Misdiagnosis of Central Motor Dysfunction in a Child with Craniovertebral Junction Anomaly-A Case Report
Kriti Mishra1, Judy A David2
1 Senior Resident, Deparment of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Professor, Department of Physical Medicine and Rehabilitation, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kriti Mishra, B-503, Sumadhur 2 Apt, Behind Azaad Society, Ambawadi, Ahmedabad-380006, Gujarat, India.
E-mail: kritimishra1@yahoo.co.in
Congenital anomalies of the Craniovertebral Junction (CVJ), though clinically significant, have often been misdiagnosed especially in the paediatric age group. Timely diagnosis and interventions can improve clinical outcome and prevent complications. Better understanding of the regional anatomy and pathophysiology of anomalies along with a strong clinical suspicion, accurate examination of clinical signs and better clinical correlation can aid in early diagnosis. We illustrate the above by exploring the clinical scenario of an 11-year-old female child with multiple CVJ anomalies resulting in spastic qaudriparesis and thereby, discuss what could have prevented the delay in diagnosis.
Motor milestones, Perinatal asphyxia, Spastic quadriparesis
Case Report
An 11-year-old girl presented to the Department of Physical Medicine and Rehabiliation with spastic quadriparesis. Her birth history was suggestive of probable perinatal asphyxia. She was born by caesarean section at 38 weeks, indication being rupture of membranes and subsequent decreased fetal heart rate. She required tactile stimulation for her first cry and her birth weight was 3.5 kg. Breast feeding was initiated immediately. She did not require any intensive care admission.
All her gross and fine motor milestones were delayed with head control at two and half years, roll over (only onto her left) at seven to eight months, sitting with maximum support at three to four years and standing with maximum support at five to six years. She was able to pick up moderate size objects with her left hand and also draw simple pictures with set up.
Her language and social milestones were age appropriate and she performed well academically at school. However, she did not achieve bladder and bowel continence and was managed with diapers. She was assisted by her mother in all her daily activities and for mobility.
She was treated for recurrent urinary tract infections since infancy. Mild chewing difficulty at three years and decreased sensations on the right side of body at four years was also reported.
A diagnosis of Central Motor Dysfunction (CMD) was made by a local neurologist considering probable birth asphyxia and delayed motor milestones for which she was on regular physiotherapy. Regular monitoring of head circumference for four to five months was done to rule out hydrocephalus. X-ray cervical spine done at two years for restricted neck movements was reported as normal. Blood tests were done twice to rule out thyroid dysfunction. By four and half years of age, in May 2006, she underwent bilateral multiple soft tissue release for spasticity, calcaneal osteotomy with K-wire fixation for foot deformities and bilateral femoral rotational osteotomies. Inspite of this, she had worsening of her spasticity and a second opinion was sought when she was 10 years of age.
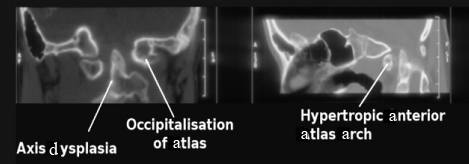
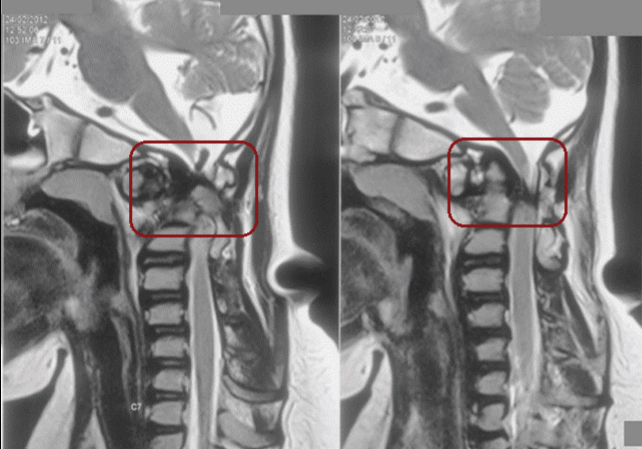
This time, cervical spine CT scan was done considering her short neck as shown in [Table/Fig-1]. It revealed multiple CVJ anomalies namely, condylar hypoplasia with partial atlanto-occipital assimilation (occipitalisation of atlas) on left side, axis dysplasia, split atlas, atlantoaxial subluxation, fusion of first and second cervical vertebrae, basilar invagination and marked cervicomedullary compression as evident in [Table/Fig-2,3]. MRI brain screening done was normal.
