Stress Among Pregnant Women: A Systematic Review
Maria Pais1, Murlidhar V. Pai2
1 Assistant Professor, Department of Obstetrics and Gynaecology Nursing, Manipal College of Nursing, Manipal, Karnataka, India.
2 Professor and Head, Department of Obstetrics and Gynaecology Nursing, Manipal College of Nursing, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Maria Pais, Assistant Professor, Department of Obstetrics and Gynaecology Nursing, Manipal College of Nursing, Manipal-576104, Karnataka, India.
E-mail: mariapuso@gmail.com
Introduction
Stress is a complex situation which is genetically determined pattern of response of the human physiology to a challenging situation. Persistent emotional neglect and constant stress response reflects differences in individual behavior, as well as differences in physical strength or general physical condition.
Aim
To systematically review the available literature on stress and its adverse effect on pregnant women.
Materials and Methods
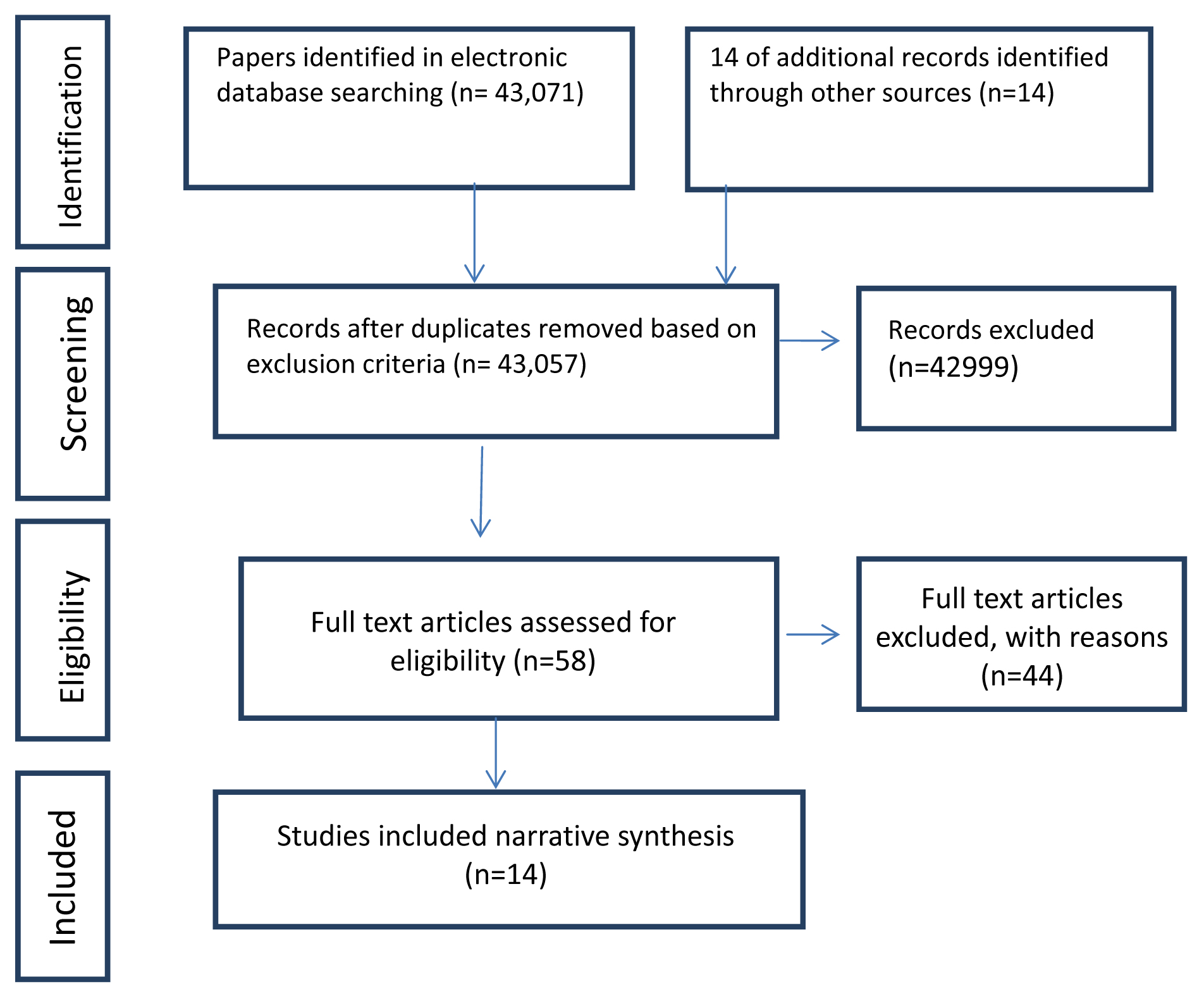
A comprehensive review from PubMed and CINAHL database was done from 1998 to 2015. Search strategy specific to each database was used. During initial search 43,071 titles were retrieved and after screening 58 articles were selected for eligibility. Finally 14 research articles were selected based on the inclusion criteria.
