Gorham’s Syndrome Associated with Chiari I Malformation and Recurrent Meningitis without Fistula: Case Report
Fernando Antônio Oliveira Costa1, Othello Moreira Fabião Neto2, Frederico Lima Gibbon3, Guilherme Gago Silva4, Luciana Azambuja Al Alam5
1 MD, PhD, Department of Neurosurgery, Universidade Católica de Pelotas, Pelotas, Rio Grande do Sul, Brazil.
2 MD, MSc, Department of Neurosurgery, Universidade Católica de Pelotas, Pelotas, Rio Grande do Sul, Brazil.
3 Medical Student, Department of Neurosurgery, Universidade Católica de Pelotas, Pelotas, Rio Grande do Sul, Brazil.
4 Medical Student, Department of Neurosurgery, Universidade Católica de Pelotas, Pelotas, Rio Grande do Sul, Brazil.
5 Medical Student, Department of Neurosurgery, Universidade Católica de Pelotas, Pelotas, Rio Grande do Sul, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Frederico Lima Gibbon, Av. Major Carlos Pinto 123, Casa 14, Rio Grande, Rio Grande do Sul, Brazil.
E-mail: fredericogibbon@gmail.com
Gorham’s syndrome is a rare osteolytic disease in which progressive and spontaneous resorption of bone occurs. We present a case of a boy who presented with Chiari I malformation and recurrent meningitis without fistula. The patient was submitted to occipital bone biopsy and due to lymphocytic infiltration and intraosseous vascular ectasia the diagnosis of Gorham-Stout Syndrome was made. The patient underwent conservative treatment but, unfortunately he died by cardiorespiratory arrest secondary to atlanto-occipital dislocation. This case emphasizes the rarity of this pathology and the previously unreported association with recurrent meningitis without fistula.
Lymphangiomatosis, Osteolysis, Skull base
Case Report
An eight-year-old male patient arrived at the Hospital for the first time in 2008, with chief complaint of torticollis and neck pain.
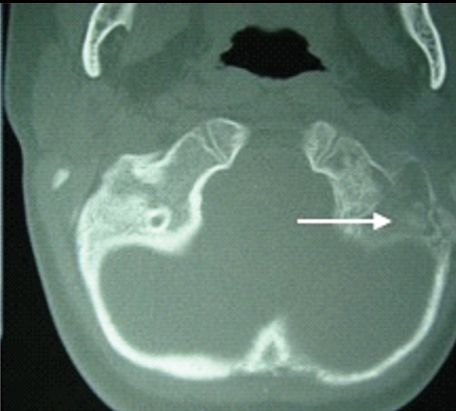
Four years before the admission he was hospitalized to treat acute bacterial meningitis at another hospital. Six months later, the patient was again admitted to the same hospital with a diagnosis of recurrent bacterial meningitis. Computed Tomography (CT) scan of the head was performed during this second infectious episode and heterogeneous abnormalities were detected in the occipital bone [Table/Fig-1] and left mastoid process [Table/Fig-2]. A biopsy of the occipital bone was performed, which showed chronic osteomyelitis. The infection was considered to be resolved after 60 days of the treatment with broad spectrum antibiotics.
CT scan of the head, bone window, showing osteolytic lesion on the occipital bone mostly on the left side (black arrow).
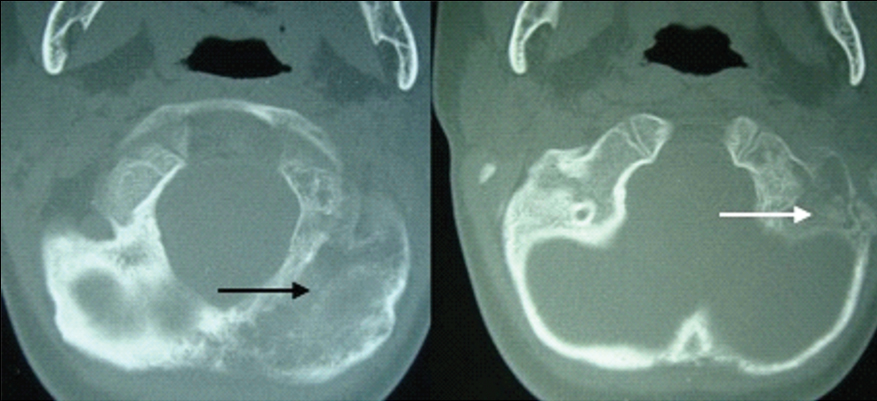
CT scan of the head, bone window, showing osteolyitc lesion on the left mastoid process (white arrow).
