Histopathological Analysis of Dens Invaginatus in an Immature Permanent Incisor
Liming Jiang1, Xuejuan Ma2, Yao Liu3, Ming Zhong4, Xu Chen5
1 Lecturer, Department of Paediatric Dentistry, School of Stomatology, China Medical University, Shenyang, Liaoning Province, China.
2 Department of Paediatric Dentistry, School of Stomatology, China Medical University, Shenyang, Liaoning Province, China.
3 Lecturer, Department of Paediatric Dentistry, School of Stomatology, China Medical University, Shenyang, Liaoning Province, China.
4 Professor, Department of Oral Histopathology, School of Stomatology, China Medical University, Shenyang, Liaoning Province, China.
5 Professor, Department of Paediatric Dentistry, School of Stomatology, China Medical University, Shenyang, Liaoning Province, China.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Xu Chen, No. 117, Nanjing North Street, Heping Zone, Shenyang-110002, Liaoning Province, China.
E-mail: chenxu_cmu@sina.com; chenxu@cmu.edu.cn
Dens Invaginatus (DI) is a congenital development malformation. The complex anatomy of DI aids in the retention of food and bacteria, which leads to pulp necrosis and develops into periapical inflammation. The histopathology of DI is not very clear. This study reports an unusual case of a 6-year-old boy who had a malformed immature permanent mandibular central incisor with DI Type III and apical periodontitis. The malformed tooth was extracted due to the severe infection and short tooth root. Histological results showed that typical pulp tissues were in the main root canal whereas a typical granuloma existed in the invaginated part. This case report indicate that the apical periodontitis in DI Type III was mainly induced by the invaginatus canal and the pertinent treatment for the invaginatus canal was the key for DI Type III.
Cone beam computed tomography, Dens in dente, Histology, Tooth abnormality
Case Report
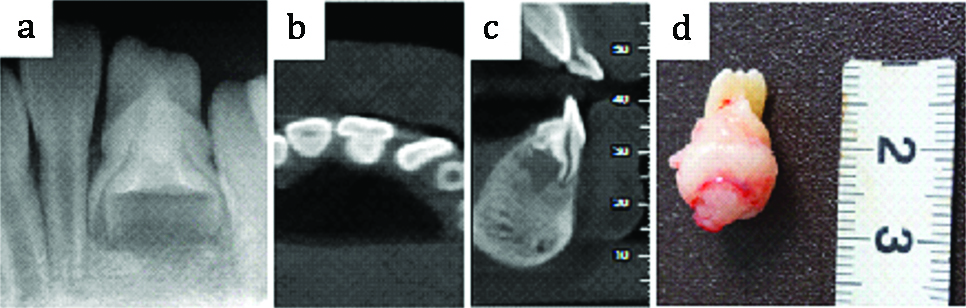
The patient was a 6-year-old boy reported to Department of Paediatric Dentistry with a chief complaint of pain and swelling in the lower left anterior region since three weeks. Clinical inspection showed that half of the crown of the permanent mandibular left central incisor (#24-according to universal system of tooth numbering) had erupted and appeared to be of normal shape and size. The tooth #24 was sensitive to percussion with class I mobility. There was a fistula on the labial gingiva between tooth lower left lateral incisor (#23) and #24. Periapical radiographic examination revealed that tooth #24 had notable periapical radiolucency and abnormal root canal structure. The root length was approximately two-third of the symmetric right incisor. Two apparent root canals (outer and inner) with open apical foramina were observed [Table/Fig-1a]. Cone Beam Computed Tomography (CBCT) examination confirmed that there was a bulge on the lingual surface in the upper part of the root [Table/Fig-1b]. The root canal of the invagination was separated from the circular external root canal [Table/Fig-1c]. Tooth extraction and mandibular removable space maintainer was suggested to the parents based on the severe infection and short tooth root. The length of the extracted abnormal tooth was about 20 mm and had a bulging root [Table/Fig-1d].
Radiographic and CBCT images and photographs of the malformed left mandibular central incisor with dens invaginatus; a) Periapical radiograph; b,c) CBCT images in a cross-section and sagittal plane; d) Post extraction specimen of mandibular cental incisor.
The Haemotoxylin and Eosin (H&E) staining showed invaginated enamel with a very thin layer of a dentin-like structure in the center of the malformed tooth [Table/Fig-2a]. Typical pulp cellular features were observed in the outer canal [Table/Fig-2b]. In the inner canal, stratified squamous epithelial hyperplasia formed nests while epithelial pegs formed the serration. The tissue in the apical end resembled typical granuloma. There were large amounts of plasma cells and lymphocyte infiltration and dilated blood vessels along with fibrous connective tissue [Table/Fig-2c,d].
Histologic sketch and photograph of the malformed left mandibular central incisor with dens invaginatus (H&E staining); a) Enamel and dentin-like structure in the invaginated region (4X); b) Pulp in the outer root canal (10X); c) Stratified squamous epithelium with the blue arrow indicating the epithelial pegs in the inner canal (4X); d) A magnified view of the boxed region in C, with the red arrow indicating the plasma cell (40X).
E: Enamel; D: Dentin; P: Pulp; Pr: Predentin; Od: Odontoblast; Cf: Cell free zone; Cr: Cell rich zone. Scale bar: (A, C) 200 μm; (B) 100 μm; (D) 50 μm.

Discussion
Dens invaginatus which is a developmental abnormity involves the invagination of accessory enamel into the dental papilla prior to dental tissue calcification, producing a tooth-like structure in the future pulp chamber [1]. DI was classified into three types by Oehlers FA [2]: Type I, invagination confined to the crown; Type II, invagination which probably contain abnomal enamel may distent and extend beyond the Cementoenamel Junction (CEJ); and Type III, invagination penetrating the root and exhibiting a second foramina in the apical third, or penetrate the lateral radicular region (direct communication with PDL). In severe DI, the Hertwig’s epithelial root sheath folds into the developing root, leading to production of enamel and dentin within the root [3]. The prevalence of DI is reported to be 0.04-10% in the general population, which is most common in the permanent maxillary lateral incisor [4,5].
