Analysis of Functional Outcome Following Rigid Skeletal Stabilisation of Unstable Proximal and Middle Phalangeal Fractures of the Hand
Surya Rao Rao Venkata Mahipathy1, Selvan Ranganathan2, Sridharan Murugesan3, Alagar Raja Durairaj4, Narayanamurthy Sundaramurthy5
1 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
2 Associate Professor, Department of Plastic and Reconstructive Surgery, Government Chengalapttu Medical College and Hospital, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Plastic and Reconstructive Surgery, Madras Medical College, Chennai, Tamil Nadu, India.
4 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
5 Assistant Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Rao Rao Venkata Mahipathy, Flat 1B, Kameshwari Apartments, 23/35, Desika Road, Mylapore, Chennai-600004, Tamilnadu, India.
E-mail: surya_3@hotmail.com
Introduction
Phalangeal fractures commonly occur in hand injuries. As hand is a complex structure of bones, joints, ligaments, muscles, tendons and neurovascular structures, the biomechanics play an important role in mobility and dexterity of the hand. Operative fixation of these fractures with miniplates and screws allows for earlier mobilisation of the hand and hence avoids the complications of other methods of fracture fixation. This allows for shorter hospital stay and faster returns to work.
Aim
This prospective study was undertaken to evaluate and analyse the functional outcome following rigid skeletal stabilisation and early mobilisation of fractures of proximal and middle phalanges of the hand with plate and screw technique.
Materials and Methods
There were a total of 21 patients with 26 phalangeal fractures. All the data were collected from Government Chengalpattu Medical College Hospital, Chengalpattu during the period of December 2008 to December 2010. An informed written consent and x-rays of the hand were taken, pre and postoperatively. The fractures were reduced and fixed with miniplates and screws. The results were analysed using the Belsky’s criteria using the parameters of pain with or without union, deformity and total active flexion range of metacarpophalangeal and interphalangeal joints.
Results
Among the patients, 84.6% of the fractures showed an excellent or good functional outcome and 15.4% had a poor outcome following rigid skeletal stabilisation. Eighteen (86%) fractures were in male patients, of third to fourth decade, involving mainly the proximal phalanx, due to Road Traffic Accident (RTA), with six patients having complications.
Conclusion
Phalangeal fracture fixation with miniplates and screws gives a good functional outcome.
Fracture, Function, Plate and screw fixation, Total active motion
Introduction
Phalangeal fractures are common in hand trauma with an annual incidence of 0.2 to 3% of the patients attending the casualty [1-4]. Majority of phalangeal fractures are stable and can be treated non-operatively. However, unstable fractures like those with shortening, displacement, angulation, rotational deformity or segmental fractures need surgical intervention [5,6]. The main aim of operative fracture fixation is to establish fracture stability and facilitate early mobilisation of the hand to achieve functional recovery as early as possible [5,7].
In surgical treatment, reduced bone fragments are fixed by an internal or external device, denominated ‘osteosynthesis, wherein all have to meet certain requirements like stable enough to permit fracture healing, preferably being biologically inert or resorbable, allow for some micro motion, permitting endosteal and periosteal callus formation, minimise further damage to already impaired circulation of fracture fragments and to allow early mobilisation [8-10]. Most phalangeal and metacarpal fractures heal adequate in short time, without functional sequelae [4,11].
With recent advances in anaesthesia, antibiotics and technologically advanced implants, there is considerable freedom in treating these injuries, but still a number of patients end up with complications like stiffness, nonunion, malunion, and chronic pain following hand fractures [9].
Apart from patients suffering from complicated hand fracture healing, it also costs for society in workers’ compensation and medical costs, which can be substantial [10-15]. The future of hand fracture treatment lies in improving our ability to choose and properly apply appropriate treatment for the variety of patients and fractures that present, bearing in mind that each patient’s perspective of an optimal outcome is different [9].
This prospective study was undertaken to evaluate and analyse the functional outcome following rigid skeletal stabilisation and early mobilisation of fractures of proximal and middle phalanges of the hand with plate and screw technique.