Results
All the 14 studies showed that increased maternal stress was associated with gravidity, gestational age at delivery, monthly family income, prematurity and preterm delivery. The maternal stress present during antenatal period for a long time has adverse effect on foetal and maternal outcomes.
Conclusion
Antenatal stress during pregnancy has adverse effect on maternal and foetal outcomes. Hence, maternity healthcare provider should understand the consequences of antenatal stress leading to long term effect. The health care providers can offer educational material as well as conduct programs to improve the maternal and infant health and initiate healthy therapeutic measures for all pregnant women.
Anxiety, Maternal, Prenatal care, Psychosocial factors
Introduction
Psychosocial stress during pregnancy is, “the imbalance that antenatal mother feels when she cannot cope with demands, which are shown both behaviourally and physiologically”. The emotions and experiences during antenatal period impinge on her developing foetus [1]. Some researchers believe that severe stress during pregnancy harms mother infant relationship and reduce mother’s ability to play motherly role [2]. It is normal for a pregnant woman to be psychologically unsteady and tensed about her health, baby’s wellbeing and the likely changes which will take place in her life after the birth of the child. Mild stress during antenatal period, is good for optimal development of the fetus, but if it exceeds it may lead to long term effect on the foetus, and alter the development of the foetal nervous system [3]. During pregnancy a women’s body changes in many ways due to the effect of hormones. These changes can sometimes be uncomfortable and may lead to stress during pregnancy [4].
A stressful event prior to delivery affects the infant’s health and is also associated with the mental health problems in childhood and adulthood. A recent review suggested that stress during antenatal period present for a long term has adverse effect on the mother and child [5]. Keeping this in view a systematic review was conducted to identify antenatal stress and its adverse outcome on pregnant women.
The aim of this systematic review was to identify the various studies related to antenatal stress and its adverse outcomes.
Materials and Methods
Search Strategy methods
An electronic search of articles published in various journals from 1998 to 2015 was made, search restricted to only English language, database assessed from Pubmed and CINAHL. The type of studies included was cross-sectional, evaluative and longitudinal cohort studies. The people who participated in the study were antenatal mothers from hospital and community settings. The type of studies excluded were high risk pregnant women, not original studies, case reports, qualitative studies, ancedotal reports and non-randomized studies. Studies were identified using search strategy as mentioned in the PRISMA flow chart [Table/Fig-1]. In addition 14 studies were identified through hand search through Google scholar. After assessment of titles and abstract, 42, 999 studies were excluded as they did not meet the inclusion criteria. An additional 44 articles were excluded after assessing the full text because they did not meet the inclusion criteria. The systematic search was conducted by framing the terms individually and in combination with synonyms, also according to the database. Even Google scholar was utilized to identify the key words for search strategy. The combination of the terms used are prenatal stress, perceived stress, anxiety, relaxation, stress reduction and pregnancy anxiety (e.g., prenatal care OR prenatal, stress AND prenatal care, stress disorder AND pregnant women, anxiety AND pregnant women. Total 58 studies were selected and 14 articles were screened.
Flow chart showing study selection.
