast study was done after intra-venously injecting 1 mL/kg body weight of non ionic iodinated contrast media in all the six patients.
MRI scan was done in Siemens Magnetom Avanto B15 1.5T MRI machine (Siemens Medical Systems, Erlangen, Germany). An appropriate body or surface coil was used. A combination of transverse, sagittal, and coronal images were obtained using the following conventional sequences:
T1-weighted spin-echo sequence (TR range/TE range, 350-590/9-13 msec) with and without fat saturation.
T2-weighted Turbo spin-echo sequence (TR range/TE range: 3,200-6300/75-88 msec)
PDFS sequence (TR range/TE range: 4500-4900/25-28 msec, TI 160)
DWI sequence: TR range/TE range :3000-3100 /100-104 m sec, slice thickness 3 mm, b value 1000 s/mm2, interslice gap: 3.3 mm, matrix: 128×128, flip angle: 900.
Multiplanar post contrast T1 weighted spin echo sequence with fat suppression was acquired after injecting Gadopentetate dimeglumine as a single bolus injection at dose of 0.1 mmol/kg body weight.
The MRI parameters in T1WI, T2WI, PDFS and post contrast sequences were: Field of View (FOV) was 180-200, slice thickness 3-4 mm, interslice gap 3.6-4.4 mm and matrix size 512×512.
Evaluation: All patients were initially evaluated clinically for swelling in and around the clavicle or sternoclavicular joint and presence of sinus tract. The cross-sectional imaging either CT or MRI scan was performed on basis of clinician requirement or patient’s affordability. Initial plain radiograph were examined for presence of osteolytic lesion, periosteal reaction or pathological fracture. The CT scans were evaluated for location, osteolytic lesion either expansile or non-expansile, presence of cortical erosion, associated bony sclerosis, periosteal reaction, presence of sequestrum, status of surrounding inflammatory component, loco-regional extension of inflammatory component and contiguous joint involvement. The fine bony cortical erosion, periosteal reaction and sequestrum were better evaluated in CT scan rather than plain radiograph or MRI.
MRI scans were evaluated for presence of bone marrow oedema, bony destruction, status of surrounding inflammatory component, extension of inflammatory components and status of sinus tract. MRI provides early detection of bone marrow changes as well as soft tissue extension of inflammatory components or myositis rather than CT scan.
Histopathological diagnosis of clavicular lesions was established with fine needle aspiration, excisional biopsy or post debridement tissue biopsy in all eight patients.
Statistical Analysis
Data were presented in terms of mean and percentage. Calculations were done using Microsoft Excel and SPSS programs (Statistical Package for the Social Science version 16.0 SPSS Inc., Chicago, USA).
Results
In present study sample of pathologically proven 8 patients of tubercular osteomyelitis of the clavicle, the mean age was 37±1.8 years with a Male:Female ratio of 3:1. The demographic details, clinical presentation, imaging findings and management have been enlisted in [Table/Fig-1]. About 5 (62.5%) patients presented with pain and swellings [Table/Fig-2], 2 (25%) patients with chronic discharging sinuses and 1 (12.5%) patient with only swelling around the clavicle. The mean duration of symptoms was 6.4±2 months (SD). CT scan was done in 6 patients and MRI scan in 2 patients. The left clavicle was affected in 5 (62.5%) patients and right clavicle in 3 (37.5%) patients. The medial 1/3rd of the clavicle was more commonly affected in present study sample. Medial 1/3rd was affected in 4 patients (50%), lateral 1/3rd in 2 (25%) patients and medial 2/3rd in 1 (12.5%) patient. In one patient, both ends of the clavicle was affected (12.5%). Isolated middle 1/3rd affection was not seen in any patient in present study sample.
Summarises the clinico-radiological findings in eight patients of tubercular osteomyelitis of clavicle.