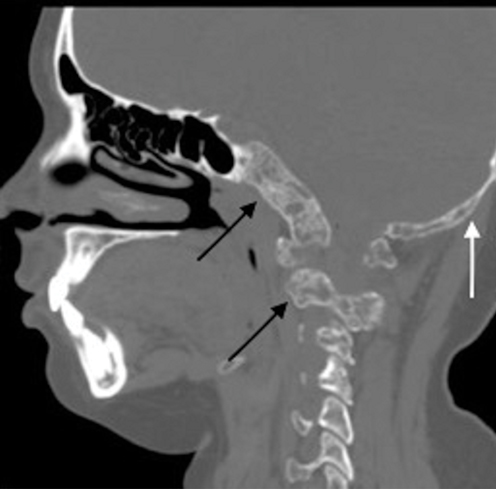
At the first time we evaluated the patient, neurological examination revealed gait disturbance, mild spastic tetraparesis and bilateral signs of pyramidal release. MRI of the head and cervical spine were performed, identifying Chiari I malformation associated with cervical syringomyelia and osteolytic lesions of the occipital bone and in the four upper vertebrae [Table/Fig-3]. The patient was submitted to a posterior fossa decompressive craniectomy. The gross specimen was a spongy cortical bone with some foci of necrosis. The tissue had poor bone marrow and fibrotic accumulation of lymphocytes and plasma cells. Intraosseous dilated blood vessels were also seen.
MRI of the head and cervical spine, T2-weighted, showing caudal displacement of cerebellar tonsils suggesting Chiari I malformation (white arrow) and cervical syringomyelia (red arrow). There is also hyperintensity of the skull base bones and the four upper cervical vertebrae (grey arrows).

After an extensive analysis, the conclusion was that histological and radiological findings were suggestive of a benign vascular lesion that affects bone and soft tissues such as angiomatosis or vascular malformation. Despite this, the exact aetiology could not be defined at this time.
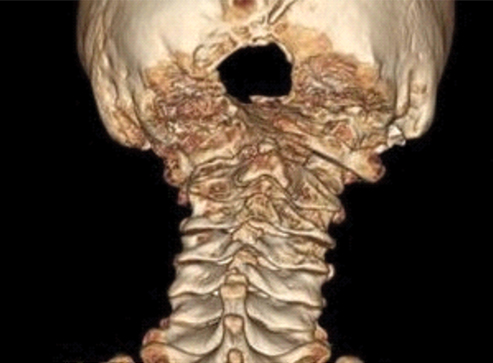
The patient maintained a normal life during the two years following surgery, but after this period, cervical pain recurred and a new investigation with radiological images [Table/Fig-4,5 and 6] identified that both the cervical and the skull base lesions had progressed, showing signs of osteolysis and bone resorption. The patient had no other complaints. Therefore, Gorham’s disease was confirmed after thorough investigation. At this point, we proposed a palliative treatment with zoledronic acid and interferon alpha-2β. Despite our efforts, the patient died due to destruction of the cervical skull transition and consequent medullary bulb compression.
CT scan of the head and upper cervical spine, showing osteolysis and bone resorption at the craniocervical junction (black arrows). There is also focal calvarial thinning at the occipital region (white arrow).
CT scan of the head and upper cervical spine, 3D reconstruction, posterior view, revealed osteolytic destruction of the bone elements of the craniocervical junction.
