The phenomenal advances in health technologies and drug development in the last half of the century have witnessed a steady improvement in the life expectancy. Consequently, there is an increase in the size of the elderly population throughout the world including India. The elderly population, aged >60 years, increased from 6.9% in 1992 to 7.7% in 2002 [1].
Medications are probably the single most important healthcare technology in preventing illness, disability, and death in the geriatric population [2]. With age, the risk of becoming ill increases and many elderly suffer from several diseases, making pharmacotherapy in the elderly a complicated task. Super-specialty services being a common place these days, the elderly people tend to consult different specialists and are frequently treated by several doctors simultaneously. Too often, illnesses in older people are misdiagnosed, overlooked, or dismissed as part of the normal ageing process, simply because health professionals are not trained to recognize how diseases and drugs affect seniors [3]. The process of prescribing a medication is complex and includes: deciding that a drug is indicated, choosing the best drug, determining a dose and schedule appropriate for the patient’s physiologic status, monitoring for effectiveness and toxicity, educating the patient about expected side effects, and indications for seeking consultation. Inappropriate drug prescribing in the elderly is also common as evidenced by numerous published reports [4-6] and criteria for defining inappropriate medications for the elderly have been developed [7,8]. The elderly are also more liable to show tendency to imperfect adherence to prescribed treatment, adverse drug reactions and drug interactions [9,10]. Drug Utilization Review (DUR) programmes have offered safeguards against inappropriate use of prescription drugs in the elderly [11].
Studies conducted on young individuals cannot always be extrapolated to older subjects, even with the use of detailed knowledge of applied geriatric pharmacology, pharmacoepidemiology and with the use of estimates of the changed therapeutic value of drugs because of other factors such as polymorbidity, polypharmacy, poor adherence to therapy and disability [12].
In resource-poor countries like India, it is likely that the elderly age group receives relatively scanty attention, in so far as medical care for chronic diseases they suffer is concerned. The cost of medical and pharmaceutical care has been escalating enormously, steadily increasing the Out-Of Pocket (OOP) spending on medicines thereby, making it ill-affordable to all patients in general, and it is possible that elderly population in India, are worst hit by this. With the obvious economic insecurity the average elderly Indians get confronted, their right-full access to medical and pharmaceutical care are probably denied. They tend to take recourse to over-the-counter medications more frequently. Further, in India with multiple alternative health care systems prevailing like Ayurveda, Homeopathy, Unani etc., the senior citizen may find solution to their health problems in these apparently more economic health care systems [13].
A careful scrutiny of contemporary literature reveals some published reports on medication use by the elderly Indians [14,15].
Against this backdrop, the present study was conceived to examine drug use habits of the elderly people and how the same is influenced by diverse factors. The current study made an attempt to study the appropriateness of drug prescribing, compliance, response to all prescribed treatments, hospitalization, adverse reactions (if any) and their management. Further, an endeavour was made to assess the indulgence to self medication and use of alternative and complementary medicines (ayurveda, homeopathy, unani etc.,) by elderly and assessed any changes noted due to impact of professional oversight. This will presumably find a new role for the clinical pharmacologists supplementing to the existing pharmaceutical care for the elderly. This would thereby bridge the gap, if any, in the existing pharmaceutical care for the senior citizens.
Thus, the broad objective of the study is to understand the challenges of pharmacotherapy in the elderly and to explore if expert oversight could address such challenges optimally.
Materials and Methods
A prospective, randomized, observational and interventional community based study was conducted in the Kolkata Municipality Corporation (KMC) at ward no. 44 under the supervision of Department of Clinical & Experimental Pharmacology, Calcutta School of Tropical Medicine, Kolkata from April 2013 to September 2014 (1½ years) after obtaining approval from Institutional Ethics Committee (CREC-STM 21/2013 dt.09.02.13). The particular ward was chosen because of its close proximity with the study centre. Elderly subjects (>60 yrs) of either sex residing ward no. 44 suffering from chronic ailment but not critically ill, ambulatory, willing to interact from time to time, well conversant in Bengali or Hindi language and agree to give written informed consent were recruited in the study. Others who failed to fulfill these criteria were excluded from the study.
A list of probable elderly subjects (n=96) residing in that area was collected from the local councillor’s office. They were interrogated at their residences with the help of a field staff provided from the councillor’s office. The field staff helped in identifying, introduction with the investigator and initiating the early sensitization of the potential study participants regarding purpose of their visit. The subjects were also interrogated at a government run dispensary run by a medically qualified doctor, located in the study site where they used to visit for their medical care free of cost.
Using online random number generator (www.random.org) [16], a simple randomization plan for this study was done for allocation of subjects into supervised (n=40) and unsupervised group (n=35). The intervention in this study refers to counselling, monitoring, time table charting and reinforcement of the study subjects. The supervised group received these interventions either direct or by telephonic conversations during the follow up period at an interval of two months i.e., total 7 visits including the screening visit [Table/Fig-1]. The unsupervised group was not intervened by any means during the whole study period and only follow up data were captured in the pre designed, validated questionnaire at above mentioned fixed intervals. The investigator never attempted to treat or modify the ongoing management of any subjects of either group provided by their respective physicians for their chronic ailments during the whole study period.