| Age (years)/sex | Side of involvement | Clinical presentation | Duration of symptoms (mths) | ESR (mm) | Mantoux test | Plain radiograph | Cross sectional imaging | Location of clavicle | Bone destruction | Sequestration | Periosteal reaction | sclerosis | Post contrast appearance | Adjacent joint involvement | Treatment | Associated findings |
|---|
| 18/M | Right | Pain and Swelling | 11 | 110 | +ve | Osteolytic lesion | CT | Both ends | Expa-nsile osteolytic | +ve | +ve | +ve | SP | + | ATT and debridement | |
| 24/M | Left | Discharging sinus | 9 | 105 | +ve | Pathological fracture | MRI | Lateral 1/3rd | Expansile osteolytic | -ve | -ve | -ve | IP | - | ATT and debridement | Necrotizing left axillary LAP |
| 56/M | Right | Discharging sinus | 14 | 89 | +ve | Osteolytic lesion | MRI | Medial 1/3rd | Expansile osteolytic | -ve | -ve | -ve | IP | + | ATT and debridement | |
| 12/F | Left | Pain and swelling | 12 | 76 | +ve | Osteolytic lesion | CT | Medial 2/3rd | Expansile osteolytic | +ve | +ve | +ve | PE | - | ATT and debridement | |
| 36/M | Right | Sw-elling | 7 | 59 | +ve | Unremarkable | CT | Medial 1/3rd | Fine erosions | -ve | -ve | -ve | PE | - | ATT only | |
| 60/F | Left | Pain and swelling | 8 | 67 | +ve | Unremarkable | CT | Medial 1/3rd | Fine erosions | -ve | +ve | +ve | SP | - | ATT and debridement | Collection in suprasternal notch |
| 56/M | Right | Pain and swelling | 5 | 56 | +ve | Unremarkable | CT | Medial 1/3rd | Fine erosions | -ve | -ve | -ve | PE | + | ATT only | Subluation of right SCJ |
| 34/M | Left | Pain and swelling | 8 | 79 | +ve | Osteolytic lesion | CT | Lateral 1/3rd | Expansile osteolytic | -ve | +ve | +ve | IP | - | ATT only | |
SP: Smooth peripheral enhancement; PE: Phlegmonous enhancement; IP: Thicker irregular peripheral enhancement; ATT: Anti-tubercular; SCJ: Sternoclavicular joint; LAP: Lymphadenopathy