Materials and Methods
This was a prospective study done over a two year period from December 2008 to December 2010. The total number of patients in the study was 21 with 26 phalangeal fractures. Data were collected from Government Chengalpattu Medical College Hospital, Chengalpattu during the period of December 2008 to December 2010. This study was carried out in collaboration with the departments of Casualty, General Surgery, Orthopaedics, Radiology, Anaesthesia, and Physiotherapy. An informed written consent was taken before carrying out any diagnostic or surgical procedure. All the investigations required were routinely done during the admission period or prior to it. X-rays of the involved hand-anteroposterior and oblique views were taken in all the cases, preoperatively as well as postoperatively. The proforma was prepared, duly filled and the results analysed.
The inclusion criteria were closed unstable phalangeal fractures and multiple phalangeal fractures. The exclusion criteria were mangled extremities or major crush injury, flexor or extensor tendon injury, associated bone loss, thumb and metacarpal fractures.
Every patient was explained regarding the procedure. Axillary block was given along with musculocutaneous nerve block. A manual pneumatic tourniquet was applied and time noted. The involved upper limb was placed on the hand table. A dorso-lateral incision was made and deepened in layers. The extensor tendon was either retracted to one side or split in the middle to expose the proximal or middle phalanx. Using a small periosteal elevator, the periosteum was elevated. With the help of the Howarth’s elevator, the soft tissue interposition between the fracture fragments was cleared. The fracture was reduced and held in alignment with bone holding forceps. These fractures were fixed with stainless 2.0 mm 2 hole or a 4 hole plate with spacer and 2.0×8 mm screws. Using a micromotor and a 1.5 mm burr, drill holes were made proximal and distal to the fracture site. Holding the plate in situ, the screws were driven into the holes with a 2 mm screwdriver with sleeve. Anatomic or near anatomic (<1-mm articular step-off) reduction and stable fixation were achieved in all patients at the time of surgical treatment. Tourniquet was released and haemostasis was secured with bipolar diathermy. If the extensor tendon had been split, it was approximated with 4-0 prolene intermittent sutures. Skin was closed with 3-0 prolene interrupted mattress sutures over two Segmuller drains. Dressing was done with paraffin gauze, dry gauze and finger crepe bandage. A volar below elbow splint was applied with wrist in neutral or 10 degrees extension, metacarpophalangeal joints in 90 degrees of flexion and interphalangeal joints straight. A sling was applied to support the anaesthetized upper limb.
Patient was shifted out to the postoperative ward. Patient was kept nil by mouth for 2 hours following which orals were allowed. Patients were put on parenteral antibiotics and analgesics. On postoperative day 1, the suture line was inspected and the patient was sent for check x-ray of the involved hand-anteroposterior and oblique views.
The average follow-up period was 12 (range, 4-24) weeks. The average time to fracture healing was 4.7 (range, 3-6) weeks. Early active motion was initiated after 1 week following surgery. Range of motion of the affected digit was measured with a use of a standard goniometer and evaluated as a proportion of Total Active Motion (TAM). Results were considered excellent, good, or poor according to criteria defined by Belsky MR et al., at 2 months postoperative [16]. Twenty one patients (84.6%) had an excellent result.
Results
Over a period of 24 months, a total of 21 patients with 26 fractures of proximal and middle phalanges were studied. There were 21 fractures of the proximal phalanx and 5 fractures of the middle phalanx. Seventeen patients had single fractures of either the proximal or middle phalanx, whereas 4 patients had multiple fractures (3 had fractures of two phalanges and 1 had fractures of 3 phalanges). Out of the 26 fractures, 16 were right sided whereas 10 were left sided. There were 18 males and 3 females in the study group. There were 6 patients in age group of 21-30 years, 9 patients in 31-40 years, 4 patients in 41-50 years and 2 patients in 51-60 years age group. Of the 21 patients, 13 fractures were due to RTA, 6 were due to assault and 2 were due to fall on the hand. There were 2 fractures involving the head, 3 neck, 16 shaft and 5 fractures involving the base. Eighteen fractures were of transverse type, 4 oblique, 2 spiral and 2 were comminuted [Table/Fig-1].