Flow chart of the study methodology.

The supervised group was further counselled regarding bad practice of self medication, potential hazards of unsupervised medications, problems of sudden discontinuation of prescribed medicines, how to cope with forgetfulness, provided time table charts for medicine intake, avoidance of simultaneous use of alternative medications, safe medicine storage practices, paying attention to expiry dates of medicines procured etc. Those who failed to contact the investigator after repeated attempts were declared dropout subjects in this study.
A 28 item predesigned, validated questionnaire was used to collect relevant data at baseline and subsequent followed up at every 2 month interval. At each intervention the detailed assessments were documented in the data collection form. Charlson Comorbidity Index (CCI) was used to compare the chronic illness of the subjects on either group by 17 clinical conditions as defined by Charlson [17]. Concomitant medication adherence was assessed by the 8-Item Morisky Medication Adherence Scale (MMAS-8) [18]. For assessing potential inappropriate medication in the elderly, 2012 AGS Beers Criteria [6] was used.
Statistical Analysis
Data analysis was done at the end of the study. Descriptive statistics was expressed in mean±SD, range and percentage. Data was analysed using standard statistical test as applicable for categorical and numerical variables with two tailed significance level of p < 0.05. Standard statistical software like Microsoft Office Excel 2007 and SPSS version 11.5 were used for analysis. Comparison between groups was done. In case of categorical variables by Chi-Square test and two sided Fischer exact test was used. Missing data due to dropouts from the study in either group was handled by Last Observation Carried Forward (LOCF) method.
Results
Altogether, 96 elderly subjects were screened, out of which 75 were selected according to inclusion/exclusion criteria and were randomized into supervised (n=40) and unsupervised (n=35) group residing at Ward No. 44 of Kolkata Municipality Corporation. Altogether 5 participants from the supervised group and 4 from the unsupervised group were lost to follow up.