Child with short neck and low posterior hair line.

Craniovertebral anomalies on CT imaging.
Sagittal section of MRI showing basilar invagination and marked cervicomedullary compression (marked in brown).
She underwent transoral odontoidectomy with occipito-C3 fixation with occipital loop in April 2012. Post surgery, she required ventilatory support for one day and was flaccid for nearly one month. There has been gradual recovery in tone and voluntary control thereafter and she has been on a rehabilitation programme to improve her motor control and functioning from a wheelchair.
An informed, written consent was taken from the care givers of child for the present case report.
Discussion
CVJ (comprising of the occiput, atlas and axis) can be affected by congenital, developmental and acquired abnormalities. Anomalies involving CVJ have been a topic of speculation and medical research since the second half of 19th century [1]. In spite of advances in neuro diagnostic imaging, timely diagnosis of CVJ anomalies is often delayed. Early diagnosis in paediatric age group is often hindered owing to complex regional anatomy, low clinical suspicion and confusing radiological picture (due to immature bones with ossification around nine years) [1,2]. A number of congenital CVJ anomalies have been described [3,4]. In condylar hypoplasia, the occipital condyles are underdeveloped and the lateral mass of atlas vertebra may fuse with hypoplastic condyles. This fusion (partial or complete) is called atlas assimilation and occurs in 0.25% of general population [3,4]. This congenital anomaly invariably leads to basilar invagination (upward migration of odontoid process of axis vertebra onto assimilated atlas). Basilar invagination is associated with neural dysgenesis (like Chiari malformation or syringomyelia) in 25-35% of patients and can cause cervicomedullary compression as well [3,4]. Atlas assimilation is also associated with increased prevalence of fusion of second and third cervical vertebrae (axis-C3). This leads to gradual loosening of atlantodental joint with progressive atlantoaxial subluxation (reported in 50% cases) [3,4].
Klippel Feil syndrome is congenital fusion of cervical spine ranging from two segment fusion to entire cervical spine involvement. This is associated with clinical triad of short neck, low posterior hairline and limitation of neck movement. Other systemic involvement like renal, cardiac, musculoskeletal anomalies are well known with this syndrome [3-5]. Split atlas is rare anomaly involving anterior and posterior rachischisis of the atlas [3].
Most of the above mentioned anomalies have been found in the imaging of the child described. For a child with delayed motor developmental milestones and spastic quadriparesis, it is important to consider differentials other than CMD. The initial presentation of the child during her early years with spastic quadriparesis (right affected more than left), decreased sensation on right side, bladder and bowel incontinence with normal cognition was more in favour of a spinal disorder rather than cerebral involvement. A spastic quadriparesis type of CMD is often known to have cognitive and speech deficits more than other subtypes [6]. The sensory deficits seen in CMD including the hemiplegic type are mostly bilateral [7].
There have been some reports of CVJ congenital anomalies being initially misdiagnosed as CMD [8,9]. Besides, the classic ‘clinical triad’ is not seen in a child having only cerebral palsy and has been described for Klippel Feil syndrome due to cervical vertebrae anomalies, as per literature [5]. The only CVJ anomaly seen in association with cerebral palsy is os odontoidenum (anomaly of odontoid process causing atlantoaxial instability) in dystonic sub type of CMD children [10,11]. On the other hand, 50% cases of congenital atlanto-occipital anomalies have been found to be associated with C1-C2 subluxation or dislocation leading to C1-C2 instability [9,12].