Results
The available literature was searched to get 10 cross-sectional, one evaluative and three cohort studies, details of which are narrated in [Table/Fig-2] [6-19]. All the 14 studies have shown that increased maternal stress was associated with gravidity, gestational age at delivery, monthly family income, prematurity and preterm delivery. The prospective follow up is one of the largest study done by Wisborg K et al., among 19,382 singleton pregnant women indicated that mothers with psychosocial stress has the risk of still birth (p-value=0.03) [19]. The other evaluative study by Nkansah Amankra S et al., among 8064 among women who had stress during pregnancy shown risk of preterm delivery and low birth weight as depicted in [Table/Fig-2] [14]. The available literature has shown that maternal stress present during antenatal period has adverse effect on foetal and maternal outcomes. The influence of psychosocial factors on health outcomes among antenatal mothers affect either directly via physiological pathways, or indirectly via behavioral pathways that are associated with preterm delivery and still birth or developmental problem.
Summary of Antenatal stress studies.
| Author | Type and Place | Objective | Sample | Result |
|---|
| Pantha, Set al., [6] | Cross-sectional study(2014, Nepal) | Identify the prevalence of stress among antenatal women | 226 antenatal women | Antenatal stress was 34.2% in the third trimester, stress was related to women staying in nuclear family (p<0.05), the antenatal women who were satisfied with counseling and services were less stressed (p=0.05). |
| Pais Met al., [7] | Cross-sectional study(2014, India) | Identify the stress and its associated factors among antenatal women | 160 antenatal women | Antenatal women (33.3%) had moderate to severe stress and stress was significantly associated with gravidity, educational status and monthly family income. |
| Carolan M and Barry M [8] | Cross-sectional study(2014, in Ireland) | Evaluate stress anxiety levels and depressive symptoms among low risk women during second trimester. | 74 antenatal women | Majority 75.6% of antenatal women reported perceived stress level. Significant variation in mean PSS score between the dissimilar age groups (p=0.01), but no significant variation was found with different living arrangements or occupation. |
| Shishehgar, et al., [9] | Cross-sectional study(2014, Iran) | To identify the role of socioeconomic status in pregnancy stress rates and correlation between husbands’s occupation status and pregnancy stress level. | 210 pregnant women | No significant association between socio economic status and stress level (p>0.05), negative correlation between husband occupation status and stress level (r=0.364). |
| Hall WA et al., [10] | Cross-sectional survey(2012, in Canada) | To find the association between pregnant women’s psychological state and sleep deprivation and obstetrical intervention. | 650 low risk antenatal women | Antenatal women who had difficult labour reported high level fear of childbirth and obstetric interventions (p < 0.001). |
| Lynn FA et al., [11] | Cross-sectional study(2011, Ireland) | Identify the level of pregnancy related stress, specific worries and concerns experienced by low-risk pregnant women. | 278 pregnant women | Mean stress score was 15.1±7.4 (range 0-46), and multiparous women had less stress scores than primiparous women (p<0.01). |
| Woods SM et al., [12] | Cross-sectional study(2010, in U.S.) | Assess the factors associated with antenatal psychosocial stress and describe the course of psychosocial stress during pregnancy. | 1,522 pregnant women | Antenatal women reported 78% low to moderate level of stress and 6% high level of stress during pregnancy. Antenatal psychosocial stress during pregnancy is common, and high stress is associated with multiple maternal factors that are known to contribute to poor pregnancy outcomes. |
| Mishra S et al., [13] | Descriptive survey study(2010 Andra Pradesh, India) | Effects of psychosocial stressor during pregnancy on the gestational age of the newborn. | 227 pregnant women | Mean stress among antenatal women was 201.51±64.92 who had preterm delivery. Stress is also associated with preterm delivery (p=0.005). |
| Nkansah Amankra S et al., [14] | Evaluative study(2000, US) | Effects of maternal stress on low birth weight and preterm birth outcomes | 8064 antenatal women | Maternal stress was significantly associated with increased risks of preterm delivery and low birth weight (p<0.001), and also suggested stress appeared as a partial mediator of contextual effects on birth outcomes. |
| Gennaro S et al., [15] | Prospective descriptive study(2008 in Northeast, New York) | Identify the stress level at 28 weeks and over a time period among women | 59 black women | There was not a high correlation between stress measures. Perceived Stress was correlating at 28 weeksof gestation. (r=0.55, p<0.0001) |
