A Case of Severe Hyperkalemia Presenting with No Significant ECG Changes
Rasha Haykal1, Mohamed A. Youniss2, Mohamad Al Kateb3, Hale Z. Toklu4, Christopher L. Bray5
1 Internal Medicine Resident, University of Central Florida College of Medicine and North Florida Regional Medical Center, Fl, USA.
2 Internal Medicine Resident, University of Central Florida College of Medicine and North Florida Regional Medical Center, Fl, USA.
3 Internal Medicine Resident, University of Central Florida College of Medicine and North Florida Regional Medical Center, Fl, USA.
4 Research Director, University of Central Florida/ HCA Graduate Medical Education, Fl, USA.
5 Internal Medicine Residency Program Director, University of Central Florida College of Medicine and North Florida Regional Medical Center, Fl, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rasha Haykal, University of Central Florida College of Medicine, North Florida Regional Medical Center, Internal Medicine Residency Program, 6500 Newberry Rd. 32605 FL, USA.
E-mail: rasha.haykal@hcahealthcare.com
An increase in serum potassium levels is followed by progressively severe electrophysiological derangements in cardiac impulse generation and conduction, which are reflected in the electrocardiogram (ECG). Severe hyperkalemia with minimal or nonspecific ECG changes is unusual. Here we report a 69-year-old female who presented to our emergency department with hyperkalemia and was found to have no significant ECG changes.
Acute kidney injury, Chronic kidney disease, Hyperpotassaemia, Serum potassium, T waves
Case Report
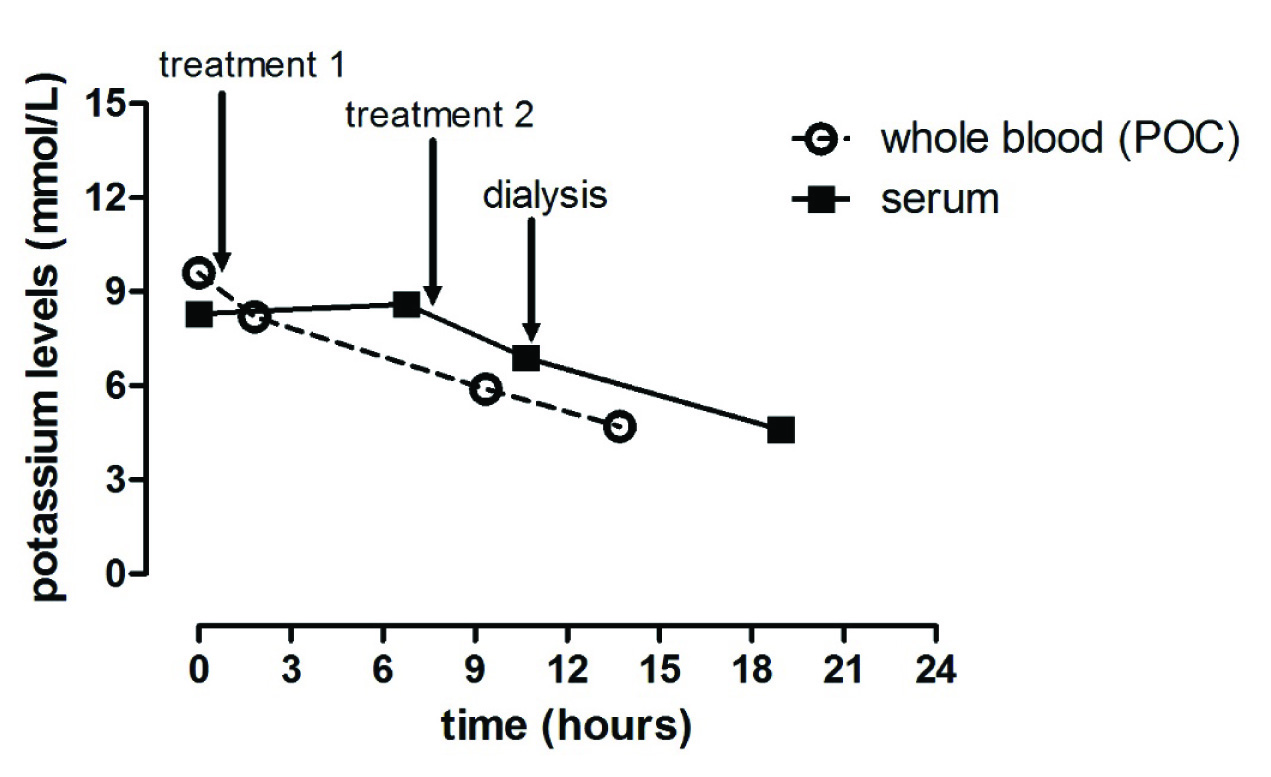
A 69-year-old African American female, presented to the Emergency Department (ED) for a non-traumatic, progressive, sharp lower back and right hip pain for 2 days. Her past medical history included hypertension, type 2 diabetes mellitus, hyperlipidemia, NYHA Class II congestive heart failure with preserved ejection fraction EF: 55-60% and chronic kidney disease stage 3 with a baseline BUN of 20 mg/dl and creatinine of 1.3 mg/dl. She received one dose of 60 mg IM ketorolac, 125 mg IM methylprednisolone and 4 mg IM morphine sulfate in the ED to control the pain and a basic evaluation including a Complete Blood Count (CBC), Comprehensive Metabolic Panel (CMP) and lumber and hip X-ray. The evaluation revealed Acute Kidney Injury (AKI) as evidenced by a sharp elevation of BUN to 51 mg/dl, creatinine to 2.1 mg/dl, further complicated by hyperkalemia to a critical level of 8.3 mmol/L in serum (Point-of-care potassium was >9 initially) [Table/Fig-1]. She had non-anion gap metabolic acidosis on intake with an ABG pH of 7.21. The patient also had proteinuria and haematuria [Table/Fig-2].
Complete blood count and blood chemistry.
| Haemogram | Levels | Normal range |
|---|
| WBC | 9.0 | (4.5 - 11.0 thou/mm3) |
| Neutrophils % | 85.4 | (50.0 - 75.0 %) |
| Lymphocytes % | 8.5 | (17.0 - 42.0 %) |