The average age in the supervised group was 68.4±5.77 years and in the unsupervised group was 66.89±6.77 years out of which one third were female [Table/Fig-2].
Descriptive statistics for numerical demographic parameters in the study population.
| Demographic profile | Supervised Group(n=40) | Unsupervised Group (n=35) | p -value* |
|---|
| Age (years) Mean±SD | 68.4±5.77 | 66.89±6.77 | 0.171 |
| Sex (Male/Female) | 31/09 | 19/16 | 0.030 |
| Marital Status (Married/Others†) | 28/12 | 24/11 | 0.989 |
| No. of Family membersMean±SD | 2.93±1.83 | 3.74±1.73 | 0.050 |
| Educational statusUG/PGPrimary to HSUp to primaryRead & writeIlliterate | 1336117 | 953108 | 0.122 |
| Occupational statusGovt. EmployeePrivate EmployeeSelf-employedUnemployed | 104917 | 46817 | 0.05 |
| Average Monthly income(INR)No Income <1500 ≥1500 to <4000≥4000 to <7500≥7500 to <12000≥ 12000 | 1928110 | 175706 | 0.139 |
† Bachelor/unmarried/ divorcee * Chi-square test with level of significance (0.05) with degree of freedom (df=1)
The educational status of the subjects was variable with majority of them were either undergraduate/postgraduates or only able to read and write [Table/Fig-2]. Rest of the study populations were distributed in between these two groups i.e. up to primary and primary to higher secondary standards. One fifth of the study population (n=15, 15.20%) was illiterate.
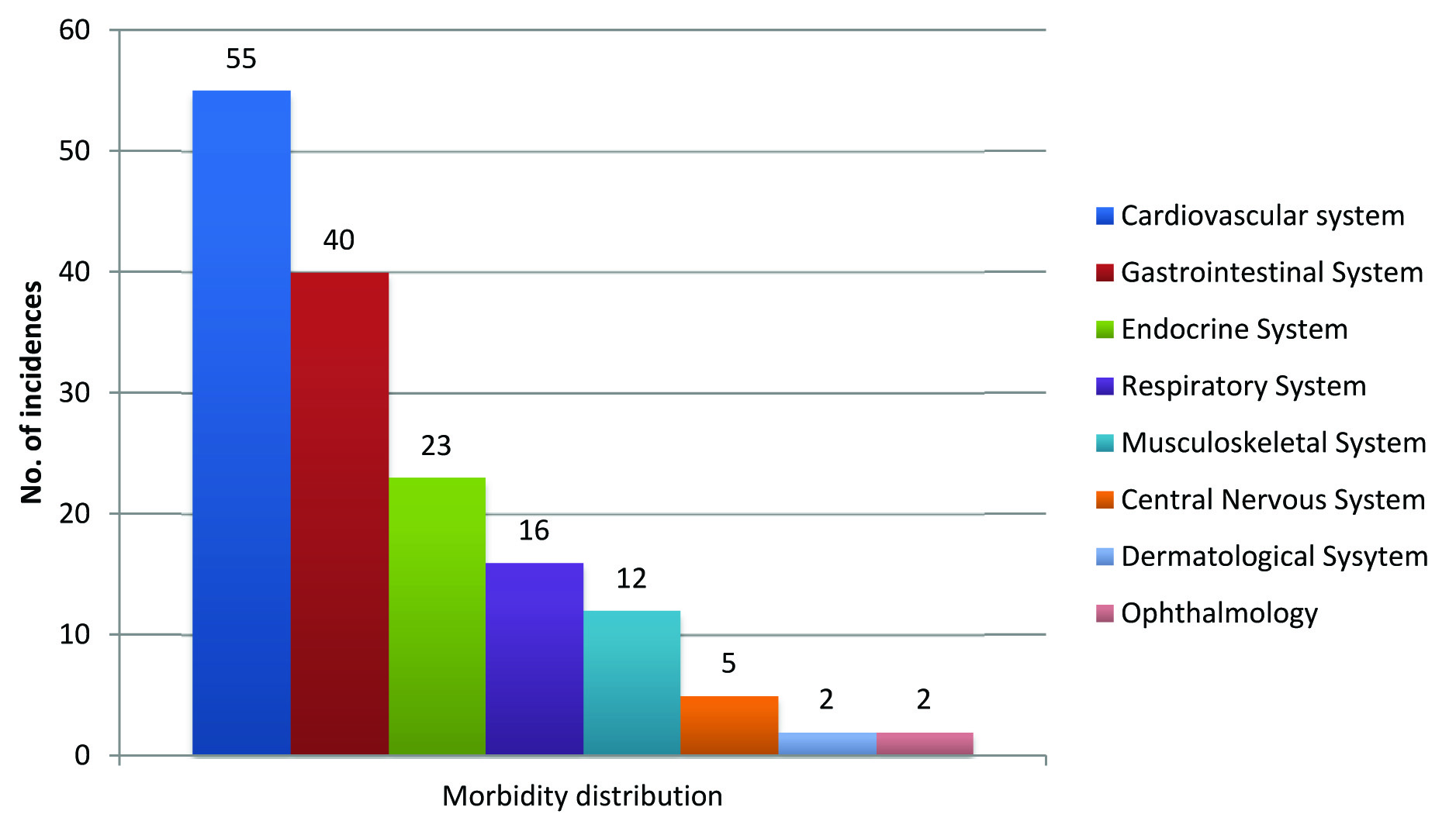
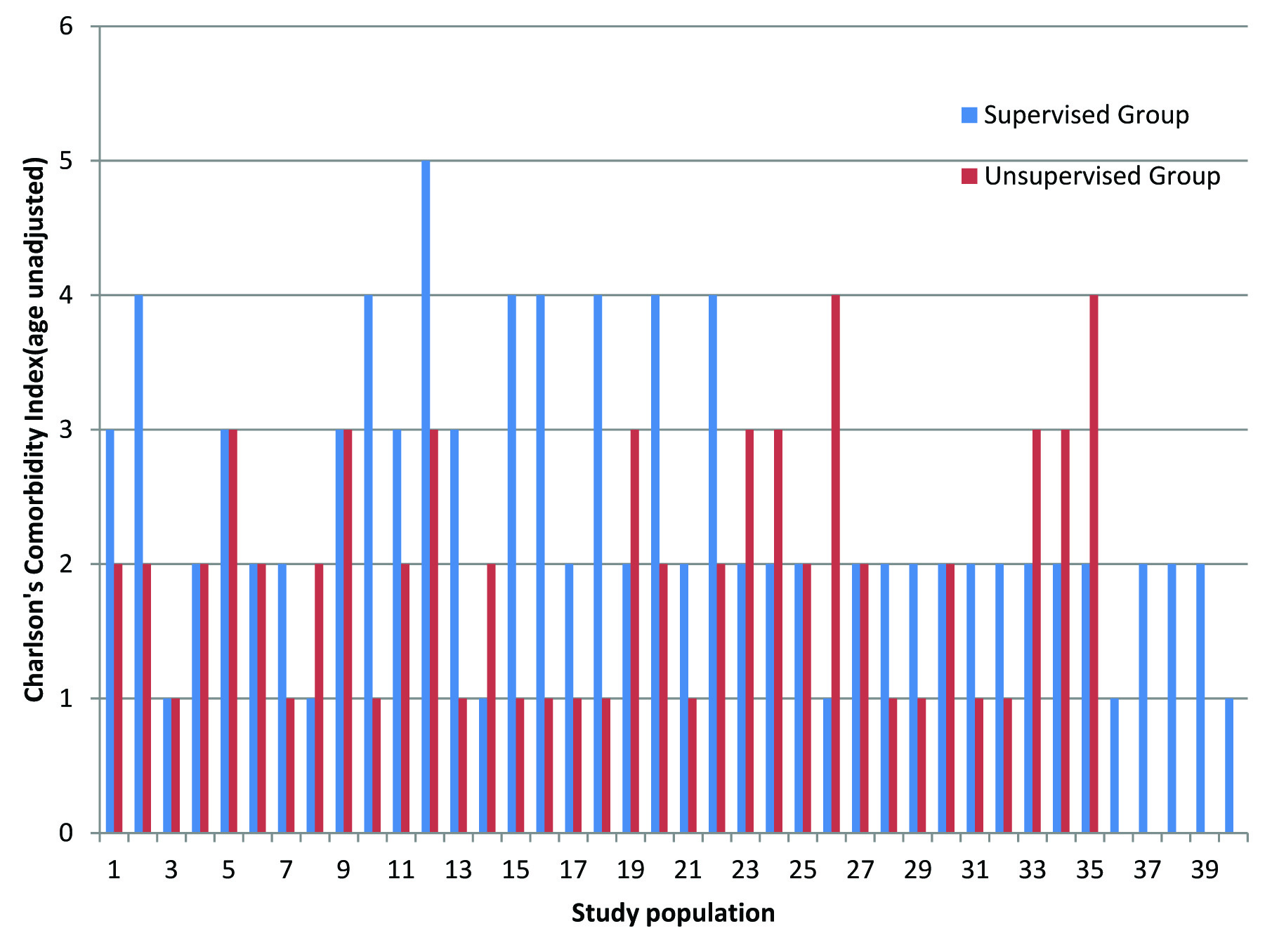
The morbidity pattern of the elderly subjects is shown in [Table/Fig-3]. Cardiovascular disorders like hypertension (n=55, 73.33%) followed by gastrointestinal disorders like hyperacidity (n=40, 53.33%) were the most common chronic illness of the study participants. The average CCI with age adjusted [Table/Fig-4] was found to be 2.40±1.03 for the supervised group and 1.97±0.93 for the unsupervised group which was not statistically significant (p = 0.06) indicating the chronic illness from which the study population suffered was fairly distributed in both the supervised and unsupervised group.