An 18-year-old male patient presented with pain and swelling over right clavicle. a) The photograph of patient showed a boggy swelling over the medial aspect and mild swelling over lateral end of right clavicle; b) PA view Chest x-ray including right clavicle showed irregular expansile osteolytic lesions with cortical destruction in both medial and lateral ends of right clavicle with overlying soft tissue shadow along medial end (black arrows). Visualised bilateral lung fields were clear.
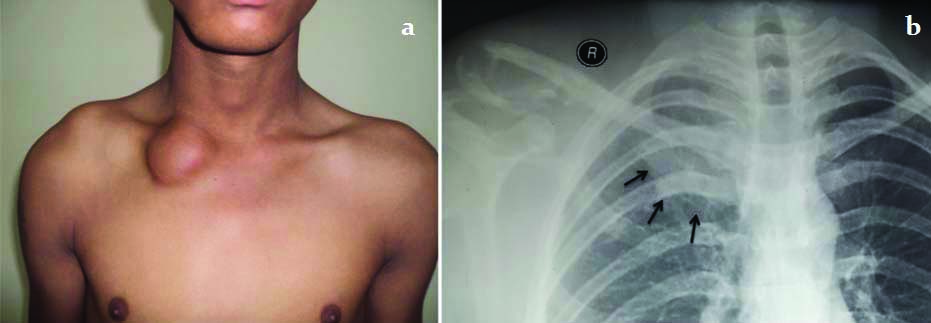
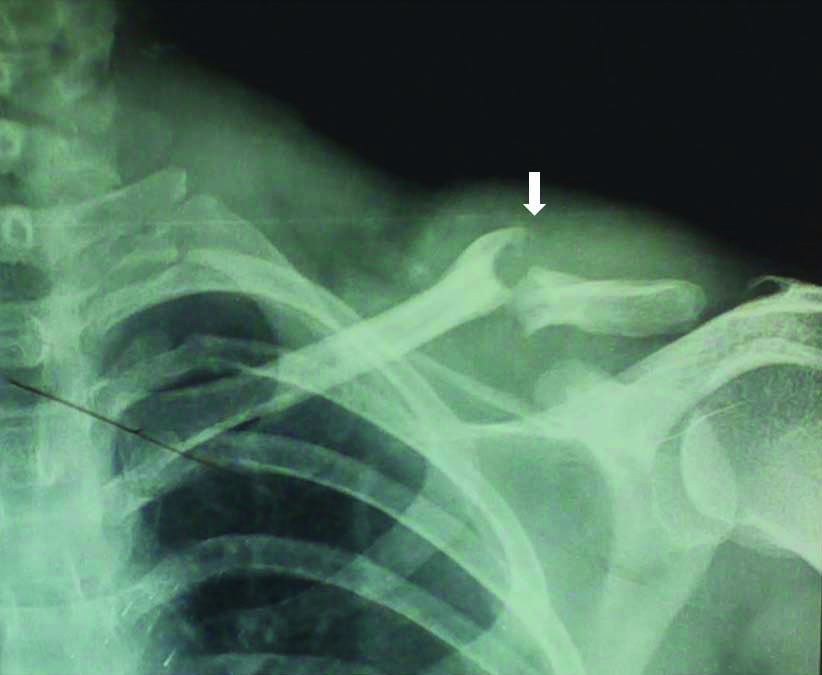
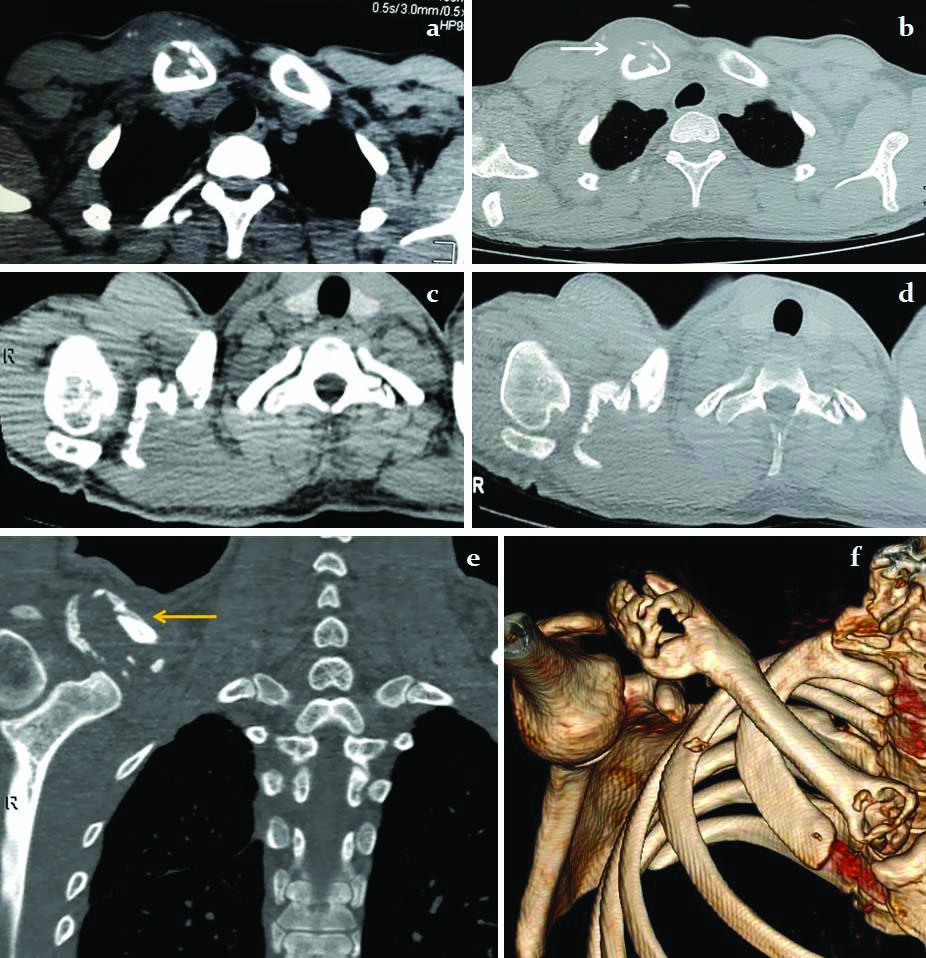
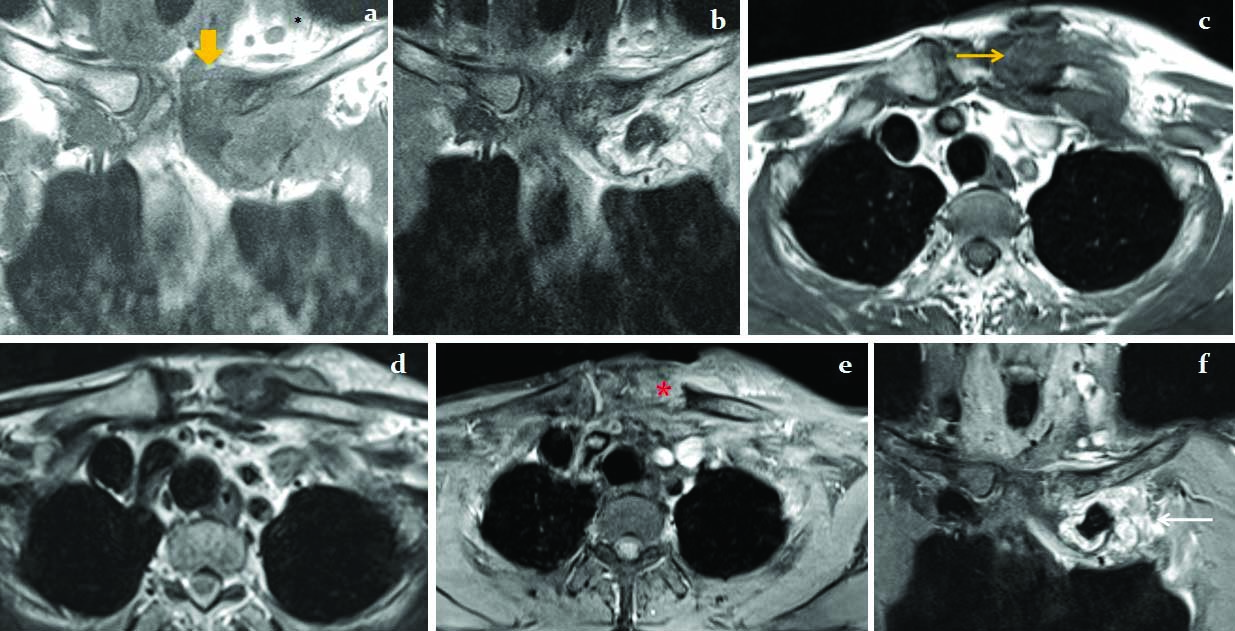
Plain radiographs detected osteolytic lesions in 4 patients (50%) [Table/Fig-2], pathological fracture in 1 patient (12.5%) [Table/Fig-3] and was unremarkable in 3 patients (37.5%). Cross-sectional imaging, especially CT scan showed bony details while MRI scan showed bone marrow affection and surrounding soft tissue signal alterations. Bony destructions in the form of expansile irregular osteolytic destructions [Table/Fig-4] were noted in 5 (62.5%) patients and fine bony erosions in 3 (37.5%) patients. Periosteal reaction was demonstrated in 4 (50%) patients, bony sclerosis in 4 (50%) patients and sequestrum formation in 2 (25%) patients [Table/Fig-4]. Post contrast study showed thick and irregular enhancement [Table/Fig-5] in 3 (37.5%) patients, phlegmonous enhancement [Table/Fig-6] in 3 (37.5%) patients and smooth peripheral enhancement of the collection around the affected clavicle in 2 (25%) patients. Contiguous affection of adjacent sterno-clavicular joint [Table/Fig-6] was demonstrated in 3 (37.5%) patients. Multiple thick and irregular peripherally enhancing lymph nodes with central necrosis [Table/Fig-5e] was noted in 1 patient.