| Monocytes % | 4.6 | (4.0 - 11.0 %) |
| Eosinophils % | 0.7 | (0.4 - 6.0 %) |
| Basophils % | 1.1 | (0.0 - 2.0 %) |
| Absolute neutrophil count | 7.7 | (1.5-8.0 thousands/ mm3) |
| RBC | 3.23 | (3.80 - 5.20 million cells/uL) |
| Hb | 10.2 | (12.0 - 15.0 g/dL) |
| Hct | 31.3 | (35.0 - 49.0 %) |
| MCV | 96.7 | (80.0 - 100.0 fL) |
| MCH | 31.5 | (26.5 - 34.0 pg) |
| MCHC | 32.5 | (32.0 - 36.0 %) |
| RDW | 16.1 | (<17.0 %) |
| Platelet Count | 141 | (150 - 450 thousand/mm3) |
| MPV | 10.4 | (6.6 - 10.2 fL) |
| Chemistry | | |
| Sodium | 140 | (136 - 145 mmol/L) |
| Potassium | 8.3 | (3.5 - 5.1 mmol/L) |
| Chloride | 115 | (98 - 107 mmol/L) |
| Carbon Dioxide | 15 | (21 - 32 meq/L) |
| BUN | 51 | (7 - 18 mg/dL) |
| Creatinine | 2.10 | (0.60 - 1.30 mg/dL) |
| Estimated GFR (African American) | 28 | (=>90) |
| Glucose | 142 | (74 - 106 mg/dL) |
| Calcium | 8.8 | (8.5 - 10.1 mg/dL) |
| NT-Pro-BNP | 228 | (0 - 900 pg/mL) |
| Albumin | 2.7 | (3.4 – 5.0 g/dL |
| ABG pH | 7.21 | (7.35-7.45) |
| ABG pCO2 | 40 | (35-45) |
Abbreviations: WBC: White Blood Cell Count; RBC: Red Blood Cell Count; Hbg: Haemoglobin; Hct: Haematocrit; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Haemoglobin; MCHC: Mean Corpuscular Haemoglobin Concentration; RDW: Red Cell Distribution Width; MPV: Mean Platelet Volume; BUN: Blood Urea Nitrogen; GFR: Glomerular Filtration Rate; NT-Pro-BNP: N-Terminal Pro B-Type Natriuretic Peptide
| Color | Yellow |
|---|
| Appearance | Cloudy |
| PH | 5.0 |
| Specific Gravity | 1.017 |
| Protein | Trace high |
| Glucose | Negative |
| Ketones | Negative |
| Nitrate | Negative |
| Bilirubin | Negative |
| Urobilirubin | <1.0mg/dL |
| Leukocyte Esterase | Negative |
| White Blood Cell Count | 3-5WBC/hpf |
| Red blood cell Count | Too numerous to count |
| Hyaline Cast | Not seen |
| Epithelial Cells | Rare |
| Bacteria | Rare |
| Haemoglobin | Large High |
Reviewing the patient’s medication list [Table/Fig-3], she was on a furosemide 40 mg tablet daily, a potassium chloride 10 MEQ tablet daily, carvedilol 25 mg tablets BID, a valsartan 20 mg tablet daily, a spironolactone 25 mg tablet daily and metformin/sitagliptin 50-500 mg tablet daily. However, she stated that she has been off her medications for the preceding 5 days. Her ECG revealed a normal sinus rhythm [Table/Fig-4], P-R-T Axes: 066 050 064 degrees, PR interval 1.58 seconds, QRS 0.84 seconds and QT 324 ms/QTc 382 ms (rate 84). The T waves were not tall or tented. Despite negative EKG with a serum and capillary blood test consistent with hyperkalemia, treatment was initiated in our hospital as hyperkalemia protocol. The patient received an oral sodium polystyrene sulfonate suspension 60 mg and calcium gluconate IV push of 1gm, followed by another calcium gluconate IV push of 1 gm, sodium bicarbonate IV push of 25 MEQ, D50W IV push of 25 gm and regular insulin IV push of 5 units in the ED after a third test showed hyperkalemia of 8.2. Repeat potassium was 8.6 mmol/L 6 hours later. Treatment was repeated with sodium polystyrene sulfonate suspension per oral 60 mg, calcium gluconate IV push of 1 gm, sodium bicarbonate IV push of 50 MEQ, D50W IV push of 25 gm and regular insulin IV push of 10 units. Her potassium dropped to 6.9 mmol/l 3.5 hours later. Her medical treatment was supported with dialysis and potassium dropped further to 4.6 mmol/L [Table/Fig-5].