Morbidity pattern of the stuy population.
N.B: Total no. of incidences is more than the number of study subjects as there were multiple co morbidities among the participants
Charlson’s Comordity Index of the study population. (age unadjusted)
Many subjects in the study population were unemployed (45%) and the rest almost equally distributed among government, private or self employment [Table/Fig-2]. This was reflected in their earnings as many of them had either no or income less than Rs 1500.00 per month [Table/Fig-2].
The study population usually travelled the least possible distance (<1 km) to seek medical care. Patients who procured their medicines out of the pocket visited the pharmacy store at a frequency of once in a month. The average number of medicines per prescription in the supervised and unsupervised group was 3.27 and 3.05 respectively. The total number of fixed drug combinations prescribed in both the group was (n=27) comprising anti hypertensive and anti diabetic agents.
Prospective Self Medication
The study revealed that 45.33% (n=34) of the total subject did not practice any kind of self medication at all during the whole study period and took prescribed medicines only. In fact at the end of the study it was noted that the number of patients without self medication marginally increased in the supervised group and decreased in the unsupervised group when compared with the baseline data although statistically insignificant (p = 0.2999) [Table/Fig-5].
Subjects without self medications practices.
| Study Group | No. of subjects (%) | p-value* |
|---|
| Start of study | End of study |
|---|
| Supervised (n=40) | 17 (42.5) | 19 (47.5) | 0.2999 |
| Unsupervised (n=35) | 17 (48.5) | 14 (40) |
* Chi-square test with level of significance (0.05) with degree of freedom (df=1)
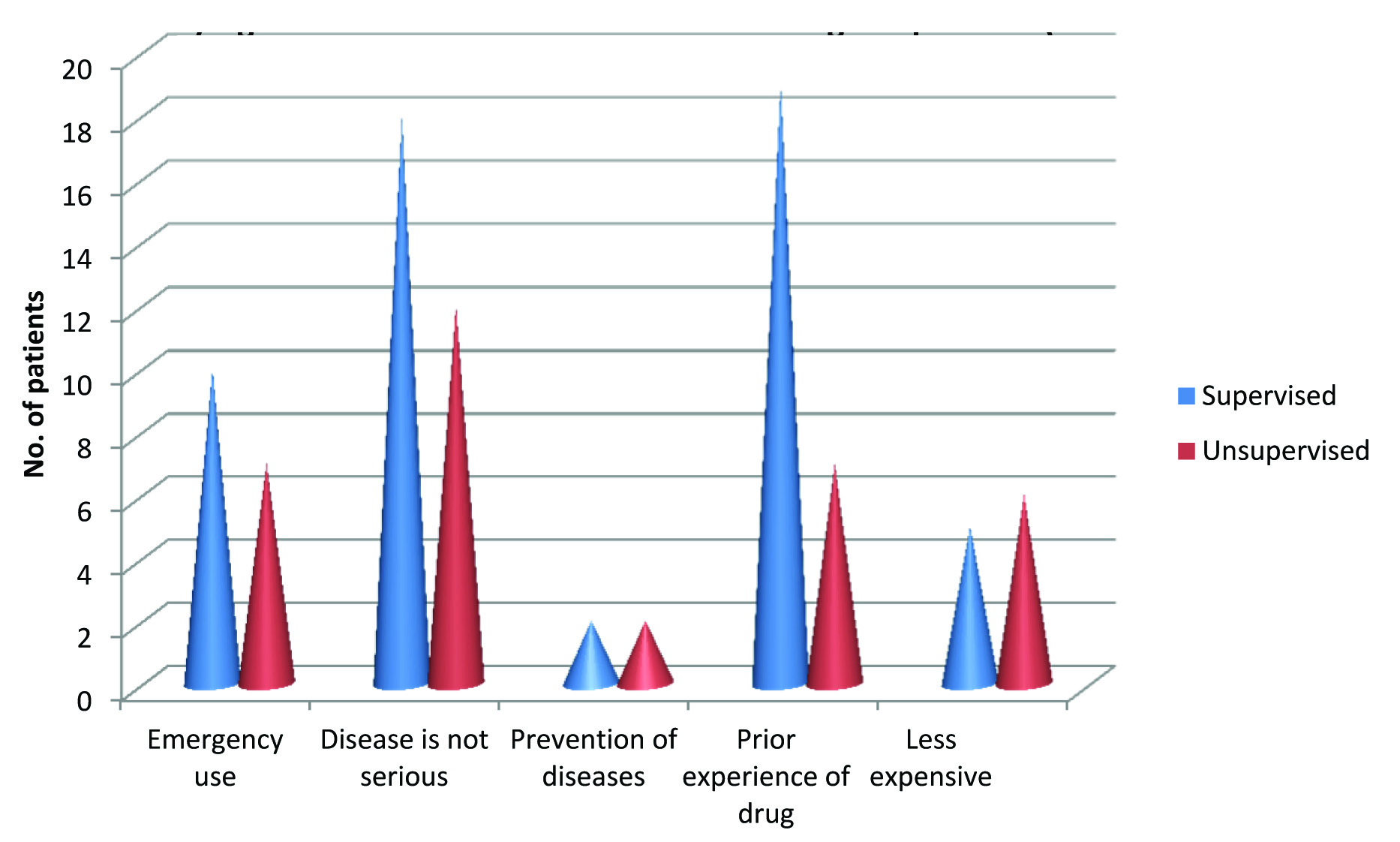
Most of the patients (n=21, 61.76%) who practiced self medication were suffering from gastrointestinal disorder (diarrhoea, heart burn) followed by fever/headache. A significant difference (p<0.002) was found regarding reasons for such self medication. In the supervised group, prior experience, followed by disease not so serious was cited for the most common issues whereas in the unsupervised group it was just the reverse [Table/Fig-6].
Reasons for self medications among the patients (at baseline).
Patients in either study group practice self medication after a waiting period of the first 24 hours after the onset of sign/symptom. One third of the patients were found to place their request at the pharmacy store telling symptoms of their illness followed by mentioning the name of the drug [Table/Fig-7].
Types of request placed by the patients indulging in self medication (at baseline).
| Study Group | Showing an old sample/package of the drug | Telling symptom of the illness | Mentioning the name of the drug | No such practices |
|---|
| Supervised (n=40) | 00 | 12 | 10 | 18 |