A 24-year-old male patient presented with chronic discharging sinus over left clavicle. The AP view plain radiograph of left clavicle showed pathological fracture at the junction of middle and lateral one-third (white block arrow). Irregular osteolytic lesion with marginal sclerosis noted in clavicle around the fractured site. Diffuse soft tissue swelling was noted around fractured site of clavicle.
Axial plain CT images in soft tissue and bone window: a,b,c and d) showed irregular expansile osteolytic lesions with destruction of cortices in both medial (white arrow) and lateral ends of right clavicle. Associated ill defined hypodense collections were noted around the destructed clavicular ends with hyperdense intervening sequestrum formation. Coronal reconstructed MIP; e) and 3D-surface shaded display (SSD): f) images showed the clavicular lesions (yellow arrow in image 4e).
a) Axial T1; b) PDFS; c) coronal PDFS MR images showed abnormal T1W hypointense and PDFS hyperintense bony lesion in left clavicle with pathological fracture (white arrow) at the junction of middle and lateral 1/3rd. Another similar signal intensity lesion was noted in lateral end of left clavicle causing posterior scalloping (red arrow). T1W mild peripheral hyperintense and central hypointense collections were noted around the affected left clavicle. d) Coronal GRE image showed the wide gaping pathological fracture of left clavicle (red block arrow); e,f) Fat suppressed post gadolinium axial and coronal T1W images showed homogenously enhancing soft tissue lesion at site of pathological fracture with multiple thick walled peripherally enhancing abscesses over the clavicle and around the shoulder joint, more in supra-clavicular fossa extending into subcutaneous plane. Multiple necrotising thick peripherally enhancing lymphadenopathy were noted in left axilla (yellow arrow).