Demographics and aetiology of phalangeal fractures.
| Fracture distribution | No. of Phalanges involved | Side distribution | Sex distribution | Age distribution (Years) | Aetiology | Site involved | Type of fracture |
|---|
| PPx 21 (81%) | Single 17 (81%) | Right 16 (62%) | Male 18 (85%) | 21-30, 6 (28.5%) | RTA 13 (62%) | Head 2 (7.7%) | Trans-verse 18 (69.2%) |
| MPx 5 (19%) | Multiple 4 (19%) | Left 10 (38%) | Female 3 (15%) | 31-40, 9 (43%) | Assault 6 (28.5%) | Neck 3 (11.5%) | Oblique 4 (15.4%) |
| | | | 41-50, 4 (19%) | Fall 2 (9.5%) | Shaft 16 (61.5%) | Spiral 2 (7.7%) |
| | | | 51-60, 2 (9.5%) | | Base 5 (19.3%) | Communited 2 (7.7%) |
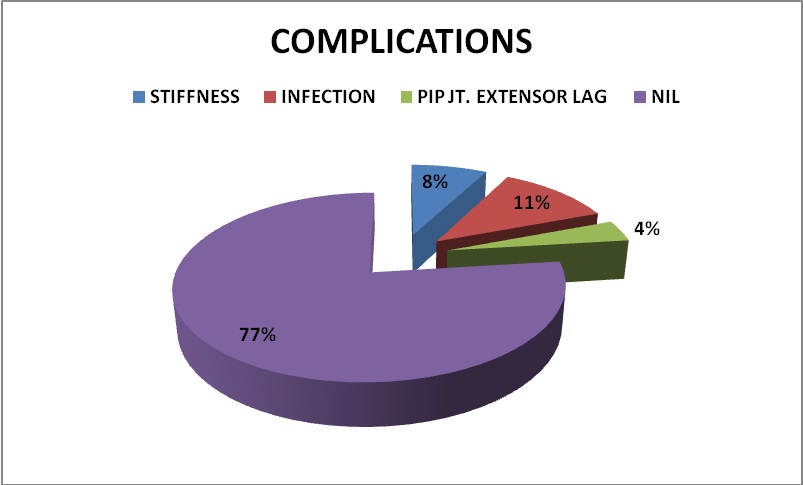
Complications: 2 Patients had stiffness, 3 had infection and 1 patient had PIP joint extensor lag [Table/Fig-2].
Pie diagram showing the complications of phalangeal fractures.
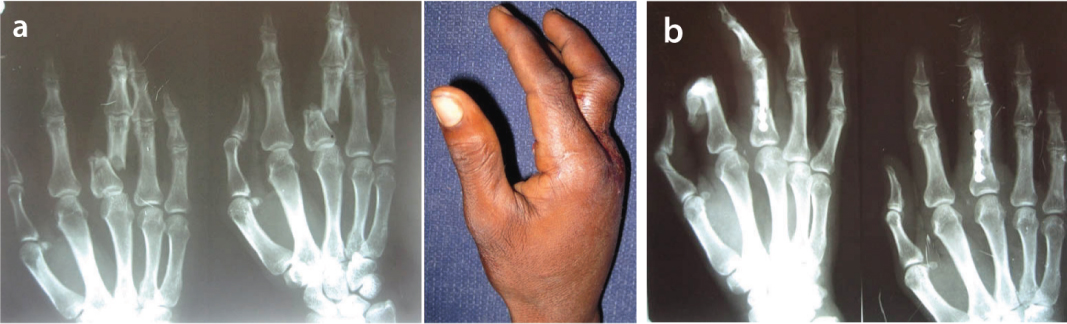
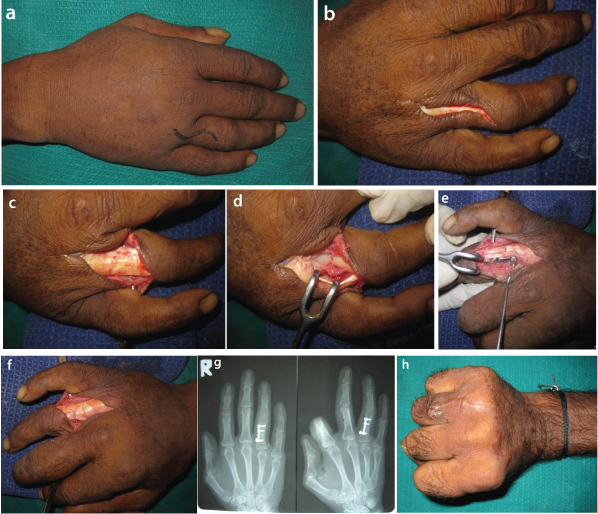
Out of the total of 26 phalangeal fractures in the study, 22 (84.6%) had excellent or good results and 4 (15.4%) had poor results following rigid skeletal stabilisation by plate and screw technique, according to the Belsky’s criteria [Table/Fig-3,4,5,6,7 and 8].