| Unsupervised (n=35) | 02 | 11 | 06 | 16 |
Analgesics/antipyretics were procured most frequently followed by drugs acting on gastrointestinal system (diarrhoea, heart burn etc.,) from over the counter.
The outcome of such self medication practice was found to prevent or improve their illness to some extent temporarily in most of the occasions without any incidence of complete cure of the disease ailment.
Compliance was a big challenge for the elderly subjects in both the group and the most common cause for not taking medicines at regular basis was forgetfulness (41.33%) followed by inconvenience of some sort in taking medicines (13.34%) [Table/Fig-8].
Reasons for irregular intake of medicines in the study population.
| Group | Feeling that it does not help | Dislike of taking medicines | Side effects | Forget-fulness | Incon-venience | Total (%) |
|---|
| Supervised(n=40) | 2 | 2 | 0 | 12 | 7 | 23(57.5) |
| Unsupervised (n=35) | 0 | 0 | 2 | 19 | 3 | 24(68.5) |
Only 18.66% of the subjects of either group missed their dose at a frequency of more than once per week followed by at least once per week (16%) at baseline. Around 40% in the supervised and 31.42% in the unsupervised group were well complaint with their treatment regimen as claimed. The number of patients without missing dose slightly improved in the supervised group and was statistically just significant (p = 0.023) [Table/Fig-9].
Subjects without missing any doses during the study period.
| Study Group | No. of subjects (Total) | p-value* |
|---|
| Start of study | End of study |
|---|
| Supervised | 16 (40) | 18(35) | 0.023 |
| Unsupervised | 11(35) | 10 (31) |
* Chi-square test with level of significance (0.05) with degree of freedom (df=1)
Once missing a dose, the common practice was to leave the missed dose and continue the rest as scheduled (n=31, 41.33%) followed by taking the missed as soon as remembered and then continuing the usual dosing schedule (n=19, 25.33%) in both the group.
Although majority of them (n=55, 73.33%) in both the groups avoided any alternative medications, only (n= 13, 18%) of the subjects used homeopathy followed by ayurvedic product mainly for arthritis and indigestion as concomitant medication. Reasons cited for such practices of alternative medicines were less expensive and with no or less side effects. The most common adverse effects due to prolonged medication reported by the subjects during the whole study period in both group were nausea (n=48, 64.4%), loss of appetite (n=14, 18.6%) and vertigo (n=6, 7.2%) with no other major complain. There were two incidences of hospitalization one each in the supervised and unsupervised group due to gastro intestinal tract infection and dyselectrolytemia respectively. In both the occasion the patient were hospitalized for 7 days. During this period the patient continued to take their usual regular medications prescribed by their treating physicians uninterruptedly as reported by them.