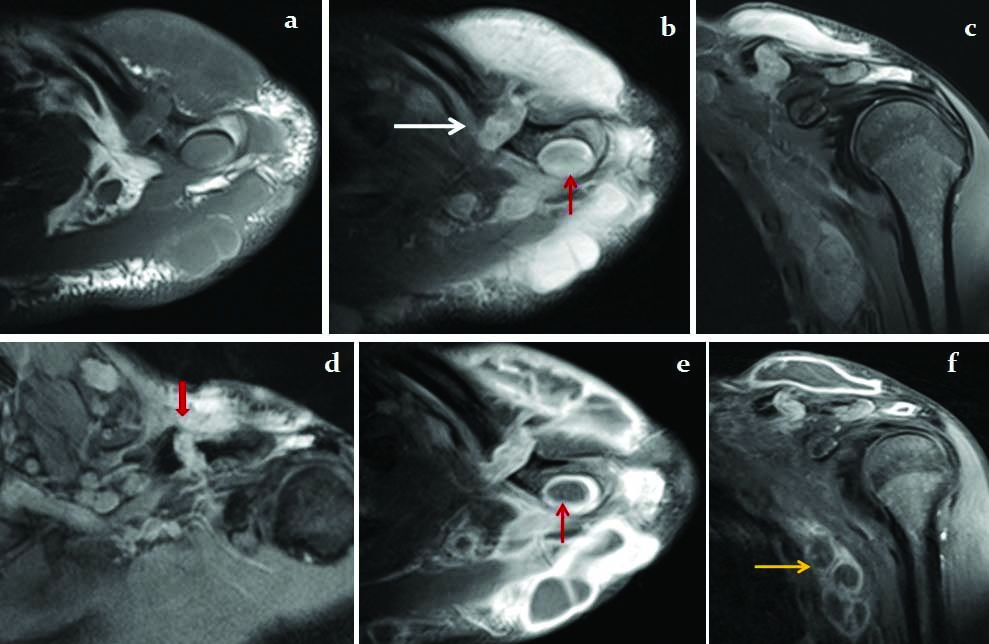
56 years male patient presented with chronic discharging sinus over medial aspect of left clavicle. a,b,c and d) Coronal and axial T1W and T2W images showed expansile destruction of medial 1/3rd of left clavicle (block yellow arrow) with affection of left sterno-clavicular joint (yellow arrow) showing ill defined T1 hypo and T2 mixed signal intensities within the affected portion of clavicle and sterno-clavicular joint. Fat suppressed post gadolinium axial and coronal T1W images e,f) showed irregular solid enhancement within the affected clavicle (*) which communicates with the thicker and irregular peripherally enhancing abscess just below the clavicle (white arrow).
Laboratory investigations showed raised Erythrocyte Sedimentation Rate (ESR) in all patients with a mean ESR of 79.1±18.5 mm at the end of first hour. All patients were reactive to Mantoux test.
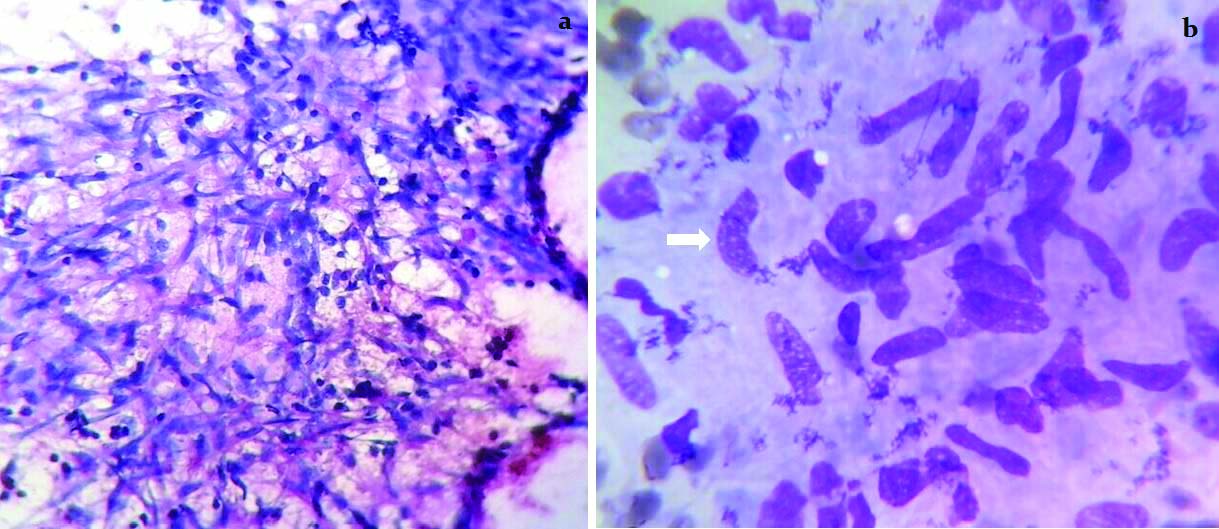
Histopathology confirmed all patients of clavicular tubercular osteomyelitis with varying clusters of epitheloid histiocytes admixed with lymphocytes suggesting tubercular granulomas. The histopathology images from one of our patients showing tubercular granuloma has been demonstrated in [Table/Fig-7].
The histopathology images of surgically debrided tissue from the clavicular lesion, a) HPE image showed clusters of epitheloid histiocytes admixed with lymphocytes suggesting tubercular granulomas (40X, Papanicolaou stain). b) Image showed epitheloid cells (white block arrow) with abundant pale cytoplasm and elongated slipper shaped nuclei with fine loose chromatin (100X, Giemsa stain).