| Medication | Initiation |
|---|
| Furosemide 40 mg tablet daily | 6 Months ago |
| Spironolactone 25 mg tablet daily | 6 Months ago |
| Potassium chloride 10 MEQ tablet daily | 6 Months ago |
| Valsartan 20 mg tablet daily | 5 Months ago |
| Carvedilol 25 mg tablets BID | 5 Months ago |
| Metformin/Sitagliptin 50-500 mg tablet daily | 6 Months ago |
Initial ECG upon admission showing normal sinus rhythm with no peaking of the T waves.

The change of potassium levels over time. Time 0 is the first measurement when the patient was admitted to emergency department. Baseline value was measured >9 mmol/L with Point-Of-Care (POC) whole blood analysis. Pharmacological treatment was applied twice before the dialysis was initiated.
Discussion
It is well recognized that serum electrolyte changes cause electrophysiological changes in heart rhythm. In experimental studies; these manifestations are reflected in the ECG as a result of hyperkalemia [1,2]. These electrophysiological changes include the shortening of the QT interval, peaking of the T waves, QRS prolongation, shortening of the PR interval, reduction in amplitude of the P-wave, loss of sinoatrial conduction with onset of a wide-complex “sine-wave” ventricular rhythm and ultimately asystole [1]. On the other hand, severe hyperkalemia with minimal or nonspecific ECG changes is unusual [3-6]. Earlier studies suggested that potassium concentration above 7.6 mmol/L is associated with consistent ECG changes [7].
In a clinical study, the best sensitivities and specificities for predicting hyperkalemia were reported as 0.43 and 0.86, and the sensitivity for detecting potassium levels of more than 6.5 mmol/L was also found 0.62 which is considered to be relatively poor [8]. Consistently, Montague et al., also found that the sensitivity and specificity of ECG in diagnosing hyperkalemia was poor [6]. Typically, serum potassium levels higher than (≥8 mmol/L) are expected to be associated with the classic ECG manifestations [2]. However, there are contradictory reports in literature. Although rare, high levels of hyperkalemia (≥8 mmol/L) without any significant changes in ECG were reported [3-5]. The underlying mechanism for why some patients do not present ECG changes is unknown. Narula et al., speculated that the rate of rise in serum potassium may also influence the development of ECG changes [5]. Also, other metabolic conditions such as acidosis, hypoxia, hyponatremia, and hypocalcemia may increase sensitivity of the heart to hyperkalemia [1].