| Faisal-Curry A and Rossai MP [16] | Cross-sectional study(2007, Osasco.) | Identify the prevalence and risk factors for antenatal anxiety and antenatal depression | 432 antenatal women | The prevalence of anxiety level was 59.5%, it was associated with women’s income and it was concluded that the prevalence of anxiety was high in antenatal women. |
| Rondo PH et al., [17] | Longitudinal cohort study(2003, in Brazil) | Identify the antenatal stress and its associations factors | 865 pregnant women, | Maternal distress was associated with low birth weight (RR=1.97, p=0.019) and prematurity (RR=2.32, p=0.015). |
| Teixeira JM et al., [18] | Cohort based study(1999, in London) | To find out association between maternal anxiety in pregnancy and increased uterine artery resistance index. | 100 pregnant women | Significant association was found between both Spielberger State Anxiety and uterine artery resistance index (p < 0.002) and anxiety (p <0.005) respectively. |
| Wisborg K et al., [19] | Prospective follow up study from 1989 to 1998 in Denmark, | To identify the association between psychological stress during pregnancy and stillbirth. | 19,282 singleton pregnant women | Antenatal women with high level of psychological stress during pregnancy had 80% increased risk of still birth (p = 0.03). |
Discussion
Research studies have confirmed that antenatal stress has adverse effects on maternal and fetal outcome. A study on antenatal stress showed that antenatal women had moderate to severe stress and stress was significantly associated with gravidity, educational status and monthly family income [7], and antenatal women who are staying in nuclear family [7], it may be due to lack of family support. Another similar study revealed that anxiety level was associated with women’s income and it was concluded that the prevalence of anxiety was high in antenatal women [16]. In contrast to this study a study done by Shishehgar S et al., in Iran, reported that no significant association was seen between socio economic status and pregnancy stress level, also had indirect correlation with husband’s occupation [9].
Multiparous women had less stress scores than primiparous women which conclude that healthy low risk antenatal women undergo the pregnancy related stress [11]. Few studies reported that if maternal stress is present during antenatal period, it has poor pregnancy outcome like intrauterine growth restriction (IUGR), prematurity, caesarian section, low birth weight and still birth [13,17,19]. Two articles were available on preterm delivery and still birth [17,19]. More researches needs to be done in this area.
Implication for Clinical Practice:
Study findings have clinical implications; stress present during antenatal period may lead to long term effect on the fetal neurodevelopment. This has an impact on infant/child psychopathology due to exposure to maternal internal environment [20-24]. The physicians and nurses must deal with physical and psychosocial wellbeing of antenatal women and make them to understand that all antenatal women are unique and may undergo different stress levels, example problem in immediate relationships, economic, social and environmental stress. They have to cope with these stress levels through the practice of different relaxation techniques [25]. The Committee on Obstetric Practice (2010) recommends that, the obstetricians should serve to protect the psychosocial integrity and maternal wellbeing during childbearing, by incorporating social support and special treatment programmes [25].
Early recognition of antenatal stress, anxiety and depression through standard stress rating scale and effective therapeutic treatment modalities is important to ameliorate some of the harmful effects of these conditions. So educating the antenatal mother during periodic antenatal checkup and teaching relaxation technique are essential.
Future research direction:
Maternity healthcare provider should understand the consequences of antenatal stress leading to long term consequences like autism and developmental abnormalities [26,27]. Health care professionals should accept the fact that every mother is unique. So educating the mother on life style factors that are associated with these problems and advising to seek healthcare during this period through counseling should be a priority. Further studies reveal the association of various factors aggravating antenatal stress and suggest preventive measures in antenatal care. In contrast to all the studies conducted in simulated or classroom settings, future studies should engage in analytical structuring of the students and reflective practice in clinical settings.
Limitation
The main limitations of the review was that only two database were considered for the review and researcher restricted the search to articles only published in English language.