All 8 patients were treated with Anti Tubercular Therapy (ATT) four drug regimen (rifampicin 600 mg, isoniazid 300 mg, ethambutol 1000 mg and pyrazinamide 1500 mg) for the first three months followed by three drugs, i.e., rifampicin, isoniazid and ethambutol for 9 months [10,11]. In addition, surgical debridement of the affected clavicle was done in 5 (62.5%) patients. The clinical, hematological and radiological parameters showed significant regression of the lesions on follow up after treatment with ATT.
Discussion
With an increase in the number of immunocompromised patients, especially HIV infected patients and the emergence of multi-drug resistant strains of TB, the incidence of osteo-articular TB is becoming more common. Because of increasing awareness of extra-pulmonary TB, the uncommon sites of the osteo-articular TB become a diagnostic dilemma [12].
Tuberculosis of the clavicle without involvement of neighbouring joints is rare. Tubercular osteomyelitis of clavicle is less common than pyogenic or fungal osteomyelitis [13]. The common differential diagnosis of non traumatic clavicular lesions are infectious lesions (pyogenic, granulomatous or syphilitic), neoplastic (metastasis, multiple myeloma, osteosarcoma, Ewing sarcoma, Giant Cell Tumour (GCT), congenital pseudo-arthrosis, condensing osteitis and sterno-clavicular hyperostosis [1,14].
After an exhaustive review of literature, we found about 16 cases reported with tubercular osteomyelitis of the clavicle in the past two decades. The clinico-radiological findings of these case reports have been compiled in [Table/Fig-2]. The present study was conducted chiefly to highlight the role of cross-sectional imaging in this condition, and to know the imaging features, since tubercular osteomyelitis of the clavicle is known to be a great mimicker.
Tubercular osteomyelitis of the clavicle can occur at any age. We found cases ranging from 12 years to 60 years. Aggarwal AN et al., [9] reported it in a 9 month neonate. However, contrary to the reports by Aggarwal AN et al., [9] and Shah J et al., [15], we found a male predominance. Affection of the medial end of the clavicle was more common compared to the lateral end. Suresh S et al., [16] stated that the lesions affecting the medial end of the clavicle are mostly benign and lesions affecting the lateral end are commonly malignant. Most of the lesions in present study were lytic and expansile. Sclerosis, when found was usually in association with the lytic lesions. The presence of sequestrum and periosteal reaction was quite uncommon. This could be a helping feature to differentiate from pyogenic osteomyelitis, where they are far more common. Sequestrum in tubercular clavicular osteomyelitis was previously reported by Dugg P et al., [2] and Agarwal A et al., [17].
The early stage of tubercular osteomyelitis of clavicle may present with swelling over the clavicle without discernable bone destruction, while in late stages of the disease process-cold abscess, chronic non-healing ulcer and multiple sinus tracts may form over the affected clavicle. The clavicular lesions in tubercular osteomyelitis are either destructive or proliferative (spina ventosa) forms. Plain radiographs in tubercular osteomyelitis of clavicle may show bony erosions, osteolytic cavities, honeycombing, sequestration, periostitis, cortical thickening and sclerosis, similar to pyogenic osteomyelitis [15]. Sometimes, it is difficult to differentiate these two entities [18]. However pyogenic chronic osteomyelitis of the clavicle commonly occurs in adolescent age group and usually starts in the medial end of clavicle with a characteristic short duration of disease onset with localised swelling and pain. The occurrence of sequestrum formation in more common in pyogenic osteomyelitis than tubercular osteomyelitis. Sometimes, even in tubercular osteomyelitis, sequestrum can form due to superadded pyogenic infection [3]. Clavicular osteomyelitis has been reported in dialysis patients [19] and HIV positive patients [20]. Post traumatic chronic tubercular osteomyelitis of the clavicle has also been reported [7]. We have encountered a case of post traumatic osteomyelitis of clavicle.
Agarwal AN et al., [9] reported 4 cases of tubercular osteomyelitis of clavicle, where they highlighted the plain radiograph and CT appearances only in three patients of tubercular osteomyelitis while in present study we have highlighted the CT as well as MRI appearances in 8 patients of tubercular osteomyelitis of clavicle.
CT scan in osteo-articular tubercular osteomyelitis shows bone and cartilage destruction, calcifications, inflammatory soft tissue lesions crossing the fascial planes which may either show irregular peripheral rim-like post contrast enhancement secondary to abscess formation or diffuse irregular post contrast enhancement in granulation tissue or phlegmonous forms [21]. CT scans can clearly demonstrate the cortical and cancellous bony destructions, spread of infection into adjacent joint space, associated periosteal reaction, sequestrum formation, reactive bony sclerosis, sinus tract formation and spread of infection via fascial planes into the nearby soft tissues and mediastinum [22,23].