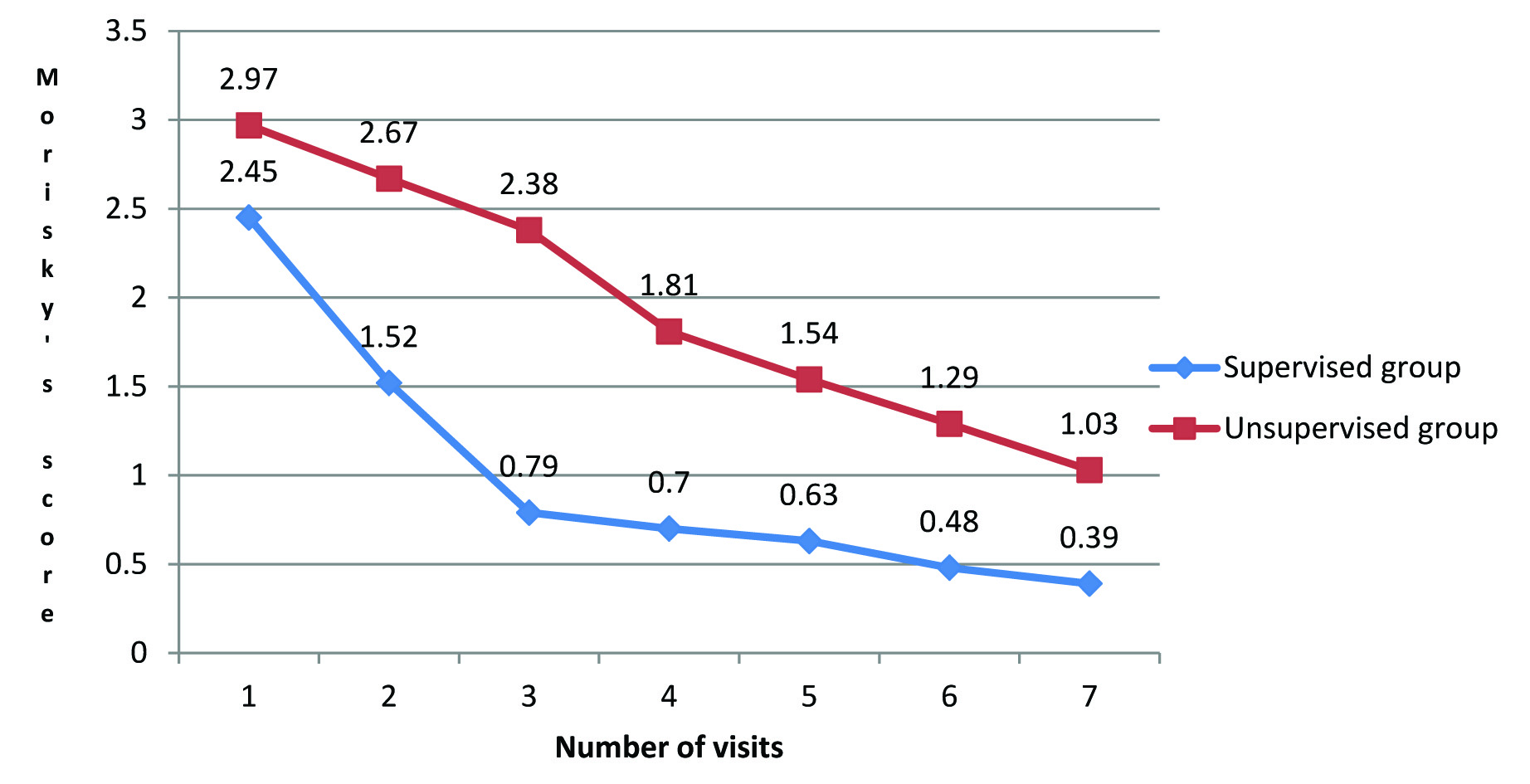
There was a statistical significant change in the Morisky’s 8 point Adherence Scale score (p<0.0001) between the supervised and unsupervised group when compared between baseline and end of study [Table/Fig-10]. The impact of supervision on medication adherence was evident.
Changes in Morisky’s score at different time interval in the study population.
Prior Knowledge about Drug
More than half of the subjects (53.33%) have no preference regarding formulation of drugs followed by tablet form (30.66%) due to convenience of intake and hassle free storage. Majority of the study subjects preferred to keep their medicines away from their children in one place separately. Most of the subjects in either group (74.66%) continued their medication with the advices of their physicians. Rest discontinued due to various reasons, with resolution of the intensity of the illness as the most common reson (63.15%).
When all the study subjects were asked regarding checking of expiry dates of the products during purchase or before consumption, almost 32% had a negative response. It was observed that the number of positive respondents increased to 100% in the supervised group and marginal improvement in the unsupervised group at the end of the study [Table/Fig-11].
Changes in the practice of checking expiry date of medicines.
| Group | Start of study | Group | End of study |
|---|
| Yes | No | Yes | No |
|---|
| Supervised (n=40) | 15 | 25 | Supervised (n=35)* | 35 | 0 |
| Unsupervised(n=35) | 12 | 23 | Unsupervised (n=31)* | 20 | 11 |
*Sample size decreased due to drop out of subjects at the end of the study
The average annual expenditure including physician’s fees and cost of medicines, laboratory investigations and indirect expenditure (if any) in the supervised group at base line and the end of study was Rs 5877.6±64 and Rs 6978.8±45 and in the unsupervised group it was Rs 6815.78±33 and Rs 8115.0±53 respectively. The increase in expenditure between baseline and end of study in both the group were statistically insignificant (p = 0.08).