Conclusion
The health care professionals should accept that every mother is different from other and educate them on complimentary therapy and life style modification. It helps to prevent adverse pregnancy outcomes. There are many strategies that can be implemented to improve the health of the mother and foetus. A multifaceted, multipronged holistic approach towards care of expectant mother will greatly improve the quality of offspring being born. As commonly said “today’s child is tomorrow’s citizen”, every health personnel involved in providing antenatal care should work towards achieving this goal during the antenatal period.
[1]. Sethre-Hofstad L, Stansbury K, Rice MA, Attunement of maternal and child adrenocortical response to child challengePsychoneuroendocrinology 2002 27(6):731-47.10.1016/S0306-4530(01)00077-4 [Google Scholar] [CrossRef]
[2]. Muller-Nix C, Forcada-Guex M, Pierrehumbert B, Jaunin L, Borghini A, Ansermet F, Prematurity, maternal stress and mother-child interactionsEarly Hum Dev 2004 79(2):145-58.10.1016/j.earlhumdev.2004.05.00215324994 [Google Scholar] [CrossRef] [PubMed]
[3]. Pickler RH, McGrath JM, Reyna BA, McCain N, Lewis M, Cone S, A model of neurodevelopmental risk and protection for preterm infantsJ Perinat Neonatal Nurs 2010 24(4):356-65.10.1097/JPN.0b013e3181fb1e7021045616 [Google Scholar] [CrossRef] [PubMed]
[4]. Ruiz RJ, Avant KC, Effects of maternal prenatal stress on infant outcomes: A synthesis of the literatureAdv Nur Sci 2005 28(4):345-55.10.1097/00012272-200510000-0000616292020 [Google Scholar] [CrossRef] [PubMed]
[5]. Huizink AC, Robles de Medina PG, Mulder EJ, Visser GH, Buitelaar JK, Stress during pregnancy is associated with developmental outcome in infancyJ Child Psychol Psychiatry 2003 44(6):810-18.10.1111/1469-7610.0016612959490 [Google Scholar] [CrossRef] [PubMed]
[6]. Pantha S, Hayes B, Yadav BK, Sharma P, Shrestha A, Gartoulla P, Prevalence of Stress among Pregnant Women Attending Antenatal Care in a Tertiary Maternity Hospital in KathmanduJ Women’s Health Care 2014 3:183-85.10.4172/2167-0420.1000183 [Google Scholar] [CrossRef]
[7]. Pais M, Pai MV, Kamath A, George A, Noronhna JA, Nayak BS, Stress among antenatal women in IndiaInternational Journal of Nursing Care 2014 2(2):63-67.10.5958/2320-8651.2014.01272.1 [Google Scholar] [CrossRef]
[8]. Carolan M, Barry M, Antenatal stress: An Irish case studyMidwifery 2014 30(3):310-16.10.1016/j.midw.2013.03.01423684696 [Google Scholar] [CrossRef] [PubMed]
[9]. Shishehgar S, Dolatian M, Majd HA, Bakhtiary M, Socioeconomic status and stress rate during pregnancy in IranGlob J Health Sci 2014 6(4):254-60.10.5539/gjhs.v6n4p25424999123 [Google Scholar] [CrossRef] [PubMed]
[10]. Hall WA, Stoll K, Hutton EK, Brown H, A prospective study of effects of psychological factors and sleep on obstetric intervention, mode of birth, and neonatal outcomes among low-risk British Columbian womenBMC Pregnancy Childbirth 2012 12:7810.1186/1471-2393-12-7822862846 [Google Scholar] [CrossRef] [PubMed]
[11]. Lynn FA, Alderdice FA, Crealey GE, McElnay JC, Associations between maternal characteristics and pregnancy related stress among low-risk mothers: An observational cross-sectional studyInt J Nurs Stud 2011 48(5):620-27.10.1016/j.ijnurstu.2010.10.002 [Google Scholar] [CrossRef]