MRI provides better sensitivity and specificity in detecting osteomyelitis of the clavicle than CT. MRI can nicely demonstrate bone signal alteration, marrow oedema and surrounding soft tissue oedema, inflammations and abscess formations. MRI scan can well demonstrate the extent of bone marrow oedema involvement as T1 weighted hypointense and T2 weighted or PDFS hyperintensities. Bony erosions are seen as T1weighted hypo and focal marginal PDFS hyperintensities in the cortices. T1 and T2 weighted hypointense bony sclerosis were also noted. The extension of inflammatory process via fascial planes is better demonstrated on MRI scan. Muscle inflammation and subcutaneous tissue cellulitis are seen as hyperintensities on T2 weighted and PDFS (fat suppressed proton density image) sequences. Chronic sinus tracts are also well visualised on both CT and MRI scan [14]. On MRI scan, sinus tracts are seen as a T1 hypointense and T2 hyperintense tract which shows irregular marginal tram-track like post contrast enhancement [13,14]. Sometimes, presence of air foci within the sinus tract or inflamed surrounding soft tissue gives T1 and T2 weighted hypointensities [14]. The soft tissue inflammatory collection in tuberculous lesion shows short T1 relaxation and longer T2 relaxation as compared to many infectious lesions [24]. Inflammatory collections in TB may show a peripheral hyperintense rim on non contrast T1 weighted images and on post gadolinium T1W images show thick, irregular peripheral enhancement.
Sometimes, chronic tuberculous osteomyelitis of the clavicle may initially present with complications. The possible complications include multiple sinus tract and fistula formations, pathological fracture of clavicle, erosion of nearby subclavian vessels with subsequent thrombosis, extension of tuberculous abscess into pleural cavity and mediastinum [14,21].
The common differential diagnosis of pain and swelling at medial end of clavicle in children includes Tietze syndrome [25], avascular necrosis of clavicular epiphysis (Friedrich disease), traumatic medial clavicular physeal separation, infections and tumours (including metastasis). Expansile osteolytic variant of tubercular osteomyelitis may mimic GCT. Malignant lesions occur predominantly in the older age group (>50 years), most commonly being metastases, for which the clavicle is an uncommon site due to its sparse red marrow content [26]. Rarely multiple myeloma deposits can occur in the clavicle. Osteitis condensans claviculi is seen as an area of increased sclerosis in the inferior part of the medial end of the clavicle without any periosteal reaction or bony erosions. The sterno-clavicular joint would also be unaffected [16] and hence can easily be differentiated from tubercular arthritis of clavicle.
Chronic osteomyelitis in SAPHO syndrome is one of the closely related differential diagnoses. SAPHO syndrome comprises of synovitis, acne, pustulosis, hyperostosis and osteomyelitis. It may present with chronic osteomyelitis of the clavicle which was first reported by Chamot AM et al., in 1987 [27] Chronic recurrent osteomyelitis of the clavicle in SAPHO syndrome in a great mimicker of Tubercular osteomyelitis of clavicle.
Here, hyperostosis and osteitis are the most dominant findings. The affected bone shows sclerosis, cortical thickening, compromised medullary canal and hypertrophy [28]. However, in tubercular osteomyelitis, sclerosis is less common with predominant osteolytic components, which helps in differentiating these two entities. In chronic osteomyelitis of SAPHO syndrome, bacterial cultures are usually negative [29]. Low virulence bacteria like Propionibacterium acne has been isolated from bone biopsy in SAPHO syndrome [30].
Uncommon neoplastic lesions like primary bone tumours e.g., osteosarcoma and Ewing sarcoma, GCT, metastasis and multiple myeloma can affect the clavicle [31] and sometimes these tumoural conditions are difficult to differentiate from SAPHO syndrome or tubercular osteomyelitis [32]. The clinico-radiological findings of present study cases were compared with the published literatures from last two decades [Table/Fig-8].
Literature review of tubercular osteomyelitis of clavicle in two decades.