a) Communited fracture shaft of proximal phalanx rt. middle finger; b) Fracture fixed with 2.0 mm 4 hole plate and screws.
a) S-shaped incision marked; b) Lazy s incision made; c,d) Extensor tendon identified and retracted laterally to expose fracture; e) ORIF done; f) Extensor tendon placed back in position; g) Fracture fixed with miniplate and screw; h) Excellent total active motion (Belsky’s criteria).
a) Closed transverse fracture shaft of proximal phalanx rt. ring finger; b) Proximal phalanx fracture; c) X-Ray showing good alignment.

Belsky’s criteria for assesment of finger fractures.
| Excellent | Good | Poor |
|---|
| Pain-free union, and No deformity, and TAM >215°, and PIP motion >100° | Pain-free union, and minimal deformity, and TAM ≥180°, and PIP motion ≥80° | Pain or non-union, or deformity affecting function/cosmesis, or TAM <180°, or PIP motion <80 |
| Total Active Movements (TAM) is the summation of Total Active Flexion range of metacarpophalangeal and interphalangeal joints. |
PIP: Proximal Interphalangeal joint
Result of treatment according to Belsky’s criteria for finger fractures.
| Joint | Excellent | Good | Poor | Total |
|---|
| MCP | 5 | 2 | 1 | 8 |
| PIP | 5 | 5 | 2 | 12 |
| DIP | 3 | 2 | 1 | 6 |
| Total | 13 | 9 | 4 | 26 |
MCP: Metacarpophalangeal joint; PIP: Proximal Interphalangeal joint; DIP: Distal Interphalangeal joint
Results of Belsky’s criteria for different sites of phalangeal fractures.
| Fracture Pattern | Excellent | Good | Poor | Total |
|---|
| Head | 1 | 1 | - | 2 |
| Neck | 2 | 1 | - | 3 |
| Shaft | 10 | 5 | 1 | 16 |
| Base | 3 | 1 | 1 | 5 |
Discussion
Phalangeal fractures are commonly encountered fractures in hand [1]. Majority of them are stable and can be treated non-operatively. Unstable fractures as those with shortening, angulation, deformity or segmental fractures need operative intervention [5,6]. Achieving fracture stability to facilitate early mobilisation to achieve a full functional recovery of the hand as early as possible is the main aim of operative fracture fixation [5,17].
The ASIF manual recommends removing K-wires after 1-2 months and screws and plates at 4-6 months postoperatively, yet Dabezies EJ and Schutte JP report no ill effects in patients whose hardware was still in place long after surgery [18]. Freeland A and Jabaley M studied 68 minicondylar plate applications in the metacarpals and phalanges [19]. They found that approximately one third of patients had excellent final range of motion, one third had good or fair range of motion, and one third had poor range of motion. The complication rate was significantly higher in open fractures, in fractures with associated soft-tissue injury, and in fractures requiring bone grafting.
Black D et al., found that dorsal plating, with or without lag screws, provided a much more stable reduction than wire techniques in phalangeal fractures [20]. Vanik RK et al., compared the strength of various internal fixation techniques in the treatment of metacarpal fractures [21]. They concluded that plate or plate-and-screw fixation was sufficiently stable to withstand functional use of the hand, but neither a single K-wire nor crossed K-wires provide solid fixation when measured against intraosseous wire, plating, and combination intraosseous wire and K-wire.