According to 2012, AGS Beers Criteria, eight drugs were prescribed shown below [Table/Fig-12] identified as potentially inappropriate in the elderly patients in our study. Total number of patients received these inappropriate medicines were (n=25) distributed into (n=13) in the supervised group and (n=12) unsupervised group was respectively.
2012 AGS Beer’s Criteria for inappropriate medication in elderly patients.
| Category | Drug | Severity rating(QE-SR) * | Recommendation | No. of patients inSupervised Group | No. of patients inUnsupervisedGroup |
|---|
| Antiparkinsons agent | Trihexyphenidyl | QE: moderateSR: strong | Avoid | 1 | - |
| Cardiovascular | Digoxin (>0.125mg) | QE: moderateSR: strong | Avoid | 1 | 1 |
| TCA | Amitriptyline | QE: highSR: strong | Avoid | 1 | 1 |
| Benzodiazepines | Alprazolam | QE: highSR: strong | Avoid | 1 | - |
| Non- Benzodiazepines | Zolpidem | QE: moderateSR: strong | Avoid chronic use (>90 days) | 1 | - |
| Non COX selective NSAIDs (oral) | Diclofenac | QE: moderateSR: strong | Avoid chronic use unless other alternatives are not effective and patient can take gastroprotective agent (proton-pump inhibitor or misoprostol) | 2 | 4 |
| Ibuprofen | 5 | 5 |
| SSRI | Sertraline | QE: moderateSR: strong | With caution | 1 | 1 |
AGS: American Geriatric Society *(QE: Quality of evidence; SR: Strength of recommendation)
TCA: Tricyclic Antidepressants; SSRI: Selective Serotonin Reuptake Inhibitor;
COX: Cyclo oxygenase; NSAIDs: Non steroidal anti inflammatory drugs.
Most of the patients from either group continued these prescribed inappropriate medicines throughout the study as recommended by their treating physician except a patient from supervised group on oral zolpidem therapy discontinued it after 6 weeks of therapy. There was no as such appreciable impact of supervision on use of inappropriate medication during this study.
The most commonly prescribed drugs among the study participants are shown in [Table/Fig-13] along with their World Health Organization- Anatomical Chemical Therapeutic – Defined Daily Dose (WHO ATC-DDD) classification. Metformin, atorvastatin and ibuprofen were prescribed with lesser strength when compared to the WHO DDD recommendation. Such under dosing in the elderly patients might be justified on the basis of the average built of the Indian elderly subjects and their therapeutic requirements.
Some most frequently prescribed drugs and their ATC/DDD codes in the study population.
| Name of drug | No. of prescriptions | *ATC Code | WHO DDD measure (mg) | No. of DDDs |
|---|
| Amlodipine | 35 | C08CA01 | 5 | 33 |
| Metformin | 18 | A10BA02 | 2000 | 4 |
| Ranitidine | 13 | A02BA02 | 300 | 13 |
| Telmisartan | 12 | C09CA07 | 40 | 11 |
| Atorvastatin | 11 | C10AA05 | 20 | None |
| Ibuprofen | 10 | M01AE01 | 1200 | 2 |
| Theophylline | 10 | R03DA04 | 400 | 10 |
*WHO= World Health Organization, ATC= Anatomical Chemical Therapeutic, DDD = Defined Daily Dose
Discussion
The current study was undertaken on a small cohort of elderly subjects aged >60years of either sex residing in a small community in Kolkata to evaluate their drug use and medication management provided for their common chronic ailment by their treating physician and to find the impact of professional supervision, if any. The study revealed that most of these elderly subjects had only elementary formal education, were financially constrained, were married and suffered from cardiovascular and gastro intestinal disorders. The distribution of the severity of illness and predicted 10 year survival calculated by Carlsons Comorbidity index was comparable with other baseline demographic parameters in both the supervised and unsupervised group. Probably due to their chronic illness and decreased physical activity they tend to travel the minimum possible distance (<1km) to seek medical care mainly from a community dispensary run by state government as found in this study.
Similar to studies conducted earlier, where the self medication practices in the form of Over The Counter (OTC) varied from 50% [19] to 65% [20], the current study had 45.33% of the elderly subjects indulged in self medication. A mere 3% falls in self medication practice was observed in the supervised group and a rise of 8% was observed in the unsupervised group during this study. Problems like fever/headache, diarrhea, heartburn etc., were found to be common conditions for such self medication practices similar to findings in other studies [21,22]. The most common reasons cited behind the self medication decisions were an emergency situation, prior experience with the drugs and/or diseases and thought of not very serious health problem respectively. While all of the study participants procured the medicines from chemist’s shop, almost one third (33.66%) of them sought for a remedy by their narrated symptoms while (23.33%) of them directly named the drug they wanted to consume. Other knowledge regarding medicines like the dose, frequency, duration of treatment etc, was limited among the study subjects. Analgesics, antipyretics, anti peptic ulcers drugs were some common self medication products procured by the study participants similar to another study reported earlier [21]. The major outcome from those OTC encounters was unsatisfactory since there was little improvement in their illness with mere temporary resolution of problems.