[12]. Woods SM, Melville JL, Guo Y, Fan MY, Gavin A, Psychosocial stress during pregnancyAm J Obestl Gynecol 2010 202(1):61.e1-61.e7.10.1016/j.ajog.2009.07.041PMC2811236 [Google Scholar] [CrossRef] [PubMed]
[13]. Mishra S, Effects of psychosocial stressors during pregnancy on gestational age of the NewbornThe Orissa Journal of Psychiatry 2010 :32-37. [Google Scholar]
[14]. Nkansah-Amankra S, Luchok KJ, Hussey JR, Watkins K, Liu X, Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000-2003Matern Child Health J 2010 14(2):215-26.10.1007/s10995-009-0447-419184386 [Google Scholar] [CrossRef] [PubMed]
[15]. Gennaro S, Shults J, Garry DJ, Stress and preterm labor and birth in black womenJ Obstet Gynecol Neonatal Nur 2008 37(5):538-45.10.1111/j.1552-6909.2008.00278.x18811773 [Google Scholar] [CrossRef] [PubMed]
[16]. Faisal-Cury A, Rossi Menezes P, Prevalence of anxiety and depression during pregnancy in a private setting sampleArch Women Ment Health 2007 10(1):25-32.10.1007/s00737-006-0164-6 [Google Scholar] [CrossRef]
[17]. Rondó PH, Ferreira RF, Nogueira F, Ribeiro MC, Lobert H, Artes R, Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardationEur J Clin Nutr 2003 57(2):26610.1038/sj.ejcn.1601526 [Google Scholar] [CrossRef]
[18]. Teixeira JM, Fisk NM, Glover V, Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based studyBMJ 1999 318(7177):153-57.10.1136/bmj.318.7177.1539888905 [Google Scholar] [CrossRef] [PubMed]
[19]. Wisborg K, Barklin A, Hedegaard M, Henriksen TB, Psychological stress during pregnancy and stillbirth: prospective studyBJOG 2008 115(7):882-85.10.1111/j.1471-0528.2008.01734.x18485167 [Google Scholar] [CrossRef] [PubMed]
[20]. Maharana S, Nagarathna R, Padmalatha V, Nagendra HR, Hankey A, The effect of integrated yoga on labor outcome: a randomized controlled studyInt J Childbirth 2013 3:165-77.10.1891/2156-5287.3.3.165 [Google Scholar] [CrossRef]
[21]. Parcells DA, Women’s mental health nursing: depression, anxiety and stress during pregnancyJ Psychiat Ment Health Nurs 2010 17(9):813-20.10.1111/j.1365-2850.2010.01588.x [Google Scholar] [CrossRef]
[22]. Satyanarayana VA, Lukose A, Srinivasan K, Maternal mental health in pregnancy and child behaviorIndian J Psychiatr 2011 53(4):351-61.10.4103/0019-5545.91911PMC3267349 [Google Scholar] [CrossRef] [PubMed]
[23]. Dunkel Schetter C, Psychological science on pregnancy: Stress processes, biopsychosocial models & emerging research issuesAnnu Rev Psychol 2011 62:531-58.10.1146/annurev.psych.031809.13072721126184 [Google Scholar] [CrossRef] [PubMed]
[24]. Buckingham JL, Donatelle EP, Thomas Jr A, Scherger JE, Family medicine: principles and practiceSpringer Science & Business Media 2013 Nov 21 [Google Scholar]
[25]. Committee opinion no. 453: Screening for depression during and after pregnancyAmerican College of Obstetricians and Gynecologists, & Committee on Obstetric PracticeObstet and Gynecol 2010 115(2):394-95. [Google Scholar]
[26]. Talge NM, Neal C, Glover V, Antenatal maternal stress and long-term effects on child neurodevelopment: how and why?J Child Psychol Psychiatry 2007 48(3-4):245-61.10.1111/j.1469-7610.2006.01714.x17355398 [Google Scholar] [CrossRef] [PubMed]
[27]. Linnet KM, Dalsgaard S, Obel C, Wisborg K, Henriksen TB, Rodriguez A, Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: review of the current evidenceAm J Psychiatry 2003 160(6):1028-40.10.1176/appi.ajp.160.6.102812777257 [Google Scholar] [CrossRef] [PubMed]