The aetiology of DI malformation remains unclear and controversial. Several factors have been suggested to cause DI, including infection, trauma, genetic factors, growth pressure of the dental arch, rapid and aggressive proliferation of a part of the internal enamel epithelium invading the dental papilla, focal failure of growth of the internal enamel epithelium, fusion of two tooth germs, and distortion and subsequent protrusion of the enamel organ during tooth development [6,7].
In this case, the most possible pathogenic factor contributing to the malformation of the mandibular central incisor could be dens in dente Type III, which is the most serious type of DI.
With regard to the formation of granuloma at the tooth root in this case, we speculated the probability of a communication between the periapical tissues and the cavity of the invagination as well as the apical papilla due to the deformed root, which might further cause the bacteria and toxin to enter the periapical tissue and induce the infection.
In the clinic, the diagnosis of malformed teeth is difficult and complicated, yet important for preparing the treatment plan. As a particularly important and useful tool to study the complexity and variability of canal systems, CBCT is a technologically sophisticated, reliable, non invasive imaging technique with a high degree of visualisation [8,9]. Early detection facilitates the diagnosis, control, and treatment of malformed teeth. If the condition is detected before complete eruption of the tooth, the removal of gingival tissue to facilitate cavity preparation and restoration may be indicated [10]. However, in this case, it was difficult to detect this condition in the early stages due to the normal shape of the erupted crown without any symptoms.
Approaches for management of DI include prophylactic treatment, apexification, endodontic treatment, retrograde periapical surgery, intentional reimplantation, or extraction, depending on the severity of the case [11]. For teeth that have to be extracted because of extremely severe periodontal lesions or a very complicated root canal curvature, histological assessments will enrich our understanding of the development of tooth anomalies.
If DI is associated with necrosis or apical periodontitis, endodontic treatment both in the DI and the main canal is usually recommended, as communication between the canals may affect the prognosis. However, this case report highlights that in Type III, the infection could come from the invaginatus canal rather than from the main canal which contains normal dental pulp.
Conclusion
Dens invaginatus is one possible reason to lead to the periapical periodontitis of abnormal teeth. When the invagination is clearly separated from the main canal, appropriate minimally invasive treatment would be chosen individually for the DI and leave the main canal pulp undisturbed.
[1]. Hülsmann M, Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerationsInt Endod J 1997 30(2):79-90.10.1111/j.1365-2591.1997.tb00679.x10332241 [Google Scholar] [CrossRef] [PubMed]
[2]. Oehlers FA, Dens invaginatus (dilated composite odotome) I.Variations of the invaginatus process and associated anterior crown formsOral Surg, Oral Med, Oral Pathol 1957 10(11):1204-18.contd10.1016/0030-4220(57)90077-4 [Google Scholar] [CrossRef]
[3]. Brooks JK, Ribera MJ, Successful nonsurgical endodontic outcome of a severely affected permanent maxillary canine with dens invaginatus Oehlers type 3J Endod 2014 40(10):1702-07.10.1016/j.joen.2014.06.00825127930 [Google Scholar] [CrossRef] [PubMed]
[4]. Kumar H, Al-Ali M, Parashos P, Manton DJ, Management of 2 teeth diagnosed with dens Invaginatus with regenerative endodontics and apexification in the same patient: a case report and reviewJ Endod 2014 40(5):725-31.10.1016/j.joen.2013.10.03024767572 [Google Scholar] [CrossRef] [PubMed]
[5]. Gündüz K, Çelenk P, Canger EM, Zengin Z, Sümer P, A retrospective study of the prevalence and characteristics of dens invaginatus in a sample of the Turkish populationMed Oral Pathol Oral Cir Bucal 2013 18(1):e27-32.10.4317/medoral.1828523229254 [Google Scholar] [CrossRef] [PubMed]
[6]. Townsend G, Bockmann M, Hughes T, Brook A, Genetic, environmental and epigenetic influences on variation in human tooth number, size and shapeOdontology 2012 100(1):01-09.10.1007/s10266-011-0052-z22139304 [Google Scholar] [CrossRef] [PubMed]
[7]. Alani A, Bishop K, Dens invaginatus. Part 1: classification, prevalence and aetiologyInt Endod J 2008 41(12):1123-36.10.1111/j.1365-2591.2008.01468.x19133103 [Google Scholar] [CrossRef] [PubMed]
[8]. Beshkenadze E, Chipashvili N, Anatomo-morphological frutures of the root canal system in Georgian population-Cone-beam computed tomography studyGeorgian Med News 2015 (247):07-14. [Google Scholar]
[9]. Capar ID, Ertas H, Arslan H, Tarim Ertas E, A retrospective comparative study of cone-beam computed tomography versus rendered panoramic images in identifying the presence, types, and characteristics of dens invaginatus in a turkish populationJ Endod 2015 41(4):473-78.10.1016/j.joen.2014.12.00125595467 [Google Scholar] [CrossRef] [PubMed]
[10]. Dean JA, Avery DR, McDonald RE, McDonald and Avery’s Dentistry for the Child and Adolescent 2011 Mosby Elsevier:90 [Google Scholar]
[11]. Schmitz MS, Montagner F, Flores CB, Morari VH, Quesada GA, Gomes BP, Management of dens invaginatus type I and open apex: report of three casesJ Endod 2010 36(6):1079-85.10.1016/j.joen.2010.02.00220478470 [Google Scholar] [CrossRef] [PubMed]