| Series/year | No. of cases | Age/mean age (years) | Sex/Sex ratio | Side of affection | Site of affected clavicle | Type of bone destruction | Salient radiological findings | Sequestrum | Bony sclerosis | Treatment |
|---|
| Gerscovich EO et al., /1994 [13] | 1 | 65 | F | Right | Medial 1/3rd | Mixed lytic sclerotic | X-ray and CT: Mixed lytic-sclerotic lesion without periosteal reaction | - | + | - |
| Shah J et al.,/2000 [15] | 2 | 36.5 | M:F(0:2) | R:L(1:1) | Middle 1/3rd:1 Medial 1/3rd:1 | Lytic | X-ray (n=2): lytic lesions with erosions in affected clavicle in 2 patientsCT (n=1): lytic destruction of middle 3rd of clavicleMRI (n=1): medial 3rd of clavicular destruction | - | - | - |
| Basanagodar PL et al., /2001 [11] | 1 | 30 | F | Right | Lateral 1/3rd | Lytic | X-ray: Expansile osteolytic lesion in lateral end of clavicle with soap bubble appearance | - | - | ATT only |
| Verma S et al.,/2008 [33] | 1 | 22 | F | Right | Medial 1/3rd | Lytic | X-ray: Osteolytic lesion | - | - | ATT only |
| Aggarwal AN et al.,/2009 [9] | 4 | 16.25 | M:F (0:4) | R:L (1:3) | Medial 1/3rd:1Middle 1/3rd: 1Lateral 1/3rd: 1Lateral 2/3rd: 1 | Mixed : 1Lytic: 2Expansile lytic: 1 | X-ray: (n=4)Osteolytic lesion: 1Lytic lesion with sclerosis-1Expansile lytic lesion: 1Soft tissue defect with lytic bony destruction:1CT (n=2): Area of destruction with mild soft tissue swelling:1;Erosion and fragmentation with soft tissue swelling:1 | - | +(1 case) | ATT only |
| Dugg P et al., /2013 [2] | 1 | 35 | M | Right | Lateral 1/3rd | Mixed lytic sclerotic | X-ray: Mixed lytic with sclerotic lesions of the lateral 1/3rd of clavicle. | + | + | ATT only |
| Agarwal A and Maheshwari R/2014 [17] | 1 | 61 | M | Left | Lateral 1/3rd | Mixed lytic-sclerotic | X-ray: Pathological fracture with sequestrum and periosteal reaction | + | + | ATT+ seques-trectomy + sinus tract excision |
| Agarwal A and Pruthi M/ 2011 [34] | 3 | 7 | M:F (3:0) | R:L (1:2) | Medial 1/3rd :1Lateral 1/3rd: 1Diffuse : 1 | Expansile lytic: 1Bone oedema:1 | X-ray (n=3): Normal in 1; Expansile and lytic lesion in 1; Lytic lesions with Pathological fracture in 1 patient.CT (n=1): Expansile and lytic lesionMRI (n=1): Bone marrow oedema | - | + (1 case) | ATT only: 2ATT + debrid-ement: 1 |
| Akhtar MN et al.,/2015 [35] | 1 | 41 | F | Right | Medial 1/3rd | Sclerotic | X-ray: NormalCT: Sclerotic lesionMRI: loss of marrow signal with post contrast enhancement. | - | + | ATT only |
| Present study | 8 | 37 | M:F (6:2) | R:L (3:5) | Medial 1/3rd:4Medial 2/3rd: 1Lateral 1/3rd: 2Both ends: 1 | Expansile lytic: 5Fine erosions: 3 | X-ray (n=8): Osteolytic lesions in 4 (50%) patients, pathological fracture in 1 (12.5%) patient and unremarkable in 3 (37.5%) patients.CT findings (n=6): Expansile osteolytic lesions in 3 (50%) patients and fine bony erosions in 3 (50%) patients.MRI findings (n=2): Loss of marrow signals with expansile bony lesions with surrounding thick peripherally enhancing collections in 1 patient;And pathological fracture of clavicle with adjacent loculated thick peripherally enhancing abscesses in another 1 patient. | 2 cases | + (4 cases) | ATT+ debrid-ement: 5 casesATT only: 3 cases |
The confirmative diagnosis of tubercular osteomyelitis is usually based on demonstration of granulomas on histopathology. Demonstration of acid-fast bacilli, which is usually the gold standard for diagnosis, is extremely rare in these lesions [10]. Timely diagnosis and multi-drug ATT treatment remains the mainstay for clavicular tubercular osteomyelitis [3,9]. Surgical management requires in situations like impending abscess rupture, uncertain diagnosis or when medical treatment fails [4].
Early institution of ATT with or without surgical debridement will lead to good clinical and haematological response with radiological resolution of the lesions and thus preventing further complications.
Limitation
The present prospective study including radiological assessment of only 8 patients of tubercular osteomyelitis of clavicle in one and half year duration. We look forward to do a study in future including a larger sample size in a longer study duration.
Conclusion
Clavicle is an uncommon location of tubercular osteomyelitis and is a great mimicker of other diseases, which leads to a diagnostic delay. Hence tubercular osteomyelitis of clavicle should be kept in the differential diagnosis of any swellings associated with chronic non-healing ulcers and overlying sinus tracts formations. We would like to emphasise the fact that a radiological picture of an osteolytic expansile lesion involving the clavicle with or without cortical destruction with overlying soft tissue swelling warrants inclusion of TB in the differential diagnosis.
SP: Smooth peripheral enhancement; PE: Phlegmonous enhancement; IP: Thicker irregular peripheral enhancement; ATT: Anti-tubercular; SCJ: Sternoclavicular joint; LAP: Lymphadenopathy