CT scan of the head, bone window, showing massive osteolysis of the skull base bones, more pronounced at the occipital bone (white arrow), clivus (black arrow) and left mastoid process (red arrow).

Discussion
Gorham’s disease, also known as disappearing bone disease, is a rare bone disorder characterized by lymphangiomatosis of bone which leads to massive osteolysis and replacement of bone with fibrosis and vessels. This condition may affect any bone and occur at any age, although it is most often in upper arm or shoulder, girdle and mandible [1,2]. The signs and symptoms are normally related to region affected. It does not exhibit inheritance pattern or preference for gender or race. Further, history of trauma, as a trigger, has been quite associated.
The pathophysiology is still poorly understood, however it has been well described in the literature the involvement of a proliferation of thin-walled and endothelial-lined capillary. Lymphatic vessels can also be found. The role of osteoclasts is still controversial. In spite of being a benign condition, the angiomatous proliferation may affect the adjacent soft tissue, leading to its destruction. The osteolysis usually arrests spontaneously, but there is not any specific sign related to when it will happen, which makes its behaviour difficult to predict [2].
The diagnosis of Gorham’s disease is performed by clinical, radiological and histopathological assessment, seeing that laboratorial tests have not shown any role in this. Despite the fact of MRI routinely used for investigation of the underlying cause of the disease, CT scane imaging plays a very important role since it is through this that the osteolysis will be clearly evidenced.
During the research in the literature, we found solely eight cases about Gorham’s disease associated and Chiari I malformation [1,3-8]. However, this seems to be a considerable data since it is estimated to have approximately 200 cases reported, which are spread by all regions of the body and not only skull base. Jea A et al., has proposed a mechanism about how this could happen [8]. Furthermore, whether decompressive surgery is the management of choice is still under discussion [1,6].
The association between meningitis and Gorham’s disease seems not to be a rare finding, for the reason that the lymphangiomatous process predispose to Cerebrospinal Fluid (CSF) leakage which provides free entry for microorganisms. However, we found only six cases in the literature and all these reports were related to fistula of the petrous bone [1,9-13]. In our case, the patient presented with recurrent meningitis without any evidence of fistula. If only lymphangiomatous process by itself predispose to bacterial infections or it causes micro lesions in the dura allowing the entry of microrganisms, we did not find any evidence.
The management of Gorham’s disease is still unclear. Treatment options such as interferon alpha-2β, corticosteroid, vitamin D, pamidronate, calcium supplementation, zolidronic acid, somatotrophic hormone have been used without success [2,6]. The role of radiation therapy remains uncertain. Even though some reports have shown some success, there is also an issue related to worsening of lymphatic obstruction that cannot be ignored [8]. In fact, treatment is usually symptomatic to date. Schell A et al., have reported a case of an occipito-cervical-thoracic fusion which was successfully treated [14]. Our patient was palliatively treated with interferon alpha-2β and zoledronic acid in a desperate attempt to prevent the progression of the disease. Nonetheless, to date we unfortunately agreed that a spinal fusion probably would have been more effective.
Conclusion
Gorham’s disease is a benign and self-limiting condition. We reported the first case of Gorham’s disease associated with Chiari I malformation and recurrent meningitis without fistula. Although both associations of recurrent meningitis and Chiari I malformation are found to be rare in the literature, we believe that these conditions are intrinsically related to Gorham’s disease.