As mentioned earlier, serum potassium >7.0 mEq/L is associated with conduction abnormalities and bradycardia [2]. Despite severe hyperkalemia (>8.3mmol/L), no significant changes in ECG were observed in our patient. While it might be argued that the QT interval was shortened, this finding would not typically be identified as significant, especially when the QTc is regarded as normal. Moreover, some of the medications patient was taking such as furosemide and spironolactone are associated with QT alterations [9]. It should be noted that her QT was 340 (QTc 404) a year prior in the emergency department with a potassium level of 4.7. Notably, the patient had elevated serum creatinine (2 mg/dL) at the time of presentation. Latus et al., has reported a case whose serum potassium level was dramatically elevated (9.5 mmol/L) and ECG showed QRS with a ‘sine-wave’ pattern. Although this patient had AKI, her serum creatinine was measured at 0.4 mg/dl (normal range 0.5–1.2) [10]. Unlike their case, our patient had no significant changes in ECG in the setting of an elevated serum creatinine (2 mg/dL). Therefore, hyperkalemia resulting from acute on chronic renal impairment and metabolic acidosis may not always translate into ECG changes as has been previously noted in literature [2,11].
Conclusion
In conclusion, the present case shows that ECG changes may not always accompany severe changes in potassium levels. Further studies are needed to investigate the mechanisms between hyperkalemia and onset of ECG changes.
Abbreviations: WBC: White Blood Cell Count; RBC: Red Blood Cell Count; Hbg: Haemoglobin; Hct: Haematocrit; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Haemoglobin; MCHC: Mean Corpuscular Haemoglobin Concentration; RDW: Red Cell Distribution Width; MPV: Mean Platelet Volume; BUN: Blood Urea Nitrogen; GFR: Glomerular Filtration Rate; NT-Pro-BNP: N-Terminal Pro B-Type Natriuretic Peptide
[1]. Ettinger PO, Regan TJ, Oldewurtel HA, Hyperkalemia, cardiac conduction, and the electrocardiogram: A reviewAm Heart J 1974 88(3):360-71.10.1016/0002-8703(74)90473-6 [Google Scholar] [CrossRef]
[2]. Mount DB, Disorders of potassium balance. In: Brenner BM, editorBrenner and Rector’s The Kidney. 1 2016 10th edPhiladelphia, PAElsevier:570-600. [Google Scholar]
[3]. Khattak HK, Khalid S, Manzoor K, Stein PK, Recurrent life-threatening hyperkalemia without typical electrocardiographic changesJ Electrocardiol 2014 47(1):95-97.10.1016/j.jelectrocard.2013.07.01223973093 [Google Scholar] [CrossRef] [PubMed]
[4]. Martinez-Vea A, Bardaji A, Garcia C, Oliver JA, Severe hyperkalemia with minimal electrocardiographic manifestations: A report of seven casesJ Electrocardiol 1999 32(1):45-49.10.1016/S0022-0736(99)90020-1 [Google Scholar] [CrossRef]
[5]. Narula AS HA, Severe hyperkalemia with normal electrocardiogramIndian J Nephrol 2005 15(Supplement):S34-S36. [Google Scholar]
[6]. Montague BT, Ouellette JR, Buller GK, Retrospective review of the frequency of ECG changes in hyperkalemiaClin J Am Soc Nephrol 2008 3(2):324-30.10.2215/CJN.0461100718235147 [Google Scholar] [CrossRef] [PubMed]
[7]. Tarail R, Relation of abnormalities in concentration of serum potassium to electrocardiographic disturbancesAm J Med 1948 5(6):828-37.10.1016/0002-9343(48)90162-4 [Google Scholar] [CrossRef]
[8]. Wrenn KD, Slovis CM, Slovis BS, The ability of physicians to predict hyperkalemia from the ECGAnn Emerg Med 1991 20(11):1229-32.10.1016/S0196-0644(05)81476-3 [Google Scholar] [CrossRef]
[9]. Snitker S, Doerfler RM, Soliman EZ, Deo R, St Peter WL, Kramlik S, Association of QT-Prolonging medication use in CKD with electrocardiographic manifestationsClin J Am Soc Nephrol 2017 12(9):1409-17.10.2215/CJN.1299121628793999 [Google Scholar] [CrossRef] [PubMed]
[10]. Latus J, Braun N, Alscher MD, Kimmel M, Life-threatening hyperkalemia--an overlooked acute kidney injury with a serum creatinine rise in the ‘normal’ rangeBMJ Case Rep 2012 :bcr012012569110.1136/bcr.01.2012.569122605836 [Google Scholar] [CrossRef] [PubMed]
[11]. Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, The frequency of hyperkalemia and its significance in chronic kidney diseaseArch Intern Med 2009 169(12):1156-62.10.1001/archinternmed.2009.13219546417 [Google Scholar] [CrossRef] [PubMed]