Compliance remained a big challenge for the elderly patients on long term treatment with multiple drugs. Forgetfulness (41.33%) and inconvenience of some sort (13.34%) were cited as the most common cause behind non adherence with their treatment as found in several other studies [23,24]. Earlier it was published that notwithstanding the importance of patients’ proper self-administration of treatment, almost 50% of chronically ill older adults do not adhere to their prescribed medication regimens [25,26] and most health care providers are inattentive to patients’ pervasive low adherence.[27]..
The study revealed that a sizable proportion (n=25) i.e., 33.33% received inappropriate medications like Trihexyphenidyl, Digoxin, Amitriptyline, Alprazolam, Zolpidem, Diclofenac, Ibuprofen and Sertraline. Trihexyphenidyl (5mg once daily) was prescribed to a patient in the supervised group for the treatment of Parkinson’s disease. Studies conducted earlier suggests that since this drug has anticholinergic properties which may impair the cognitive function more in the elderly subjects and thus must be avoided [28].
One subject from each study group were found to consume digoxin (0.25 mg once daily) i.e., at a higher dose which was considered inappropriate according to AGS Beer’s criteria. The patient in the unsupervised group on digoxin (0.25mg once daily) left in the middle of the study and was lost to follow up.
Similarly amitriptyline (10mg once daily), a tricyclic antidepressant was prescribed for neuropathic pain to two study subjects in each group, with no untoward effects during the study period. Other studies revealed that amitryptiline is permitted in low dose for neuropathic pain and contraindicated as a antidepressant in the elderly [29].
Sertraline, an anti depressant was prescribed to one patient in each comparator group. Although, contrasting comments like increase in risk of fall in the vulnerable age group [30] as well as less depression in the elderly in short term regardless of medical co-morbidity status [31] were found in the earlier studies. This study revealed no untoward incidences during the entire follow up.
Apart from some common symptoms like occasional nausea, vertigo or loss of appetite there was no other significant adverse drug effect reported from the study population in either group. No such incidences of possible drug–drug interaction between prescribed and OTC or alternative medicine was reported from this study. The subjects were cautioned regarding the dangerous aspect of this medication and subsequently it was found to be withdrawn by his treating physician.
A significant finding of this study was that the majority of the elderly (73.33%) in either group didn’t practice any alternative medications. But other studies suggest that 60 to 80% of elderly consumers have declared the use of at least one herbal or nutritional medicine on a regular basis [32]. The rest of the elderly patients (26.66%) used either homeopathy or ayurvedic products for their ailment like arthritis and indigestion as these products were less expensive or having no/less side effects similar to a study conducted earlier [33].
Another significant outcome of this study was the increase in medication adherence (Morisky’s 8 point Adherence Scale score) in the supervised group due to continued supervision and follow up during the study period. It was clear that better communication among providers and patient-based interventions has a key role to enhance patient education, improves patients’ self treatment behaviours and skills, facilitates the identification and self-administration of patients’ medications and improves monitoring of their medication. Collectively, such influences affect older adults’ ability and willingness to take their medications. But in spite of these attempts there was no appreciable change in the practice of missing doses in both the group as patients was found to miss their doses at least once in a week during this study. Poor cognitive power might be the reason behind such outcome as a previous study indicates that poor cognition is associated with both over adherence and under adherence of a prescribed medication regimen [34-36] although no incidence of over adherence was noted in the present study. Unfortunately, few rigorously designed studies have been conducted to determine the effect of interventions to improve the medication-use process on patient outcomes [37] but such studies are needed critically [38].
Finally, it appears that learning with educational methods like oral and written formats in organized and logical order might be the most helpful for the older adults. Medication schedules or charts in combination with teaching or counselling enhances patient medication adherence and prevent frequent missing of the doses. Self medication though cannot be completely stopped but can be restricted with proper vigilance and supervision of the elderly subjects and that might control any possible drug induced adverse effects in future.
Limitation
For logistic reasons, the study was completed within one year time frame and thus done with a small sample size. The study site was not randomly chosen but based on the close proximity of the study centre. The demographic profile of the study population may not represent true population comprising of urban, rural and other social strata. The impact of other factors in the form of interventions like any advices and suggestions from treating doctors, family members and public media during the study period which might have influenced the outcome in both the study group was not analysed. Influence of media in the form of newsprint, television, radio on quality of medical care was not assessed during this study. Assessing self medication practice of hypnotics for insomnia which is common among the elderly was not incorporated in the questionnaire and thus creates further opportunities to study extensively in future. Although a set of questionnaire was used by the investigator towards all study population, they perhaps could not perceive the facts equally for which extra effort was made to their fullest satisfaction.
Conclusion
The present study concludes that supervision had an improved medication adherence with better compliance and improved quality of pharmaceutical care. The results of the present study undermine the need of further research to be conducted with larger population addressing properly the limitations of this study.
† Bachelor/unmarried/ divorcee * Chi-square test with level of significance (0.05) with degree of freedom (df=1)