A recent study compared the biomechanics of the hand following application of either microplates or miniplates to fractures of the metacarpal or phalanges. The authors concluded that dorsally applied miniplates provided the greatest rigidity across a fracture to a dorsal load [22]. Freeland A and Jabaley M, discuss the advantages and disadvantages of rigid internal fixation in the hand [19]. Screws and plates are said to enhance stability of the reduction by increasing friction between the fracture fragments while freeing the hand for early mobilisation. When properly used, rigid fixation devices are stress shielding, applying the load to the implant rather than to the fracture site [19,23-26]. Fracture of the phalangeal neck is mainly seen in children and is generally missed on X-rays. The fractures are usually categorised into undisplaced, partialy displaced and completely displaced, requiring ORIF [27].
Limitation
The patients were limited in the two year period to compare with K-wire fixation of the fractures. These plates were all stainless steel due to affordability factor and hence usage of titanium plates and their results couldn’t be done.
Conclusion
Rigid skeletal stabilisation of proximal and middle phalangeal fractures of the hand by open reduction and internal fixation using plate and screw technique seems to be an effective treatment method for these unstable fracture patterns.
PIP: Proximal Interphalangeal joint
MCP: Metacarpophalangeal joint; PIP: Proximal Interphalangeal joint; DIP: Distal Interphalangeal joint
[1]. Packer GJ, Shaheen MA, Patterns of hand fractures and dislocations in a district general hospitalJ Hand Surg Br 1993 18(4):511-14.10.1016/0266-7681(93)90161-8 [Google Scholar] [CrossRef]
[2]. Angermann P, Lohmann M, Injuries to the hand and wrist. A study of 50,272 injuriesJ. Hand Surg 1993 18(5):642-44.10.1016/0266-7681(93)90024-A [Google Scholar] [CrossRef]
[3]. De Jonge JJ, Kingma J, van der Lei B, Klasen HJ, Phalangeal fractures of the hand. An analysis of gender and age-related incidence and aetiologyJ Hand Surg 1994 19(2):168-70.10.1016/0266-7681(94)90157-0 [Google Scholar] [CrossRef]
[4]. Maitra A, Burdett-Smith P, the conservative management of proximal phalangeal fractures of the hand in an accident and emergency departmentJ Hand Surg 1992 17(3):332-36.10.1016/0266-7681(92)90123-J [Google Scholar] [CrossRef]
[5]. Hwa LK, Kuen CB, Ooi LC, Metacarpal and proximal phalangeal fractures-Fixation with multiple intramedullary K-wiresJ Hand Surg 2000 5(2):125-30.10.1142/S021881040000031411301506 [Google Scholar] [CrossRef] [PubMed]
[6]. Lenoble E, Goutallier D, Reduction and osteosynthesis of displaced fractures of the distal third of the fifth metacarpal with central medullary bone wiresAnn Chir Main Memb Super 1993 12(3):189-95.10.1016/S0753-9053(05)80099-7 [Google Scholar] [CrossRef]
[7]. Gupta R, Singh R, Siwach RC, Sangwan SS, Magu NK, Diwan R, Evaluation of surgical stabilization of metacarpal and phalangeal fractures of handIndian J Orthop 2007 41(3):224-29.10.4103/0019-5413.3368721139749 [Google Scholar] [CrossRef] [PubMed]
[8]. Kawamura K, Chung KC, Fixation choices for closed simple unstable oblique phalangeal and metacarpal fracturesHand Clin 2006 22:287-95.10.1016/j.hcl.2006.02.01816843795 [Google Scholar] [CrossRef] [PubMed]
[9]. Harness NG, Meals RA, The history of fracture fixation of the hand and wristClin Orthop Relat Res 2006 445:19-29.10.1097/01.blo.0000205882.73705.5016505723 [Google Scholar] [CrossRef] [PubMed]