The above mentioned child underwent orthopaedic surgeries for the spasticity of her lower limbs due to the misdiagnosis of CMD, when she would have benefitted with an early cervical spine decompression. This, in turn, impacted subsequent rehabilitation interventions, which affected the neurological and functional outcome of child significantly.
Conclusion
Hence, the report highlights the need to carefully scrutinise basis of diagnosis for infants and younger children, regularly on each visit. A good clinical suspicion and meticulous clinical examination of subtle signs is important to avoid missing the proper diagnosis and can help in early interventions, thereby, improving clinical outcome.
[1]. Goel A, Basilar invagination, Chiari malformation, syringomyelia: a reviewNeurol India 2009 57(3):23510.4103/0028-3886.5326019587461 [Google Scholar] [CrossRef] [PubMed]
[2]. Kale SS, Ailawadhi P, Yerramneni VK, Chandra PS, Kumar R, Sharma BS, Pediatric bony craniovertebral junction abnormalities: Institutional experience of 10 yearsJ Pediatr Neurosci 2011 6(1):S91-S95.10.4103/1817-1745.8572122069436 [Google Scholar] [CrossRef] [PubMed]
[3]. Smoker WR, Craniovertebral junction: normal anatomy, craniometry, and congenital anomaliesRadioGraphics 1994 14(2):255-77.10.1148/radiographics.14.2.81909528190952 [Google Scholar] [CrossRef] [PubMed]
[4]. Menezes AJ, Craniovertebral junction abnormalities. section iii congenital and developmental spinal disorders. In: Albright AL, Pollack IF, Adelson PDPrinciples and Practice of Pediatric Neurosurgery 2007 2nd edNew YorkThieme Medical Publishers [Google Scholar]
[5]. Copley LA, Dormans JP, Cervical spine disorders in infants and childrenJ Am Acad Orthop Surg 1998 6(4):204-14.10.5435/00124635-199807000-000029682083 [Google Scholar] [CrossRef] [PubMed]
[6]. Horstmann H, Bleck E, Total Body Involvement. In: Helen Horstmann, Eugene BleckOrthopaedic Management in Cerebral Palsy 2007 2nd edLondonMac Keith Press [Google Scholar]
[7]. Cooper J, Majnemer A, Rosenblatt B, Birnbaum R, The determination of sensory deficits in children with hemiplegic cerebral palsyJ Child Neurol 1995 10(4):300-09.10.1177/0883073895010004127594266 [Google Scholar] [CrossRef] [PubMed]
[8]. Traughber BJ, Hodak JA, Mamourian AC, Radiological evaluation of craniovertebral junction. Section 1, chapter 4, figure 4.3, pg 85 In: Bambakidis NC, Dickman NA, Spetzler RF, Sonntag VKH, EditorsSurgery of the Craniovertebral Junction 2012 First edNew YorkThieme Medical Publishers [Google Scholar]
[9]. Lee JA, Wood MJ, An unusual form of occipitocervical assimilation presenting with spastic tetraparesis in a childPediatr Neurosurg 2010 46(2):146-50.10.1159/00031956020689346 [Google Scholar] [CrossRef] [PubMed]
[10]. Trabacca A, Dicuonzo F, Gennaro L, Palma M, Cacudi M, Losito L, Os odontoideum as a rare but possible complication in children with dyskinetic cerebral palsy: a clinical and neuroradiologic studyJ Child Neurol 2011 26(8):1021-25.10.1177/088307381039783521616925 [Google Scholar] [CrossRef] [PubMed]
[11]. Amess P, Chong WK, Kirkham FJ, Acquired spinal cord lesion associated with os odontoideum causing deterioration in dystonic cerebral palsy: case report and review of the literatureDev Med Child Neurol 1998 40(3):195-98.10.1111/j.1469-8749.1998.tb15447.x9566658 [Google Scholar] [CrossRef] [PubMed]
[12]. Weng MS, Haynes RJ, Flexion and extension cervical MRI in a pediatric populationJ Pediatr Orthop 1996 16(3):359-63.10.1097/01241398-199605000-00013 [Google Scholar] [CrossRef]