[1]. Nagashima H, Mizukawa K, Taniguchi M, Yamamoto Y, Kohmura E, Cerebrospinal fluid leakage and Chiari I malformation with Gorham’s disease of the skull base: A case reportNeurol Neurochir Pol 2017 51(5):427-31.10.1016/j.pjnns.2017.06.00728743389 [Google Scholar] [CrossRef] [PubMed]
[2]. Choma ND, Biscotti C V, Bauer TW, Mehta AC, Licata AA, Gorham’s syndrome: A case report and review of the literatureAm J Med 1987 83(6):1151-56.10.1016/0002-9343(87)90959-4 [Google Scholar] [CrossRef]
[3]. Pavanello M, Piatelli G, Ravegnani M, Consales A, Rossi A, Nozza P, Cystic angiomatosis of the craniocervical junction associated with Chiari I malformationChild’s Nerv Syst 2007 23(6):697-700.10.1007/s00381-006-0274-517219234 [Google Scholar] [CrossRef] [PubMed]
[4]. Agrawal R, Mohammed I, Reilly PG, Duropleural fistula as a consequence of Gorham-Stout syndrome: A combination of 2 rare conditionsJ Thorac Cardiovasc Surg 2006 131(5):1205-06.10.1016/j.jtcvs.2006.01.02316678627 [Google Scholar] [CrossRef] [PubMed]
[5]. Girn HRS, Towns G, Chumas P, Holland P, Chakrabarty A, Gorham’s disease of skull base and cervical spine- Confusing picture in a two year oldActa Neurochir (Wien) 2006 148(8):909-13.10.1007/s00701-005-0806-x16791440 [Google Scholar] [CrossRef] [PubMed]
[6]. Coulter IC, Khan SA, Flanagan AM, Marks SM, Chiari i malformation associated with Gorham’s disease of the skull baseClin Neurol Neurosurg 2014 116:83-86.10.1016/j.clineuro.2013.11.00724300744 [Google Scholar] [CrossRef] [PubMed]
[7]. Hughes BD, Grant GA, Cummings TJ, Fuchs HE, Disappearing bone disease and Chiari i malformationPediatr Neurosurg 2010 46(1):58-61.10.1159/00031500520516742 [Google Scholar] [CrossRef] [PubMed]
[8]. Jea A, McNeil A, Bhatia S, Birchansky S, Sotrel A, Ragheb J, A rare case of lymphangiomatosis of the craniocervical spine in conjunction with a Chiari I malformationPediatr Neurosurg 2003 39(4):212-15.10.1159/00007247412944703 [Google Scholar] [CrossRef] [PubMed]
[9]. Evans DA, Baugh RF, Gilsdorf JR, Heidelberger KP, Lymphangiomatosis of skull manifesting with recurrent meningitis and cerebrospinal fluid otorrheaOtolaryngol Head Neck Surg J 1990 103(4):642-46.10.1177/0194599890103004202123326 [Google Scholar] [CrossRef] [PubMed]
[10]. Cushing SL, Ishak G, Perkins JA, Rubinstein JT, Gorham-Stout syndrome of the petrous apex causing chronic cerebrospinal fluid leakOtol Neurotol 2010 31(5):789-92.10.1097/MAO.0b013e3181de46c520502378 [Google Scholar] [CrossRef] [PubMed]
[11]. Nazarian GK, Gebarski SS, Niparko JK, Cranial lymphangiomatosis causing csf otorrhea and recurrent meningitis: ct featuresJ Comput Assist Tomogr 1990 14(1):121-23.10.1097/00004728-199001000-000232298975 [Google Scholar] [CrossRef] [PubMed]
[12]. Morimoto N, Ogiwara H, Miyazaki O, Kitamuara M, Nishina S, Nakazawa A, International Journal of Pediatric Otorhinolaryngology Gorham – Stout syndrome affecting the temporal bone with cerebrospinal fluid leakageInt J Pediatr Otorhinolaryngol 2013 77(9):1596-600.10.1016/j.ijporl.2013.06.00423827687 [Google Scholar] [CrossRef] [PubMed]
[13]. Hernández-Marqués C, González AS, Ortega FC, Alvarez-Coca J, Cerda SS, Lechón FC, Gorham-Stout disease and cerebrospinal fluid otorrheaPediatr Neurosurg 2011 47(4):299-302.10.1159/00033687722456030 [Google Scholar] [CrossRef] [PubMed]
[14]. Schell A, Rhee JM, Allen A, Andras L, Zhou F, Surgical management of Gorham disease involving the upper cervical spine with occipito-cervical-thoracic fusion: a case reportSpine J 2016 16(7):467-72.10.1016/j.spinee.2016.02.02026975457 [Google Scholar] [CrossRef] [PubMed]