[10]. Brennwald J, Fracture healing in the handClin Orthop 1996 327:9-11.10.1097/00003086-199606000-000038641088 [Google Scholar] [CrossRef] [PubMed]
[11]. Pun WK, Chow SP, So YC, Luk KD, Ip FK, Chan KC, A prospective study on 284 digital fractures of the handJ Hand Surg 1989 14(3):474-81.10.1016/S0363-5023(89)80006-1 [Google Scholar] [CrossRef]
[12]. Kasdan ML, June LA, Returning to work after a unilateral hand fractureJ Occup Med 1993 35(2):132-35.10.1097/00043764-199302000-000138433184 [Google Scholar] [CrossRef] [PubMed]
[13]. O’Sullivan ME, Colville J, The economic impact of hand injuriesJ Hand Surg 1993 18(3):395-98.10.1016/0266-7681(93)90072-N [Google Scholar] [CrossRef]
[14]. Hashemi L, Webster BS, Clancy EA, Courtney TK, Length of disability and cost of work-related musculoskeletal disorders of the upper extremityJ Occup Environ Med 1998 40(3):261-69.10.1097/00043764-199803000-000089531097 [Google Scholar] [CrossRef] [PubMed]
[15]. Mink van der Molen AB, Matloub HS, Dzwierzynski W, Sanger JR, The hand severity scoring system and worker’s compensation cases in Wisconsin, USAJ Hand Surg 1999 24(2):184-86.10.1054/JHSB.1998.017910372772 [Google Scholar] [CrossRef] [PubMed]
[16]. Belsky MR, Eaton RG, Lane LB, Closed reduction and internal fixation of proximal phalangeal fracturesJ Hand Surg 1984 9(5):725-29.10.1016/S0363-5023(84)80023-4 [Google Scholar] [CrossRef]
[17]. Stern PJ, Wieser MJ, Reilly DG, Complications of plate fixation in the hand skeletonClin Orthop 1987 214:5910.1097/00003086-198701000-00010 [Google Scholar] [CrossRef]
[18]. Dabezies EJ, Schutte JP, Fixation of metacarpal and phalangeal fractures with miniature plates and screwsJ Hand Surg 1986 11(2):283-88.10.1016/S0363-5023(86)80072-7 [Google Scholar] [CrossRef]
[19]. Freeland A, Jabaley M, Management of hand fractures by stable fixationPlast Reconstr Surg 1986 2:307-28.10.1007/978-1-4613-8640-7_9 [Google Scholar] [CrossRef]
[20]. Black D, Mann RJ, Constine R, Daniels AU, Comparison of internal fixation techniques in metacarpal fracturesJ Hand Surg 1985 10(4):466-72.10.1016/S0363-5023(85)80067-8 [Google Scholar] [CrossRef]
[21]. Vanik RK, Weber RC, Matloub HS, Sanger JR, Gingrass RP, The comparative strengths of internal fixation techniquesJ Hand Surg 1984 9(4):21610.1016/S0363-5023(84)80145-8 [Google Scholar] [CrossRef]
[22]. Prevel CD, Eppley BL, Jackson JR, Moore K, McCarty M, Sood R, Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical studyJ Hand Surg 1995 20(1):44-49.10.1016/S0363-5023(05)80057-7 [Google Scholar] [CrossRef]
[23]. Fyfe IS, Mason S, The mechanical stability of internal fixation of fractured phalangesHand 1979 11(1):50-54.10.1016/S0072-968X(79)80009-1 [Google Scholar] [CrossRef]
[24]. Jones WW, Biomechanics of small bone fixationClin Orthop 1987 214:11-18.10.1097/00003086-198701000-00004 [Google Scholar] [CrossRef]
[25]. Muller ME, Manual of Internal Fixation 1979 2nd EdNew YorkSpringer:27910.1007/978-3-642-96505-0 [Google Scholar] [CrossRef]
[26]. Jabaley ME, Peterson HD, Early treatment of war wounds of the hand and forearm in VietnamAnn Surg 1973 177:167-73.10.1097/00000658-197302000-000074572781 [Google Scholar] [CrossRef] [PubMed]
[27]. Al-Qattan MM, Phalangeal neck fractures in children: Classification and outcome in 66 casesJ Hand Surg Br 2001 26(2):112-21.10.1054/jhsb.2000.050611281661 [Google Scholar] [CrossRef] [PubMed]